1. Background
Definition of acute diarrhea is frequent (3 or more than 3 times per day), watery or semisolid fecal matter, for less than 14 days (1). This condition is one of the most common complaints of children referred to pediatricians (about 1.7 billion cases per year) and is the second cause of death (near 525,000 death per year) (2). Diarrhea is both preventable and treatable. Each year in many countries especially low-income countries, children experience 3 to 5 episodes of diarrhea. This event can cause malnutrition in this group of children. This is while malnutrition is a risk factor for childhood diarrhea.
The most important factors to prevent diarrhea include hand washing with soap, exclusive breastfeeding for the first six months of life, healthy food and drinking water, good personal hygiene and improved sanitation.
During diarrhea there is an increased loss of water and electrolytes in the stool so if these losses are not replaced adequately this may lead to development of electrolyte imbalance and metabolic acidosis and finally hypovolemic shock and end-organ damage (3).
Medical errors also play a prominent role in health care and the outcome of the patient’s illness. For this reason, focus on patient-safety in addition to emphasis on therapeutic protocols is important to prevent medical errors. Moreover, having a systematic and algorithmic approach, with clear definitions and step by step instructions, are useful for proper functioning and prevention of medical errors (4).
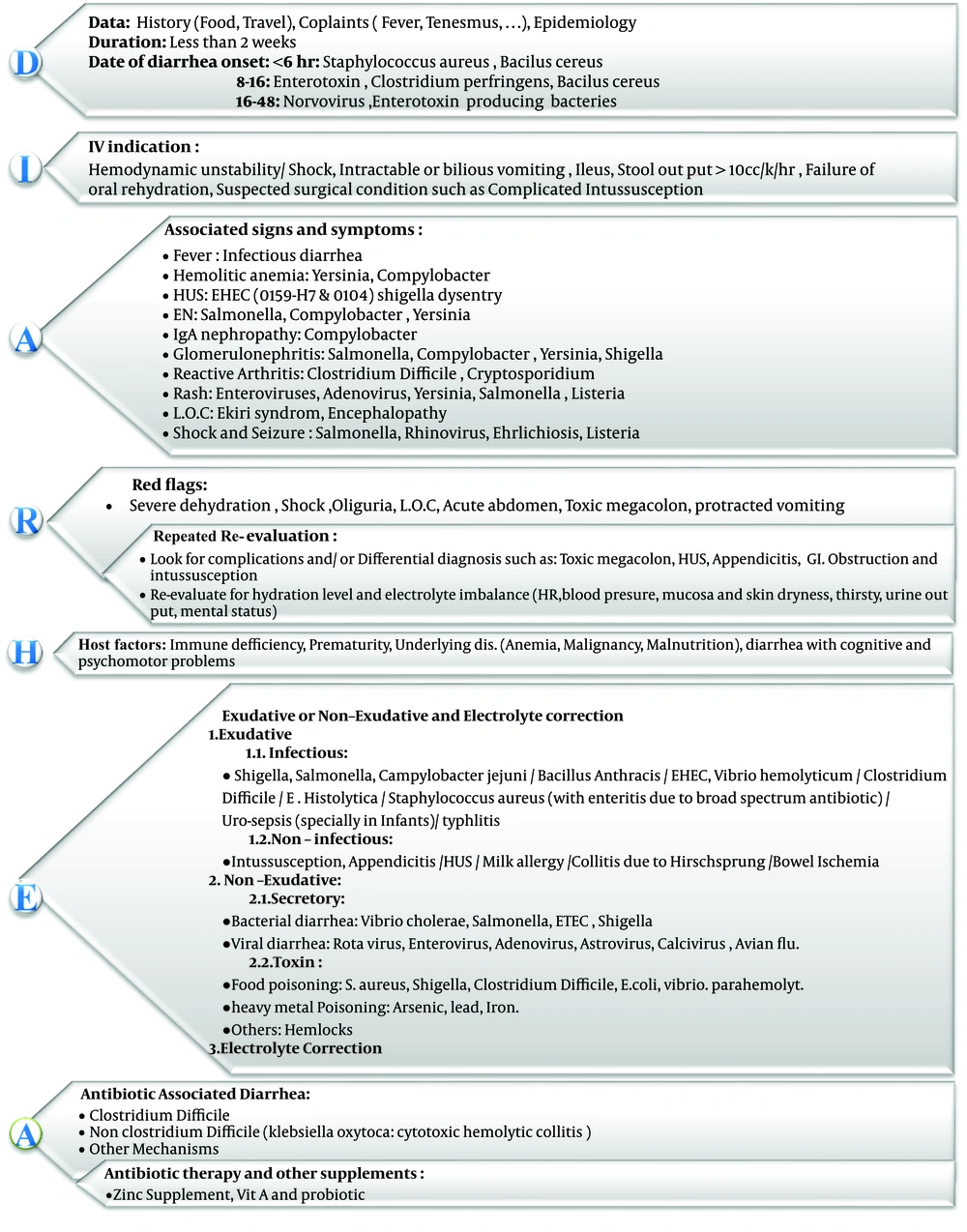
A punctual and complete history and physical exam are required to assess the patient with diarrhea and to do accurate and proper treatment (5). Given the importance of time and accuracy in approach to a patient’s problem, a new algorithmic approach will reduce the medical errors (human errors) due to lack of attention to red flags and principles of treatment. In this new algorithmic approach, the alphabetics that make up the word “DIARHEA” have been used to remember important points (Figure 1).
In the following, Figure 1 is explained in detail.
2. D (Data, Duration and Date)
Initially, a complete history of the patient including type and duration of diarrhea and other complaints such as fever, abdominal cramp, malaise and tenesmus should be asked. Also, pay attention to the incubation period (approximately 1 - 6 hours due to enterotoxin of bacillus cereus and Staphylococcus aureus, 8 - 16 hours due to diarrheal toxin of Clostridium perfringens and Bacillus cereus, 1 - 3 days due to Shigella spp., Salmonella spp., Enterotoxigenic E. coli (ETEC), Vibrio cholera and Yersinia enterocolitica) and the epidemiology of the region can be helpful in identifying the causative agent of bacterial or parasitic agents (6).
3. I (Intravenous (IV) Indication)
Although most children with dehydration can be successfully managed using Oral rehydration therapy (ORT), for various reasons intravenous (IV) therapy may be indicated. In children with unstable hemodynamic condition, hypovolemic shock, protracted vomiting, clinical suspicion of illeus or complicated Intussusception and stool output higher than 10 cc/k/h immediate IV therapy might be required.
4. A (Associated Signs and Symptoms)
In patients with diarrhea, some infectious pathogens are associated with some specific clinical features. For instance, in the vast majority of cases, acute gastroenteritis may be associated with fever. Fever in bacterial gastroenteritis may be higher.
In some cases of bacterial gastroenteritis (such as Yersinia, Campylobacter) hemolytic anemia may be seen. EHEC E. coli (0159-H7 and 0104) and Shigella dysenterie can cause Hemolytic-uremic syndrome (HUS), and so on, IgA nephropathy may be accompanied by Campylobacter, skin rash by Enteroviruses, Adenovirus, Yersinia, Salmonella, Listeria and reactive arthritis by clostridium difficile and cryptosporidium. Salmonella, Rhinovirus, Ehrlichia, Listeria can cause shock and seizure.
5. R (Red Flags)
In each patient with diarrhea, red flags should be taken into consideration and the patient should be examined for severe dehydration, protracted vomiting, shock, reduced urinary output, loss of consciousness (LOC), symptoms of acute abdomen and toxic megacolon.
5.1. Re-Evaluation
It is also necessary to re-evaluate patient regularly for hydration level (heart rate, blood pressure, mucosal dryness, prolonged capillary refill time, abnormal skin turgor, urine output and abnormal respiratory pattern and change in mental status) and electrolyte imbalance.
Regular assessment for complications or other comorbidities such as toxic megacolon, HUS, appendicitis, intussusception and gastrointestinal (GI) obstructions is also important (7).
6. H (Host Factors)
In the treatment of a patient with diarrhea some important host factors such as immune deficiency, prematurity, anemia, failure to thrive and association with cognitive and psychomotor problems should be considered and if necessary, the patient should receive special treatment for these conditions.
7. E (Exudative or Non-Exudative and Electrolyte Correction)
Some infectious or non- infectious conditions may be associated with exudative diarrhea. Infection with bacterial agents such as Shigella, Salmonella, Campylobacter jejuni, Bacillus anthracis, E. coli EHEC, Vibrio hemolyticumm, Entamoba histolytica and Clostridium difficile due to gastroenteritis and typhlitis in immunosuppressed patients can cause exudative diarrhea. On the other hand, intussusceptions, appendicitis, HUS, kidney disorders, milk allergy and bowel ischemia can induce exudative diarrhea and may mimic acute gastroenteritis.
Other bacterial agents such as Vibrio cholera, Salmonella, E. coli ETEC and Shigella or viral agents such as rotavirus, enterovirus, adenovirus, astrovirus, calcivirus and avian flu, as well as food poisoning or heavy metal poisoning can induce secretory diarrhea.
In patients with diarrhea particularly in secretory diarrhea, we should consider water and electrolyte imbalance (hypothermia, hypernatremia, hypercalemia and hypokalemia, acidosis and alkalosis) and should correct these biochemical disturbances as soon as diagnosis.
8. A (Antibiotic Associated Diarrhea)
Colitis due to previous antibiotic therapy with Clostridium difficile and Klebsiella oxytoca should not be forgotten. In these cases, bloody diarrhea can be confused with cytotoxic hemolytic colitis. In these cases, the prescribed antibiotic should be discontinued and special treatment for antibiotic associated diarrhea should begin.
8.1. Antibiotic Therapy and Other Supplements
Antibiotics should be considered in infants younger than 3 months of age with suspicion of a bacterial infection and older children with bloody diarrhea, fever, abdominal pain and dysentery due to probable Shigella and also in children who have chronic conditions or specific risk factors such as immunosuppression with dysentery (frequent scant bloody stools, fever, abdominal cramps, tenesmus) (8, 9).
According to results of studies, in cases of gastroenteritis, zinc supplements and probiotics are associated with reduction in stool volume and reduce the duration of diarrhea (10).
9. Conclusions
According to several guidelines and our experiences in Iran we suggest the alphabetic clinical algorithm for evaluation, diagnosis and treatment of infants and children whit acute diarrhea. In recent years, many of the recommended treatments, such as oral rehydration therapy (ORT) and zinc supplementation, have made a significant contribution to reducing mortality and morbidity from diarrhea but delay in diagnosis and treating specific conditions can cause severe complications and prolong the duration of disease (11). The new algorithmic approach, in addition to considering proper management of patients with diarrhea, will reduce the medical errors (human errors) due to lack of attention to red flags and principles of treatment.