1. Context
In late December 2019, a cluster of infected patients with severe respiratory distress (pneumonia) of unknown etiology were reported in Wuhan, China (1). The virus-caused malady seriously afflicted the society and rapidly spread to other countries (2). In mid-January 2020, “World Health Organization” (WHO) named the virus severe respiratory syndrome-coronavirus-2 (SARS-COV-2), introducing it as the main trigger for acute respiratory distress syndrome (ARDS), and the malady was termed “coronavirus disease 2019 (COVID-19)”. In late January, WHO declared a state of COVID-19 pandemic, and defined it as a public health emergency of global concern (3). Fortunately, ~80% of the involved cases show no clinical symptoms; however, in symptomatic cases, fever, fatigue (myalgia), dry coughs (without phlegm), and acute respiratory problems are considered to be the symptoms of the disease (4).
Owing to the characteristics of dental treatments and settings, the risk of cross-infection, including viral and bacterial pathogens between dental practitioners/personnel and patients, cannot be ignored (5). Despite vigorous efforts by researchers and scientists, as well as the commencement of related clinical studies, except for chloroquine and hydroxychloroquine, which have recently been granted the state of “Emergency Use Authorization (EUA)” by FDA (6, 7), no other effective vaccines or medicinal drugs have been approved for the prevention and/or treatment of COVID-19 (8). Therefore, the need for strict and tough effective protocols for dental practices, especially in potentially affected areas with COVID-19, is of immense significance. In this study, COVID-19 is reviewed, and the recent protocols for infection control in dental treatments and corresponding centers are addressed.
2. Novel Coronavirus Disease 2019 (COVID-19)
Coronaviruses are defined as the largest group of viruses, which belong to the Nidovirales order, including Coronaviridae (alpha, beta, gamma, and delta), Arteriviridae, and Roniviridae families. These families are enveloped, non-segmented positive-sense RNA viruses. Coronaviruses can cause digestive and respiratory diseases in birds and mammals, as well as lethal respiratory infections in humans (9). COVID-2019 seems to be closely related to “Severe Acute Respiratory Syndrome” (SARS)-like coronaviruses (beta-coronavirus) (10). It has been shown that the structure of the receptor-binding domain (RBD) of COVID-19 is quite comparable with SARS coronavirus, and through the similar RBD of their spike protein, COVID-19 can enter the cell via human angiotensin-converting enzyme 2 (ACE2) receptor (11). Epidemiological findings on the first cases of COVID-19 infected patients revealed that the virus was primarily transmitted through bats (12), and pangolins (13) to humans, and then, it was spread person-to-person (12).
3. COVID-19: World and Iran
As of 31 March 2020, it has been reported that COVID-19 has spread and affected 200 countries and territories around the world. Overall, 799,724 individuals have tested positive for the virus, with 169,989 individuals recovered, and 38,721 individuals passed away worldwide. Moreover, and at the same date, the top ten countries which mostly suffered from COVID-19 were USA (164,359 positive cases; 3,173 total death), Italy (101,739 positive cases; 11,591 total death), Spain (94,417 positive cases; 8,189 total death), China (81,518 positive cases; 3,305 total death), Germany (67,051 positive cases; 650 total death), Iran (44,605 positive cases; 2,898 total death), France (44,550 positive cases; 3,024 total death), UK (22,141 positive cases; 1,408 total death), Switzerland (15,922 positive cases; 359 total death) and Belgium (12,775 positive cases; 705 total death) (14).
4. Routes of Transmission
Direct contact (person-to-person) and indirect contact (close contact less than 6 feet, inhaled droplets, aerosols, fecal-oral routes) are the major routes of transmission for COVID-19 (15-17). The incubation period of COVID-19 disease is usually long (varied from 3 - 14 days); however, it differs from one person to another (18). Asymptomatic patients and stealth carriers can transmit and infect other individuals (19).
5. Infection Control in Dental Centers and Practices
The widespread outbreak of COVID-19 (especially in Iran) and its incubation period (20) have made the prevention and control of infection very difficult. Since the main transmission route of the novel coronavirus 2019 is through respiratory droplets, aerosols, and direct contact (21), dental practitioners and personnel are considered a high-risk group (15).
Since there are no vaccine and/or effective medicinal drugs for the prevention and treatment of COVID-19 (22), modifications in the management strategies on infection control protocols in dental centers and practices, particularly in the post-pandemic era, is of great significance. To help dental professionals/personnel to effectively combat the disease, taking into account the current investigations and evidence, some presented measures are as follows:
5.1. General Recommendations
5.1.1. Patient Evaluation in the Waiting Room
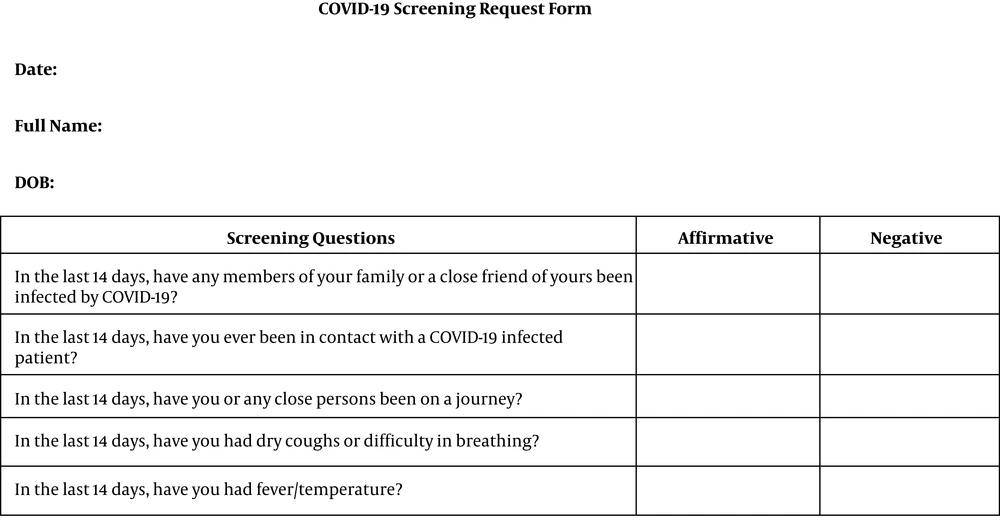
The waiting room in the dental practice/center should be sufficiently ventilated. Before the patient's entry to the dental chair-side, patients should be provided with a surgical or face mask and disinfectant gel, and their temperature should be measured using a sterile or contact-free forehead thermometer. Patients should stay at least six feet from one another/dental personnel. A thorough medical history should be obtained from the patients, and designated screening form (Figure 1) should be precisely completed and signed by the patients.
Furthermore, patients’ education on sneeze and cough etiquettes is of immense importance and should be addressed as follows:
a. Patient encouragement to use disposable tissues and handkerchiefs during coughs and sneezes.
b. Disposal of tissues and handkerchiefs, immediately after use into a garbage bin.
c. Hand hygiene education, after coughs, sneezes, contact with respiratory droplets or contaminated items via mentioned secretions.
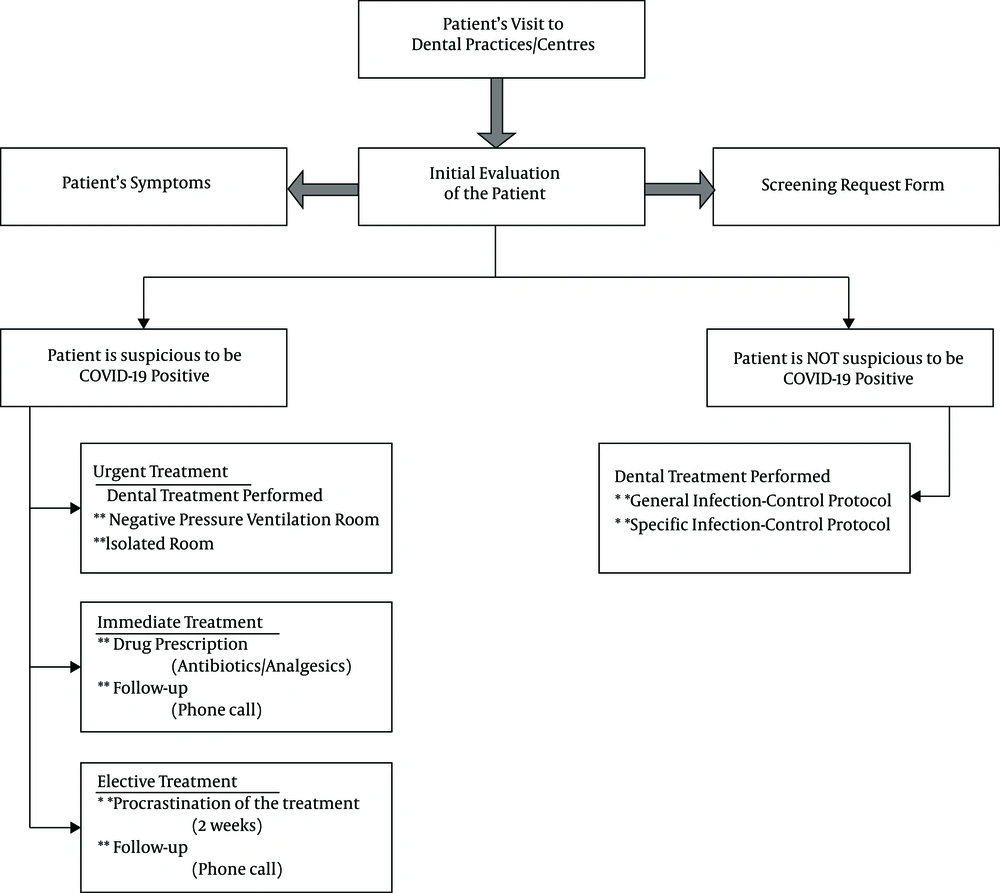
All surfaces in the dental practice environment and medical instruments (e.g., thermometers and sphygmomanometers) should be carefully and repeatedly disinfected using ethanol 70% (23). If a patient is suspected to be positive for COVID-19, having symptoms related to the malady or positive answer to the screening questions, they should be immediately identified, quarantined and referred to the department of infection control in a hospital/center or the local health department (15). However, in case of urgent dental problems, patients can receive necessary treatments even if they are in the acute phase of the disease. In accordance with WHO, the suspicious and positive patients should be transferred to specific precaution rooms with negative pressure ventilation (12 air changes/hour “ACH” or 160 L/s/patient) (24). Patients who do not report any symptoms, can receive dental care and treatments while considering all the above-mentioned advice (Figure 2).
5.1.2. Hand Hygiene
Hand hygiene is one of the principal pathways for reducing the transfer of microorganisms to the patients (25). According to WHO, SARS-CoV-2 can survive on different surfaces from a number of hours to several days (26). Since oral-fecal transmission of the virus has been reported for COVID-19 (27), hand hygiene has become of utmost importance for dental professionals/personnel. Hand hygiene can be achieved in two ways; handwashing with water and soup and hand disinfection using alcohol-based solutions, both for 20 seconds.
In the following circumstances, dental professionals and personnel should follow hand hygiene protocols and prevent their hands from direct contact with eyes, nose, and mouth:
a. Before examination of patients, and beginning of dental treatment.
b. After contact with patients, environmental surfaces and materials/ substances contaminated with blood and body liquids/secretions.
c. After contact with secretions, mouth mucosa, and injured skin.
5.1.3. Personal Protection Measures
Aerosols, which are defined as small and tiny floating particles, are produced in most dental treatments (28, 29). Aerosols can stay suspended in the air for a long time (30) and carry/transfer different substances, from blood and cells to restorative materials and microorganisms (31). Aerosols can be inhaled by dental professionals/personnel and cause respiratory infections and complications (32, 33). Therefore, using self-protective measures is highly recommended for dental ministrations.
a. Protective goggles and face shields
Evidence shows that ocular tissues are susceptible to the transmission of microparticles and aerosols (34). Thus, it is highly recommended to use protective goggles or face shields during dental treatments; so that the eyes and surrounding areas are perfectly covered and protected from the entry of microorganisms. After termination of a dental treatment, the goggle/shield should be properly washed and completely disinfected.
b. Face masks
After termination of dental treatments, used face masks must be disposed. Surgical masks are recommended when the operator is at a distance of less than six feet from the patient, and special masks, i.e., N95 respirator and FFP2 masks are suggested when there is a possibility of aerosol production.
c. Protective outwear (gown)
Protective outwears should be changed after the termination of each dental treatment.
d. Gloves
Dental professionals and personnel should change their protective gloves (latex, nitrile, nylon, and so forth) after the termination of each dental treatment. In addition, hand hygiene protocols should be precisely followed immediately before and after wearing gloves. Protective gloves might have unidentified or small tears, which could end in rupture of the glove during use. It is highly recommended to use two pairs of gloves during dental surgical procedures.
5.1.4. Surface Disinfection
Dental chair-side surfaces -i.e., dental light handle, dental chair keyboard keys, connected computers/laptops, oral cameras, dental surgery drawer handles, water taps, stationaries, working desks, telephone sets, doorknobs and so forth- and peripheral surfaces -i.e., floor, walls, washing sink/faucets and so on- should be disinfected in the intervals between patients using ethanol 70%.
5.1.5. Mouth-Rinsing Before Dental Treatment
Mouth-rinsing with antibacterial solutions cannot impede the transfer of COVID-19 from the patients to the dental professionals/personnel and vice versa; nevertheless, it can reduce the number of microorganisms, which are in contact with blood during invasive dental treatments (35).
Using mouth-rinses before dental treatments can cause a reduction in the oral cavity microorganisms (36-38). In accordance with the guidelines in the diagnosis and treatment of COVID-19-caused pneumonia by the health council of the People’s Republic of China, chlorhexidine (as a common mouth-rinse and mouthwash solution) may not be effective against COVID-19. Since the virus is quite sensitive to oxidation, using a mouth rinse or mouthwash solutions containing hydrogen peroxide is recommended (39).
5.1.6. Use of Other Materials/Instruments/Equipment
Rubber dam, specifically when handpieces and ultrasonic devices are used, can minimize the dispersion of droplets, secretions, and aerosols. It is recommended to use high volume evacuators (HVE) when rubber dam is to be applied. In these circumstances, four-handed technique is usually practiced. If rubber dam cannot be applied, the use of hand instruments, e.g., hand scalers/curettes are recommended for periodontal purposes or carisolv for chemomechanical caries removal (40).
5.1.7. Removal of Medical/Dental Waste
Disposable protective equipment should be transferred to a temporary storage area. The medical waste -from the treatment of patients suspicious to COVID-19- should be considered an infectious residue. These wastes should be packed in two-layered packages and sealed properly.
5.2. Specific Dental Considerations for the Reduction of Aerosols
In all branches of dentistry, the mentioned infection-control principles should be carefully followed. However, in a number of specialties, there are other points to consider:
5.2.1. Endodontics
The application of rubber dam in endodontic treatments is highly recommended at all times. In these circumstances, it is advocated to use hand instruments instead of rotary systems. In the case of pain due to symptomatic irreversible pulpitis, pulp exposure and devitalization could be made with chemomechanical caries removal and a HVE after local anesthesia under rubber dam isolation. In these circumstances, vital pulp therapy (VPT) is much preferred to conventional root canal treatments.
5.2.2. Restorative and Pediatric Dentistry
In elective cases, high treatment priority is given to chemomechanical caries removal and atraumatic restorative techniques. Similar to endodontic considerations, hand instrumentation for cavity preparation is preferred to rotary preparations. However, if rotary instruments are to be considered, rubber dam isolation should pertain. Moreover, manual scaling and polishing are endorsed.
5.2.3. Periodontics
It seems that hand and ultrasonic approaches have similar clinical effects on the reduction of dental plaque and calculi (41), and there were no significant differences between the two methods (42, 43). Therefore, and in suspicious circumstances, using instruments manually is preferable.
5.2.4. Prosthodontics
To avoid gagging in patients, salivary suction should be used. If an impression is taken, the impression and other prosthodontic materials (e.g., bite registration and so on) should be properly disinfected prior to the delivery to prosthodontic laboratories. The disinfection procedure is as follows:
a. Initial irrigation using tap water
b. Placement of the material in a disinfectant with at least intermediate level activity, i.e., sodium hypochlorite for 10 minutes.
c. Re-irrigation using tap water
Furthermore, the application of rubber dam is an all-time necessity for crown and bridge/other prosthodontic preparations. Modification of treatment plans can also be considered; for example, supra-gingival margins for posterior bridges or using split-dam techniques.
5.2.5. Oral and Maxillofacial Radiology
Extraoral dental radiographies i.e., cone beam computed tomography (CBCT) and panoramic radiography are recommended.
5.2.6. Oral and Maxillofacial Surgery
When ministrations e.g., a simple extraction, are performed, the patient should be treated in the supine position. Using salivary suction and/or HVE during procedures is necessary. When there is a wound, it should be rinsed slowly. In the case of sutures, using absorbable material is preferable.
6. Conclusions
The widespread outbreak of COVID-19 and the pandemic of the novel coronavirus have become a global concern and a serious threat to the health, well-being, and survival of humans. The characteristics of dental treatments and the possibility of aerosol production during such ministrations classify dentistry as one of the most high-risk jobs in the world. The existing knowledge on COVID-19 is currently limited, and studies for vaccines, effective medicinal drugs, and possible treatments are imminent. Comprehensive research and investigations are needed to clarify COVID-19 routes of transmission, pathogenicity, and its mechanisms, and define potential pharmaceutical purposes. Hereby, we addressed protocols on infection-control for general and specific dental treatments and presented conventions for the protection of dental professionals/personnel from the transmission of the virus in the coming months.