1. Background
Various aspects of the diagnosis of hydatid cyst of the liver (HCL) remain relevant in pediatric practice (1). In the literature on children’s specialties, there are very few studies on the specificity and sensitivity of different approaches to the diagnosis of HCL in children, according to the stage of the parasite’s life cycle (2, 3). Unlike in adult practice where diagnostic algorithms are widely used, there are limited studies on the early diagnosis of HCL in pediatric practice (4).
2. Objectives
We sought to determine the effectiveness of various diagnostic methods of HCL in children, depending on the stage of parasitic activity.
3. Methods
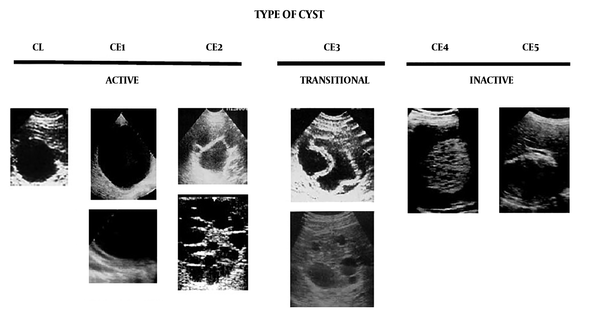
From January 4, 2005 to December 28, 2018, a total 93 children were admitted with isolated form of HCL of type CL-CE2 and with cyst size > 2 cm. There were 61 boys and 32 girls, with average age 9.1 ± 1.8 (3 - 17) years. Patients underwent clinical examination with laboratory diagnostics; serological testing using ELISA with an Echinococcus-IgG-ELISA-BEST reagent kit (D-3356; VECTOR-BEST, Russia); and Doppler ultrasound (US) examination of the abdominal organs using an ARIETTA V60 device (Hitachi Aloka Medical Ltd., Japan) with four linear and convex transducers of 3.5 and 5 MHz. To interpret the US data, we used the international classification of ultrasound images of HCL, approved by the World Health Organization for echinococcosis (5) (Figure 1). Patients were divided into groups, depending on the type of HCL: Group I (CL type) with 27 patients, Group II (CE1 type) with 32, and Group III (CE2 type) with 34.
Types of HCL which be found on US examination (5)
To determine the diagnostic value of clinical and laboratory follow-up, we included 61 patients with nonparasitic congenital and acquired cysts (comparison group).
Surgery and postoperative immunohistochemistry are definitive methods of determining the type of cyst. Surgical treatment was performed for all patients. Laparoscopic echinoccectomy with intraoperative evaluation of parasitic activity was performed in patients with HCL (6). A liver resection with cyst was performed in children with nonparasitic cysts.
The Ethics Committee of Stavropol State Medical University approved the study, and informed consent was obtained from the parents of all patients, as their legal representatives.
We determined the coefficients of sensitivity (Se) and specificity (Sp) were determined (7). Clinical and laboratory follow-up are designated true positive (TP), false negative (FN), false positive (FP), and true negative (TN), and we calculated Se and Sp as follows:
The Student t-test and χ2 test were used for statistical analyses with Statistica V. 10.0 (StatSoft, USA). A P value of < 0.05 was considered to indicate statistical significance.
4. Results
When attending our clinic, patients had the following clinical signs: pain in the right hypochondrium, 64 (41.6%) patients; enlarged liver, 59 (38.3%); enlarged abdomen, 44 (28.6%); loss of appetite, 37 (24.0%); weakness, 32 (20.8%); nausea, 23 (14.9%); dry skin, 27 (17.5%); pruritus, 31 (20.1%); and sleep disturbance, 16 (10.4%). Positive clinical criteria were considered one local sign or symptom together with one systemic sign or symptom. Evaluation of clinical manifestations of HCL showed Se = 49.2% and Sp = 27.6%. All patients with CL-type cysts had a negative ELISA result; in patients with CE1, 11 (34.4%) had a positive result; in those with CE2, 19 (55.9%) patients had a positive ELISA result. Conducting ELISA in children with echinococcosis had a low diagnostic value (Se = 16.4% and Sp = 28.8%). US with CL had high diagnostic value in 21 (77.7%) children, 29 (90.6%) with CE1, and 34 (100%) with CE2. We found a high US success rate, with Se = 91.1% and Sp = 92.3% (Table 1).
| Parasite Stage (N = 93) | Clinical Manifestations | Ultrasound Imaginga | ELISA | Reliability Index | |
|---|---|---|---|---|---|
| Abs (%) | Abs (%) | Abs (%) | χ2 | P | |
| CL (n = 27) | 10 (37.0) | 21 (77.7) | 0 (0) | 21.306 | 0.00 |
| CE1 (n = 32) | 15 (46.9) | 29 (90.6) | 11 (34.4) | 14.00 | 0.00 |
| CE2 (n = 34) | 26 (76.5) | 34 (100) | 19 (55.9) | 13.071 | 0.001 |
| Total | 44 (46.5) | 84 (90.3) | 30 (32.2) | 45.088 | 0.00 |
| Sensitivity | 49.2% | 91.1% | 16.4% | ||
| Specificity | 27.6% | 92.3% | 28.8% | ||
| χ2 | 2.751 | 4.312 | 7.187 | ||
| P | 0.253 | 0.116 | 0.028 | ||
Comparison of Various Diagnostic Methods of HCL
In assessing the Sp and Se of a combined diagnostic method with different types of cysts, the indicators increased from CL to CE2 types. ELISA diagnostics showed Se = 30.2% and Sp = 23.8%. Clinical manifestations combined with US and ELISA yielded Se = 59.8% and Sp = 47.5%.
In determining the Sp and Se of combined diagnostic methods (clinical manifestations with US and ELISA) for different types of HCL, we found that for CL-type cysts, these methods had Se = 51.0% and Sp = 53.6%; for CE1 cysts, these values were Se = 65.0% and Sp = 69.2%; for CE2-type cysts, these methods yielded Se = 84.4% and Sp = 89.3%. The Sp and the Se of clinical manifestations together with US and ELISA for CE2-type cysts were significantly higher (P < 0.05) than the values for CL and CE1. An integrated approach can provide reliable detection of echinococcosis at any stage of the parasite’s life cycle (χ2 = 7.973, P = 0.019). The Sp and Se of both clinical manifestations and serology were statistically improved in patients with CE2-type lesions compared with CL and CE1, which did not show any increase in Sp and Se.
5. Discussion
Previous investigations (1) have emphasized that US is an effective method for visualizing HCL (Se 80% - 99%, Sp 60% - 97%) with active cysts (CE2 - CE5). Serological methods for the diagnosis of HCL have a high Se (38% - 93%) and Sp (80% - 100%). A meta-analysis conducted by Iranian researchers of the incidence of echinococcosis, based on seropositivity, showed that 6.0% of the total population is infected and the above method is specific for HCL, with Sp 95.1% (8). Previous authors have also identified US as the most sensitive method for diagnosing HCL of types CE3 - CE5, with Se 97.6% and Sp 99%; these authors also emphasize that US is sensitive and specific for determining HCL types CL and CE1 - CE3 in children (6). In our work, the data obtained were comparable to the abovementioned studies. However, our results remain to be confirmed in integrated studies among children with HCL.
In summary, the effectiveness of HCL diagnosis in children with isolated and combined liver damage increased from CL to CE2 types. The most informative diagnostic method for all types of HCL is a comprehensive approach, taking into account clinical manifestations together with ELISA and US.