1. Context
Coronavirus disease 2019 (COVID-19) is an emerging disease that has been associated with a rapid increase in afflicted cases and deaths since its first diagnosis in Wuhan, China, in December 2019 (1). Since December 2019, the outbreak of COVID-19 has become a major epidemic threat in China. Since February 11, 2020, the cumulative number of confirmed cases in mainland China has reached 38,800 of which, 4,740 persons have recovered and 1,113 persons have died (2). After emerging in China, there has been an increase in the number and spread of the virus worldwide. On January 11, 2019, the World Health Organization (WHO) issued a statement declaring the spread of the new coronavirus to be the sixth major public health emergency worldwide to pose a threat to all countries (1, 3). On February 11, the new coronavirus disease (formerly called coronavirus 2019 (2019 (nCoV-19) received an official name from the WHO as coronavirus disease 19 (COVID-19). The International Committee has proposed the classification of the SARS-CoV-2 virus as the name of the virus causing COVID-19.7. (2) The Chinese National Health Commission has released a set of guidelines for the prevention, diagnosis, and treatment of COVID-19, based on the growing evidence of pathogens responsible for COVID-19 infection, as well as the epidemiological and clinical features (4). Following the pandemic crisis of the coronavirus disease in different parts of the world, the coronavirus epidemic in Iran was officially confirmed on February 5 (5). However, previously suspected cases of COVID-19 have also been reported from Iran (6). According to the Iran Ministry of Health and Medical Educatio’s Public Relations, by March 6, 14,991 patients with COVID-19 were identified in the country, of whom 853 persons died and 4,996 persons recovered (6). China and Italy had the highest numbers of casualties due to coronation (7) and Iran was third to these countries.
The cause of the outbreak of COVID-19 is still unknown. It is thought that person-to-person spread, similar to the outbreak of influenza and other respiratory pathogens, is caused mainly by respiratory droplets present in the affected person’s cough or sneeze (8). Limited information about COVID-19 is available during pregnancy. However, information on other diseases associated with highly pathogenic coronaviruses (e.g., acute respiratory syndrome (SARS) and Middle Eastern Respiratory syndrome (MERS)) may provide insight into the effects of COVID-19 during pregnancy. A spectrum of symptoms ranging from colds to severe respiratory illness and death are the main symptoms. Currently, the main epidemiological risk factors for COVID-19 include a travel history from China (especially Hubei Province) or close contact with infected persons within 14 days of symptom onset (8). It seems that given the widespread epidemic in countries such as Iran and Italy, these countries may also become high-risk epidemiological areas.
Coronavirus can spread from person to person without any symptoms (9). The data show that the average incubation period is about five days (range 2 to 14 days). The average age of patients is 56 - 49 years, with one-third to one-half of them having the underlying disease. The infection of children is rarely reported. Patient manifestations include fever, cough, myalgia, headache, diarrhea, and gastrointestinal symptoms. Paraclinical investigations include abnormal test results (including abnormal chest radiography, lymphopenia, leukopenia, and thrombocytopenia). Initial reports show that the acute respiratory distress syndrome (ARDS) occurs in 27% - 29% of hospitalized patients. The overall mortality rate appears to be 1%; however, new data may indicate a higher mortality rate (10). Various studies have shown that emerging infections have a significant impact on pregnant women and their fetuses (11). For example, some maternal and fetal complications increased with the emergence of the 2009 H1N1 influenza virus and the Zika virus (12, 13). In times of rapid outbreaks, which can have a significant impact on public health and medical infrastructure, the needs of pregnant women should be included in preparedness and response programs. In a similar outbreak, physicians have sometimes been reluctant to treat or vaccinate pregnant women, despite concerns about fetal safety (14). Since surveillance systems have been developed for COVID-19 cases, it is necessary to collect and report information on pregnancy status and maternal and fetal outcomes (10). The purpose of this study was to review and summarize the latest research on the management and treatment of women in pregnancy and childbirth worldwide and the management protocols available in Iran and other countries.
2. Evidence Acquisition
The present study aimed to review the literature related to the management of COVID-19 during pregnancy, childbirth, and postpartum and to provide valuable clinical evidence for the management of mothers afflicted with this virus from pregnancy to delivery. In this review, studies were performed by searching the Pubmed, Web of Science, UpToDate, SID, Scopus, Google Scholar, and medRxiv databases using keywords pregnant, pregnancy, gravidity, coronavirus, infection, COVID-19, and their Persian equivalents. There were no restrictions on language and history for access to full texts when collecting studies. The inclusion criteria were access to full text, human studies, published studies, or online access between December 2019 and March 18, 2020, when the final search was made (due to the emergence of the virus). Articles that were letters to the editor. The list of articles was evaluated in two stages. In stage one, the titles and abstracts of the articles were reviewed. in second stag, the full-text articles were reviewed according to the inclusion criteria. To prevent bias, two independent researchers performed the stages.
In total, 6,471 articles were extracted using the above-mentioned keywords. The initial search found at least two medRxiv articles and 15 guidelines, care guides, or recommendations. After reviewing and excluding duplicate and non-eligible articles, 12 articles and 11 guidelines and recommendations were reviewed. The search strategy is also annexed (Appendix 1 in Supplementary File). All study data were extracted based on the authors’ criteria, country of study, sample size, and the main findings. The initial draft was agreed upon by a specialist in perinatology working at a coronavirus hospital admission center.
3. Results
Based on the search strategy, a total of 12 articles and 11 instructions were extracted. The results of the review study were categorized according to the following: clinical course of COVID-19 in pregnancy, perinatal outcomes, neonatal outcomes, vertical transmission potential, management of coronavirus in pregnancy, labor, and delivery in women with COVID-19, postpartum stage in women with COVID-19, breastfeeding, and care for a baby born to a mother with COVID-19.
3.1. Clinical Course of COVID-19 in Pregnancy
Recent experiences with the Zika virus show that when a new pathogen emerges, the healthcare community must prepare for the worst-case scenario (15). Therefore, recommendations for the management of pregnant women at risk of SARS-CoV-2 immediate infection are needed (16). Pregnant women are susceptible to respiratory diseases and severe pneumonia, which may make them more susceptible than the general population to COVID-19 infection, especially if they have a chronic illness or maternal complications (4). There is currently no evidence of other severe coronavirus infections (SARS) or MERS indicating that pregnant women are more susceptible to coronavirus. The reported clinical features of pregnant women with confirmed COVID-19 infection are similar to those of non-pregnant adults with confirmed COVID-19 infection in the general population. Infection with COVID-19 represents a relatively optimistic clinical course compared to SARS-CoV infection (17, 18). However, a few published studies have examined the clinical course of infection in pregnant women. This indicates the need for further studies to more accurately assess the safety and health levels of pregnant women and newborns with COVID-19. So far, men have become more infected than women in the epidemic of the new coronavirus infection (19). Previous data on SARS and MERS suggest that clinical findings during pregnancy can range in symptoms from severe illness to death. In the study by Liu et al. (19), clinical symptoms were studied in 13 affected women. The results showed that clinical manifestations ranged from symptomatic to very severe and most pregnant patients had mild to moderate symptoms. Fever and fatigue were the main symptoms. The most common symptoms included sore throat and shortness of breath and almost all patients had a positive epidemiological history (traveling to high-risk areas) (19). Initial data from several hospitalized patients in China also show that up to 32% of people had severe pneumonia and 19% had ARDS. The mortality rate in these individuals was 1.4 to 4.3% (20, 21). Therefore, the most common symptom of COVID-19 is fever and cough, with more than 80% of hospitalized patients showing these symptoms. In the study by Chen et al. (22), the clinical course of nine women with COVID-19 during the third trimester of pregnancy was similar to that of other adults; the symptoms were fever (in seven patients), cough (in four patients), myalgia (in three patients), and sore throat and weakness (in two patients). Lymphopenia was present in three patients. All women had pneumonia, but none needed mechanical ventilation and none died. All nine women had cesarean sections. The neonatal Apgar score was 9 - 8 at the first minute and 10 - 9 at the fifth minute.
The study by Zhu et al. (23) was performed on nine pregnancies with 10 infants (one set of twins). The results showed that the onset of symptoms occurred before delivery (1 - 6 days) in four cases, the day of delivery in two cases, and after delivery (1 - 3 days) in three cases. The clinical manifestations in these women were similar to those of other non-pregnant women. Fetal intrauterine distress occurred in six cases. Cesarean delivery was performed in seven cases. Premature infants included five cases (10).
In a recent study published by Liu et al. (19), the results showed that five out of 13 patients underwent an emergency cesarean section due to pregnancy complications. These complications were fetal distress (in three of the 13 cases), premature rupture of the fetal membrane (in one of the 13 cases), and delivery (in one of the 13 cases). The condition of six patients deteriorated during hospitalization and led them to be admitted to the Intensive Care Unit (ICU) with MODS. The functional impairment syndrome included ARDS requiring intubation and mechanical ventilation, acute hepatic insufficiency, acute renal failure, and septic shock (19). In one case, the report of COVID-19 in pregnancy in Iran was as follows. The patient was a 27-year-old female, gravid one, with no history of the disease and with low risk-pregnancy of 36 weeks. The patient was admitted with fever, myalgia, and cough symptoms. She had less severe symptoms than two days before hospitalization. The next morning after admission, the patient suffered from hypoxemia, orthopenia, and shortness of breath. For this reason, the patient was transferred to the ICU. Because of the relative improvement of symptoms, the decision was made to terminate the pregnancy. For the induction of labor, oxytocin started and after successful labor, the mother experienced severe shortness of breath and hypoxemia at the time of crowning, which resulted in fetal heart rate decline. The mother had a cesarean section after intubation and died on the seventh day after the cesarean section due to respiratory distress (24). Therefore, based on limited reports and data from other respiratory pathogens such as SARS and influenza, it is unclear whether pregnant women with COVID-19 experience more severe disease.
Physiological changes in pulmonary function during pregnancy can increase the sensitivity and severity of pneumonia. Early studies have shown that pneumonia is associated with high perinatal mortality rates, thus requiring aggressive treatment including supportive measures with hydration, oxygen therapy, and chest physiotherapy (25). Ng et al. (25) performed the pathophysiological evaluation of the placenta of mothers with SARS7. The results indicated changes in the placenta that were most likely associated with abnormalities in maternal placental blood flow during hypoxic episodes of acute stages of their disease. Likewise, one of the main goals of managing pneumonia is to prevent and correct maternal hypoxia (10). Therefore, considering the complications of pregnancy and childbirth, strategies focusing on the prevention and management of COVID-19 infection should be considered for the management and treatment of the new coronavirus in pregnant women and newborns. On February 8, 2020, the National Health Commission of China presented a new protocol based on evidence from the latest studies and recommendations of experts, as well as previous experiences with SARS prevention and control (26). The protocol proposes to strengthen therapeutic counseling, screening, and follow-up of pregnant women. Visits should be as informal as possible. When referring pregnant women to gynecology clinics, quality in-person visits should be carried out using disinfectants and specialized protective clothing (4).
3.2. Perinatal Outcomes
There are very limited data on the risks associated with infection in the first and second trimesters of pregnancy. There are various data on the risk of congenital malformations associated with maternal fever. There is currently insufficient data on COVID-19 and the increased risk of miscarriage or congenital malformations. Available data from the SARS epidemic are reliable and indicate no increased risk of fetal loss and congenital malformations associated with early pregnancy infection (27). Given the limited data available on COVID-19 during pregnancy, the results of other respiratory viral infections may be helpful. For example, other respiratory viral infections during pregnancy, such as influenza, are associated with adverse neonatal outcomes, including low birth weight and preterm labor, which are generally due to severe maternal illness. In women with other coronavirus infections including SARS-CoV and MERS-CoV during pregnancy, observed perinatal complications included preterm delivery, intrauterine growth restriction, spontaneous abortion, infants with small for gestational age, young babies relative to gestational age, admitted to intensive care unit, kidney failure, and intravascular coagulation and release (28-30). Preterm delivery has been reported in infants born to women with COVID-19 during pregnancy. However, some cases appear to be iatrogenic and have not been spontaneous due to preterm labor. It is unclear whether these outcomes were related to maternal infection. All infants in this report were clinically good and no mortality was reported in infants (22, 24).
In a recent study published by Liu et al. (19), the results showed that five out of 13 patients underwent emergency cesarean sections due to pregnancy complications. These complications were fetal distress (in three of the 13 cases), premature rupture of the fetal membrane (in one of the 13 cases), and delivery (in one of the 13 cases); six (46%) of the 13 patients had preterm labor between 32 - 36 weeks of gestation (19). However, Zhu’s (23) study showed that maternal and neonatal side effects in pregnant women with COVID-19 infection were fewer than those with SARS-CoV-1 infection. There is no evidence of severe consequences for mothers and infants (31). These perinatal complications can be attributed to viral infection and physiological changes that reduce the woman’s intolerance to hypoxia in late pregnancy (32).
3.3. Neonatal Outcomes
The study by Chen et al. (22) was performed on nine infants born to affected mothers; all infants were born after 36 weeks of gestation and had no problems. Among the 10 infants born to affected mothers, 4 were full-term and 6 were born premature. There were two infants small for gestational age (SGA) and one infant large for gestational age (LGA). Eight were single pregnancy and two were twin pregnancy. Among infants born to mothers infected with CVV, six infants had a critical score (less than 90) in the pediatric system (PCIS). The most common clinical sign observed in these infants was shortness of breath (n = 6). Other symptoms observed were fever (n = 2), tachycardia (n = 1), and vomiting. The symptoms of the gastrointestinal tract seen in four patients were nutrition intolerance, bloating, refusal to breastfeed, and gastric bleeding. At admission, chest radiographs in seven infants were abnormal, including infection (n = 4), neonatal respiratory distress syndrome (n = 2), and pneumothorax (n = 1). Each infant received symptomatic supportive treatment after hospitalization. Two infants developed thrombocytopenia associated with abnormal liver function. One of the two babies was born at 34 + 5 weeks of gestation and was hospitalized 30 min after delivery for shortness of breath and moaning. Eight days later, he suffered from shock, cyanosis, multiple organ failure, and intravascular coagulation (DIC), which was treated with platelet transfer, suspended erythrocytes, and plasma. He died on the ninth day. The other baby was born at 34 + 6 weeks of gestation and was admitted 25 min after birth due to shortness of breath and moaning and discharged 15 days after supportive treatment. Overall neonatal outcomes were as follows: five infants were treated, one infant died, and four infants were hospitalized in stable condition. All infants had negative COVID-19 tests (23). Wang et al. reported a 30-week birth in good health (33). A study by Liu et al. reported a case of stillbirth and nine infants were born with the first minute Apgar score of 10 (19).
3.4. Vertical Transmission Potential
It is known that SARS-COV-2 is a new strain of coronavirus that is pathogenic to humans. The other two notable strains are SARS-CoV and the Middle East respiratory syndrome (MERS) coronavirus (MERS-CoV) (34). Homology modeling shows that SARS-CoV-2 has a structure with a receptor domain similar to SARS-CoV-1 (34-36). Therefore, the risk of COVID-19 vertical transmission may be as low as the SARS-CoV-1 transmission risk and COVID-19 infection has a pathogenicity similar to SARS-CoV-1 infection (4). Postnatal evaluation of newborns born to mothers with SARS and MERS did not identify cases of maternal transfer to the fetus. Media reports indicate that a 30-hour-old infant developed COVID-19, which may indicate the possibility of uterine transmission (37). However, there is insufficient information in media reports to rule out perinatal or postnatal stages. The studies by Chen et al. (22), Zhu et al. (23), and Wong et al. (29) found no evidence of SARS-CoV-2 viral particles in pregnancy products or in infants, these results are consistent with the findings of a previous study on SARS-CoV-1. The previous study was about SARS-CoV-1. Chen et al. (22) reported that in six patients of nine that amniotic fluid, cord blood, and neonatal throat swab were tested, were negative for SARS-CoV-2. So far, two cases of COVID-19 infection have been confirmed in infants. One case occurred 17 days after birth that had a history of close contact with her mother at birth. The other case was confirmed at 36 hours postpartum, with the possibility of a close relationship with the mother and a history of contact. However, no reliable evidence is yet available to support the direct transmission of COVID-19 from mother to baby (22). Liu et al. (19) also found no evidence of vertical transmission from the mother to the infant. Chen et al. (22) also found no evidence of COVID-19 intrauterine infection due to vertical transmission from mothers who had COVID-19 pneumonia in the third trimester. In this regard, it should be noted that all cases in this study underwent cesarean sections, so it is not possible to determine whether COVID-19 could be transmitted through vaginal delivery because no samples were taken from the vaginal mucosa. Previous studies demonstrated the possibility of maternal embryo transfer from human coronavirus (HCoV)-10 with evidence of the virus not only in maternal respiratory swabs but also in vaginal swabs (38). In this regard, Liu et al. (39) did not report the potential benefits of maternal and neonatal vertical transmission by examining the samples of three pregnant women including oral swabs, placental tissue, vaginal mucosa, breast milk, cord blood, and neonatal serum. Therefore, given the limitations of the reported studies, the most important goal during labor should be to reduce the exposure of infants to maternal body fluids (10).
3.5. New Corona Virus Management in Pregnancy
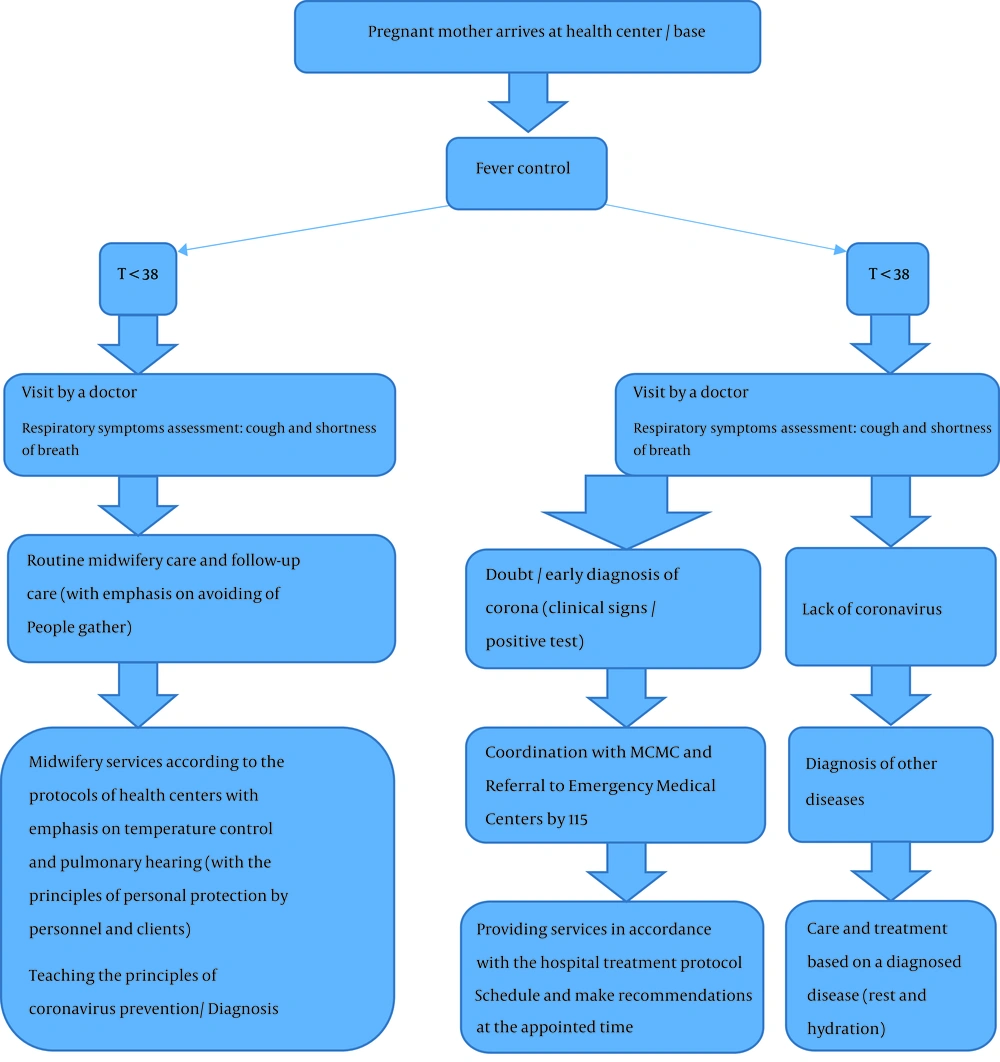
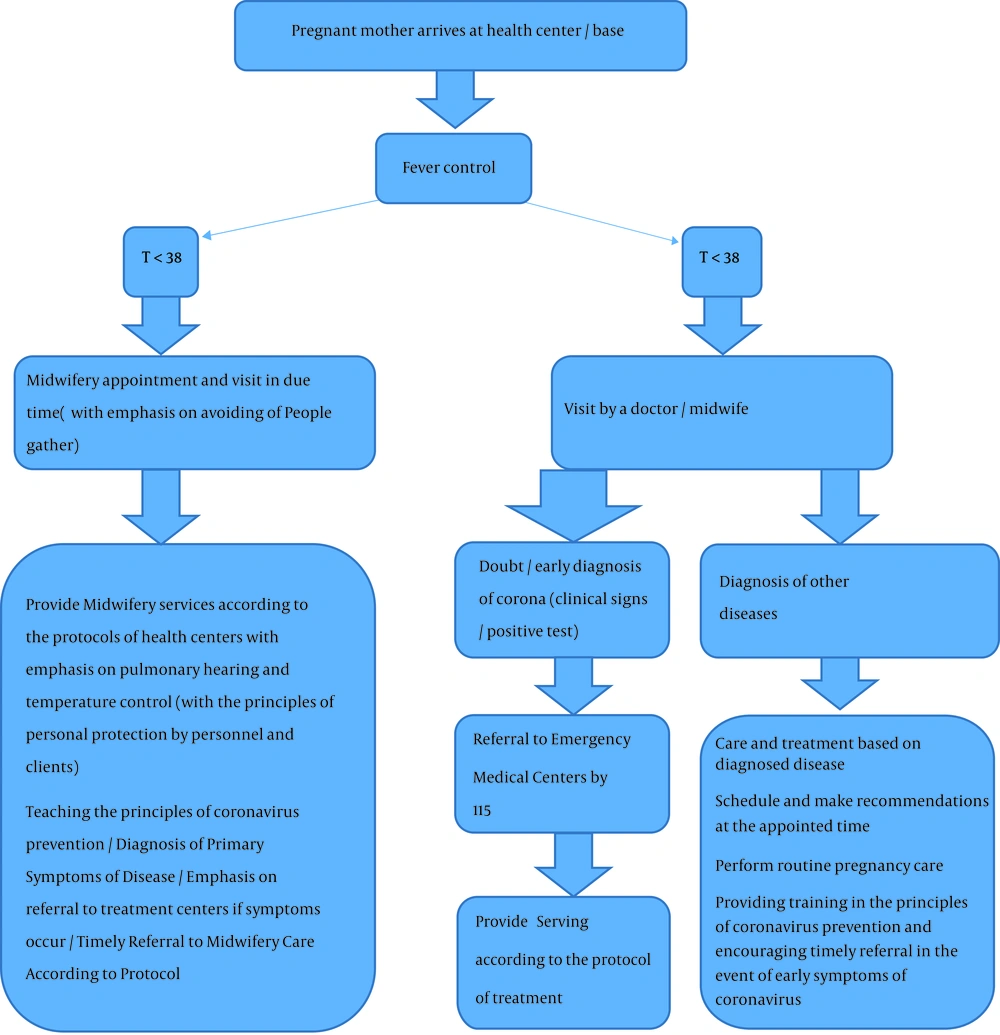
All patients, including pregnant women, should be evaluated for fever and respiratory infection symptoms. Ideally, screening begins before a pregnant woman enters a delivery ward or prenatal clinic. When scheduling appointments, the patient should be instructed not to have a face-to-face appointment on a designated day, or if the patient is contacted for triage before the appointment, she should be evaluated for respiratory and other symptoms via telephone. Patients with respiratory symptoms should be separated from other patients and they should use masks. Patients who meet the criteria for admission (Table 1) should be placed immediately in isolated rooms (single rooms under negative pressure). Health care personnel should use standard precautions (contact and air) (40) and perform necessary tests (upper and lower respiratory and serum specimens are currently recommended; other specimens, including stool and urine samples, may also be sent for analysis) (10). In this regard, the Ministry of Health reduced the number of routine care for low-risk pregnant women from eight to three. This is to reduce the traffic of pregnant mothers and decrease the mothers’ exposure to environmental contamination until disease control. It is also suggested that care be done by quality services (for optimal performance of care). Assessing thromboembolism and cardiomyopathy is done if needed. Mothers are advised to have adequate mobility and drink fluids. The monitoring of maternal status at intervals of care, test results, and ultrasound results should be done by telephone or SMS and referral to specialized levels be done if needed (41). General principles for managing COVID-10 during pregnancy include early separation, using aggressive infection control methods, SARS-CoV-2 and common infection tests, oxygen therapy if needed, preventing from fluid overload, starting empirical antibiotics (due to risk of secondary bacterial infection), fetal monitoring and uterine contraction, premature mechanical ventilation for progressive respiratory failure, planning for personal delivery, and team-based approach with multidisciplinary consultation (Table 2) (40). Favre et al. (16) proposed an algorithm. According to this algorithm, COVID-19 testing should be performed on all pregnant women who have traveled to countries affected by SARS-CoV-2 in the past 14 days (epidemiologically positive history) or have had contact with a patient with confirmed SARS-CoV-2 infection (42). Asymptomatic pregnant women with positive laboratory results for SARS-CoV-2, due to the clinical features of COVID-19, should be quarantined for at least 14 days at home (16). Maternal care processes in coronavirus have been presented by the Isfahan University of Medical Sciences regarding how to evaluate and manage pregnant women with suspected/positive viruses. Figures 1 and 2 presents the care for these mothers during pregnancy (43). The RCOG and RCPCH also provide a comprehensive guideline to care for women with COVID-19 during pregnancy, which is updated frequently. This guideline on prenatal care recommends that all mothers who are diagnosed with COVID-19 should be managed at appropriate maternal and newborn specialist centers and neonatal intensive care units (Table 2) (44). As the number of women with COVID-19 in pregnancy is increasing, it may be necessary to take care of women during pregnancy regionally and with a particular sensitivity for screening. It should be noted that the use of corticosteroids for the treatment of coronavirus pneumonia is not recommended unless there are other symptoms because the use of corticosteroids in MERS-induced pneumonia may not be beneficial and may even delay the recovery of MERS-CoV (45). The use of corticosteroids for fetal lung maturation should occur after consultation with infectious disease and perinatal specialists (44). In prenatal care, it should be advised to regularly consume 1000 D3 daily to the desired serum level (at least 50 nmol/mL) and frequent fluid intake (43). During acute illness, fetal management should be similar to other communicable diseases. Continuous monitoring of the fetus for severe diseases is recommended. For those who become ill at the end of pregnancy, ultrasound evaluation is considered to assess fetal growth in the third trimester (46). Because of the potential consequences of infection, fetal growth ultrasound and Doppler evaluation are performed bi-monthly for asymptomatic pregnant women and others who recover from mild disease (16).
| Epidemiological Risk | with | Clinical Features |
|---|---|---|
| Any person, including health care staff, who has had close contact with a laboratory-confirmed COVID-19 patient within 14 days of the symptom onset | with | Fever * or signs/symptoms of lower respiratory disease (e.g., cough or shortness of breath) |
| History of traveling to high-risk areas within 14 days of the symptom onset | with | Fever * and signs/symptoms of lower respiratory disease (e.g., cough or shortness of breath) |
| History of traveling to high-risk areas within 14 days of the symptom onset | with | Fever * and signs/symptoms of lower respiratory symptoms (e.g., cough or shortness of breath) requiring hospitalization |
| Row | General Principles |
|---|---|
| 1 | Patients with respiratory symptoms should cover their face with a mask and be ventilated separately and well at least six feet from other persons. |
| 2 | Confirmed and suspected cases of COVID-19 should be isolated as soon as possible in an isolated room (AIIR). |
| 3 | The CDC infection prevention and control measures should be taken for health care providers, including standard, contact, and air precautions. N95 eye protection and proper respiration should be used. |
| 4 | The staff should be provided with the proper use of personal protective equipment. |
| 5 | Training protective equipment (PPE) should be done including the correct method of landfilling. |
| 6 | Hospital infection control personnel should be contacted. |
| 7 | In coordination, relevant samples should be collected and sent for SARS-CoV-2 diagnostic testing. |
| 8 | Access to the room of confirmed or suspected patients should be restricted for visitors and healthcare personnel. |
| 9 | Pregnancy should be considered a dangerous situation. The fetal heart rate and uterine contractions should be checked. |
| 10 | For starters, oxygen therapy should be considered (for O2 saturation with a target of 95 and/or pO2 ≥ 70 mmHg). |
| 11 | Early mechanical ventilation should be considered with evidence of the progression of respiratory failure. |
| 12 | Non-invasive ventilation techniques may have a low risk of aspiration during pregnancy. |
| 13 | Intravenous fluids should be used conservatively unless the cardiovascular system is unstable. |
| 14 | Other viral respiratory infections and bacterial infections should be monitored (due to potential complications of infection). |
| 15 | Experimental antimicrobial therapy should be considered (because of the risk of other bacterial infections). |
| 16 | The experimental flu test should be taken, waiting for the results of the diagnostic test. |
| 17 | Corticosteroids should not be used frequently. |
| 18 | The use of steroids to enhance fetal lung maturation in individuals with anticipated preterm labor can be considered individually. |
| 19 | If septic shock is suspected, targeted management should be done quickly. |
| 20 | Decisions on childbirth and termination of pregnancy should be based on the age of the pregnancy, maternal status, fetal stability, and maternal wishes. |
| 21 | Gynecologists and perinatal, intensive care, anesthesia, and midwifery specialists should be consulted with. |
| 22 | Patients and their families should be talked about diagnosis and clinical status. |
3.6. Labor and Delivery in Women with COVID-19
In most cases, the timing of delivery should not be specified in case of COVID-19 infection. For infected women recovering early in pregnancy, no change in routine delivery is necessary. In the case of infected women recovering in the third trimester, it is reasonable to try to postpone childbirth (if no other medical indications arise). In general, COVID-19 infection itself is not a sign of labor (46).
The choice of the delivery time for pregnant women with confirmed infection should vary depending on gestational age, maternal, fetal, and delivery conditions (16). The decision to terminate a pregnancy based on maternal and fetal conditions must be made by a team. The termination of pregnancy after 37 weeks seems to be reasonable after the mother’s vital signs have stabilized (47). Vaginal delivery through induction of labor and instrumental vaginal delivery should be supported to prevent maternal fatigue and avoid unnecessary surgical complications in the patient. In the event of septic shock, acute organ failure, or fetal distress, a caesarean delivery (or legal termination of pregnancy) should be immediately prompted (16). Team-based management is proposed to manage suspicious and positive pregnancies for the virus. The team should include an optimized clinical unit that can provide the necessary care. It is necessary to provide supervision for the early detection of a pregnant mother’s disease and the ability to monitor the complications of labor (e.g., preterm delivery or fetal distress). Changes in the fetal heart rate pattern may be the first sign of maternal respiratory deterioration (40). The question of whether termination of pregnancy has benefits for the mother with the virus remains unclear. Therefore, decisions regarding childbirth should be based on the fetal gestational age and maternal status (48). According to the experience of SARS and MERS, severe respiratory failure may occur in pregnant women and in most severe cases, mechanical ventilation may not be sufficient to support oxygen delivery, in which limited studies indicate the potential role of ECMO in pregnancy (49). Table 3 lists the treatment recommendations applicable to pregnant women with the virus. The RCOG and RCPCH also have made recommendations for the care of women with COVID-19 at the stage of delivery and emphasized that a delay in cord closure (DCC) is not recommended (to reduce the risk of vertical transmission). Also, to reduce the transmission of the virus from the mother to the infant, secretions and blood from the baby’s body must be removed immediately (10, 44). The Isfahan University of Medical Sciences has provided midwifery recommendations in laboratories as part of care processes and has emphasized the following: No induction or augmentation of labor (oxytocin or syntocinon, misoprostol, etc.), applying techniques to reduce labor pain and emotional support of the mother by doula midwives in the care of each mother (one-to-one care for a pregnant mother and midwife and following LDR rules), disinfection of equipment and supplies by maternity services with the supervision of the infectious supervisor, considering negative pressure isolation rooms for safe delivery, continuous monitoring of the fetus in the labor process (due to the possibility of fetal distress), controlling the mother’s vital signs carefully and every hour, maternal respiratory monitoring, preventing the presence of anyone in the pregnant mother’s bedside, using upright, sitting, squatting, and lateral positions to reduce the duration of the two-stage labor, encouraging mothers to consume fluids to hydrate the mother and of course, not keeping the mouth dry in the case of a positive corona mother, no skin-to-skin contact between mother and infant, baby’s nasal suction before the first breath, isolating the infant immediately after birth, and performing a coronavirus test for the infant (43). Table 3 lists the most important treatment recommendations for pregnant women with COVID-19.
| Therapeutic Recommendations | References |
|---|---|
| Provide extra oxygen to maintain oxygen saturation above 95%. | (40) |
| Consider termination of pregnancy to improve maternal oxygenation. | (40) |
| If mechanical ventilation is required, keep pregnant patients in the left lateral position to maximize uterine blood flow. | (40) |
| Consider empirical antibiotics to prevent secondary bacterial infections. | (40) |
| Keep close and vigilant monitoring and timely interventions to minimize maternal hypoxia. | (10, 40) |
3.7. Postpartum Stage in Women with COVID-19
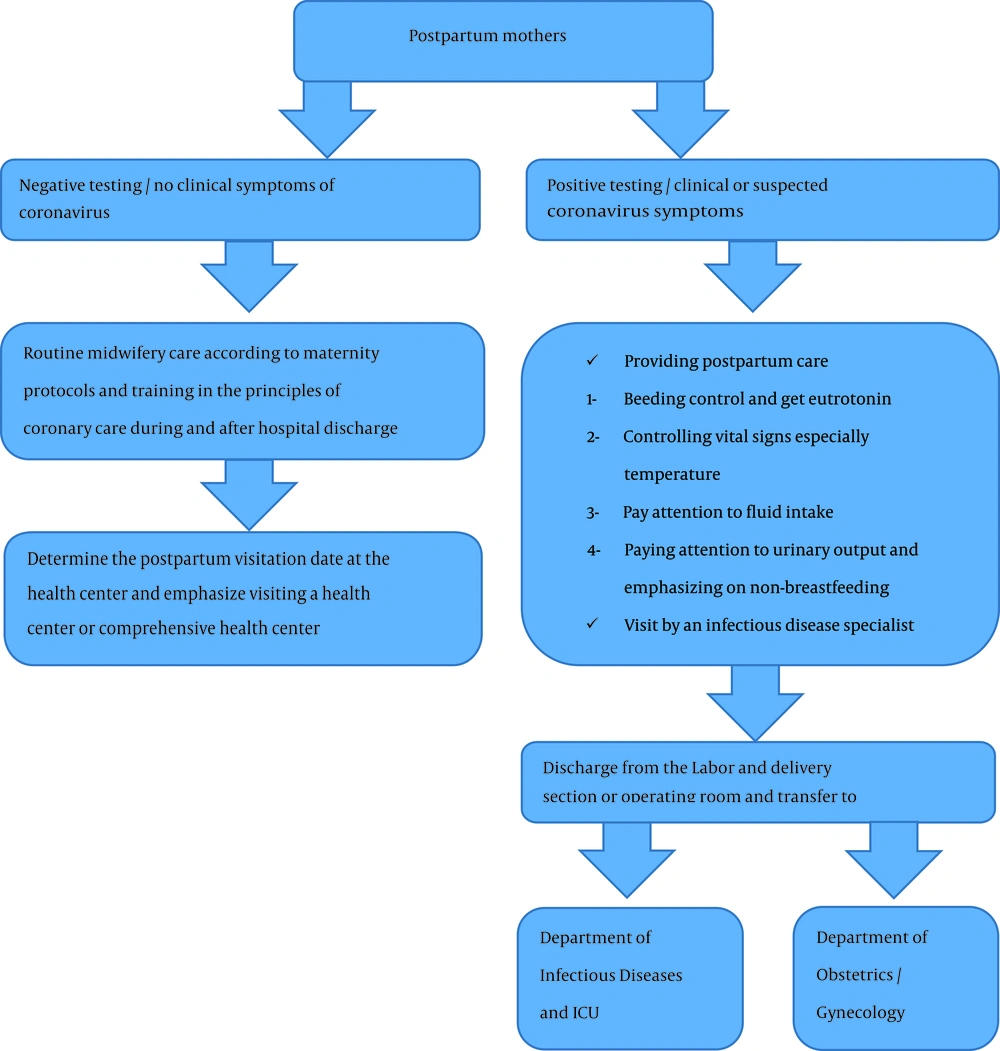
Postpartum is an important step that requires team management and coordination of care between gynecologists, neonatal specialists, midwives, and nurses for accurate delivery to ensure maternal and newborn safety. In this regard, the RCOG and RCPCH recommend that mothers and infants should be kept separate until complete maternal recovery (44).
The care process by the Isfahan University of Medical Sciences in the postpartum phase emphasizes the following: one-to-one mother and midwife care, Lack of breastfeeding and breast milk in mothers with coronavirus, Attention to postpartum midwifery complications and their potential for overlap with symptoms of coronavirus disease, considering postpartum administration of oxytocin, misoprostol, and methylergonovine if needed, attention and differentiation of the symptoms of coronavirus with postpartum amniotic fluid embolism, and specific sensitivity to detecting and recording maternal vital signs, especially fever and respiratory rate. The postpartum care process is attached (Figure 3).
3.8. Lactation (Breastfeeding)
Due to limited studies, the transmission of COVID-19 through breast milk remains unclear. In a study, no viral RNA was detected in the SARS-CoV breast milk test in a mother with improved SARS. However, a sample collected 130 days after the onset of the disease found SARS-CoV antibodies in breast milk (50). However, one patient was tested positive for SARS-CoV-2 on days 12 and 30 postpartum (51). In a study by Chen et al. (22) that examined the milk of six mothers for COVID-19, all samples were negative. Therefore, due to insufficient information, mothers who intend to breastfeed should continue breastfeeding until the appropriate breastfeeding time (10, 40). Infants with positive mothers for SARS-CoV-2 should be kept in a room separate from the mother for at least 14 days or until the virus disappears (16); direct breastfeeding is not recommended during this time. Since breast milk is an important source of antibodies to protect infants, it seems that mothers should be encouraged to breastfeed. The CDC recommends that women who wish to breastfeed should be encouraged to pump milk during the temporary separation of the mother and baby (8). If possible, a dedicated breast pump should be provided. Women should have proper hygiene before pumping breast milk. After pumping, all parts of the pump that are in contact with the breast milk should be thoroughly washed and the entire pump must be disinfected according to the manufacturer’s instructions. Breast milk should be given to the baby by a healthy caregiver. For women and infants who are not separated, the CDC recommends that if a woman wishes to breastfeed, she should use a mask and protective equipment and keep the hands hygienic before each feeding (52). According to the RCOG and RCPCH, guidance on breastfeeding is difficult given the lack of information on vertical transmission. It is also suggested that breast milk banks do not recruit mothers infected with COVID-19 (44, 52). Clinical guidance published by the Iran Ministry of Health is in part consistent with CDC recommendations and states about breastfeeding as follows:
1) If the disease has been definitively diagnosed and the mother is generally ill, temporarily feed the infant with human milk (stored in a milk bank) or artificial milk. With the improvement of the general condition, breast milk should be stored and used following health principles.
2) If the disease is definitively diagnosed and the mother’s general condition is good, breastfeed the infant with breast milk. For this purpose, the mother should breastfeed using a hand-held or electric milking machine. The mother should wash her hands before touching any part of the pump or storage container. After each breastfeeding, all breastfeeding components that have been in contact with the breast and the mother’s hands should be washed or disinfected according to the breastfeeding guidelines of the Office of Population, Family, and School Health.
3) In a mother suspected with the coronavirus, breastfeeding is not prohibited by the mother’s breast (53).
3.9. Care for Infants Born to Mothers with COVID-19
There is limited experience of caring for infants born to mothers with COVID-19. In the report by Zhu et al. (23), some infants had the symptoms (shortness of breath in six infants, cyanosis in three infants, gastric bleeding in two infants, multiple organ failure and DIC in one infant). However, throat swab testing in all infants was negative for SARS-CoV-2. The results suggest that these neonatal complications may not be due to intrauterine transmission. It is unclear at this time whether SARS-CoV-2 can be transferred from the mother to the fetus. Given the current lack of information, it is hypothesized that a baby born to a mother with COVID-19 may become infected during labor, either in the womb or during labor. Therefore, the infant should be isolated to avoid exposure to other infants. The ideal option for a healthy infant is to keep him in the room of the healthy mother, but the temporary separation of the ill mother and her infant, such as in the case of the H1N1 epidemic (54), seems prudent. Due to the long duration of infection, RCOG and RCPCH do not recommend absolute separation but recommend careful separation in healthy infants. They also emphasize the absolute separation of high-risk infants (such as premature or immunocompromised infants and those with respiratory problems) (44). The Iran Ministry of Health’s Office of Health, Population, Family, and School recommends avoiding skin-to-skin contact between the newborn baby and the mother with a definite, probable, or suspected infection. If the mother is suspected of having COVID-19, the baby should be temporarily separated from the mother and kept in another room. If the separation and placement of the infant in another room are not possible for some reason, the infant should be at least two meters away from the mother and a curtain (from the ceiling to the floor) should be placed between the mother and the infant (53).
4. Discussion
Given the emergence of the COVID-19 virus and the lack of adequate studies on the incidence of COVID-19 in pregnancy and its perinatal and maternal complications and consequences, conclusions in many cases still need further studies. Given previous experiences in managing similar viral diseases such as influenza, physiological changes during pregnancy (in the respiratory and immune system), maternal and neonatal complications of respiratory distress, and pandemic infections, special measures should be taken to ensure the proper management of pregnant women and infants for optimal immunity. The morbidity and mortality of COVID-19 are less than those of SARS and MERS. According to the results of studies, preterm labor affects 42% of women hospitalized with COVID-19. If more than 70% of the world’s population is infected with the virus, there may be significant pressure on the maternal and neonatal service sectors, requiring urgent action (55). Therefore, optimal management should be at a health center with close monitoring of the mother and infant (10). In there is a risk of the disease, proper care must be taken for pregnant mothers and the care team should follow an integrated procedure.
Based on suspected or affected pregnant mother's conditions (number of pregnancies, midwifery symptoms during pregnancy, place of residence, presence/absence of health centers, etc.), all screening, diagnosis, and treatment processes during pregnancy, labor, delivery, and postpartum should be planned with greater sensitivity and accuracy and managed in a team-based manner. The type of delivery should be given special attention due to the specific conditions of pregnancy and possible midwifery problems in these mothers. In the case of a mother with coronavirus, an elective cesarean section is performed when the mother has high respiratory involvement and requires immediate termination of pregnancy. This increases the efficiency of treatment. Immediate cord-cutting and immediate separation and evaluation of the newborn of an affected mother should be considered. Breastfeeding should not be performed by a confirmed infected mother (due to the breast milk potential for viral transmission) and the mother and her baby’s quarantine principles must be respected until they are fully remedied (43). No specific treatment for coronavirus has been approved by the US Food and Drug Administration (10, 40). When offering new therapies, pregnant women should be fully consulted about possible side effects for the patient and the teratogenic effects on their fetuses. Information and studies on COVID-19 are growing rapidly. Physicians and midwives should regularly check and read the CDC website to keep their information up-to-date to provide quality services to mothers and babies.
5. Conclusions
Given the limited information on the complications and outcomes of the virus in pregnancy and childbirth and the increasing number of studies, the provision of up-to-date care according to global and regional processes and guidelines is recommended for mothers affected or suspected with COVID-19.