1. Context
Using smart mobile devices, called mobile health (mHealth), facilitates providing health services, speeds up the process, and reduces the costs and complications of direct services (1, 2). mHealth is a practice that provides health care services indirectly in wireless and remote communication (2, 3). mHealth is a type of health information technology that can be used to provide health care services as a supportive tool. Many apps and software have been developed in a mobile platform in all aspects of health care (3). mHealth can be used in epidemic and pandemic outbreaks because of its accessibility, ease of use, and attracting many users (4). Therefore, in recent years, there has been a growing use of mHealth in epidemic conditions.
Coronavirus 2019 (COVID-19), as a pandemic outbreak, emerged on December 31, 2019, in China and quickly spread around the world (5, 6). By March 1, 2020, there were 859,392 affected cases and 42,327 deaths worldwide (7). COVID-19 is a coronavirus disease that appears as a severe acute respiratory syndrome with symptoms such as fever, cough, shortness of breath, and sore throat (5, 8, 9). Given the enormous damage to society, many countries adopted specific policies to deal with COVID-19.
One of the key programs for tackling COVID-19 is the use of information technology, including mHealth. In recent years, mHealth capacities have been used in many countries as a new technology to control epidemic/pandemic outbreaks, with valuable results. Navin et al. (10), in their study in 2017 provided a mHealth solution to use in the public health epidemic surveillance system and it showed a high capability to detect any disease outbreak. Also, Lwin et al. used FluMob, a mHealth app, for tracking influenza by obtaining real-time epidemiological and surveillance data from healthcare providers by allowing them to report influenza incidence using smartphones (11).
Given the importance of mHealth technology in dealing with COVID-19 as a pandemic outbreak, this study briefly reviewed studies of the use of mHealth in recent epidemic/pandemic outbreaks worldwide to learn some lessons on how to deal with COVID-19.
2. Evidence Acquisition
This review study was done in 2020. To find related studies, searches were done in PubMed and Scopus, as well as Google Scholar, by related keywords (Table 1).
| Search Strategy | Details |
|---|---|
| Limitations | |
| Time | 2014 - 2020 (March, 10) |
| Language | English language |
| Other limitations | |
| PubMed | Human |
| Scopus | Medicine and article |
| Used keywords | |
| #1 | “pandemic” OR “epidemic” OR “outbreak” OR “corona” OR “COVID-19” |
| #2 | “mobile” OR “mobile health” OR “mobile phone” OR “mHealth” |
| Search | |
| #1 AND #2 |
The Search Strategy
We included studies of using mHealth in an epidemic/pandemic infectious disease outbreak and reporting/describing the mHealth application in epidemic/pandemic outbreaks. Studies on other health information technologies such as geographic information systems and telemedicine were excluded from the study. Also, studies not focusing on epidemic/pandemic outbreaks were excluded. Studies that used PC or web-based applications for population tracking and data analysis were removed, as well.
After selecting the related studies, data were extracted using a data extraction form and analyzed by the content validity technique. In this regard, the data were categorized into themes and sub-themes based on the study objectives.
3. Results
Of 727 retrieved studies in the initial search, after applying inclusion and exclusion criteria, 17 studies were selected for the study. Table 2 shows the selected studies.
| Authors | Year | Study Type | Study Population | Study Objective |
|---|---|---|---|---|
| Navin et al. (10) | 2017 | Developmental | - | Providing mHealth for detecting any disease outbreaks |
| Toda et al. (12) | 2016 | RCT | 135 participants | Assessing the text message system for outbreak alert in Kenya |
| O’Donovan and Bersin (13) | 2014 | Correspondence | 167000 users | Reporting an experience of IBM company about implementing a mHealth program in three countries (launching a disease-mapping system) |
| Abiola et al. (14) | 2015 | Case report | 100 smartphones | Contact tracing using ubiquitous sensors present in the node smartphone application on Android phones |
| Otu et al. (15) | 2016 | Cross-sectional | 203 participants | Reporting an education intervention that used tablet computers for health workers training |
| Gu et al. (16) | 2015 | Cross-sectional | 9105 users | Using a mobile internet device to assess KAP regarding H7N9 among mobile users |
| Phillips et al. (17) | 2014 | Commentary | - | Introducing a novel method of mHealth for the patient-physician relationship |
| Gashu et al. (18) | 2020 | Review | Articles | Assessing the effect of mobile phone messaging on anti-TB success treatment |
| Racine and Kobinger (19) | 2019 | Commentary | - | Reporting challenges and perspectives on the use of mobile laboratories during outbreaks and their use for vaccine evaluation |
| Danquah et al. (20) | 2019 | Developmental | 26 contact tracing coordinators (CTCs) and 86 contact tracers (CTs) working in 11 chiefdoms | Designing and evaluating an electronic system for tracking contacts of Ebola cases |
| Rebaudet et al. (21) | 2019 | - | 7,856 weekly cholera alerts | Describing and evaluating the exhaustiveness, intensity, and quality of CATIs in response to cholera alerts |
| Kim et al. (22) | 2019 | Cross-sectional | 7702 influenza reports | Evaluating the Fever Coach app in real-time surveillance of influenza activities for children and parents |
| Fujibayashi et al. (23) | 2018 | Cross-sectional | - | Evaluating the new influenza-tracking mobile phone app that used a self-administered questionnaire |
| Guetiya Wadoum et al. (24) | 2017 | Cross-sectional | 910 medical consultations | Identifying the applications of mHealth clinic developed for Ebola in Sierra Leone |
| Rosewell et al. (25) | 2017 | Case study | 160,750 malaria tests | Describing an m-health initiative to strengthen malaria surveillance in a 184-health facility, and provinces |
| Lwin et al. (11) | 2017 | Descriptive | Health care workers | Describing the development of FluMob |
| Kuehne et al. (26) | 2016 | Cross-sectional | 6,813 household members in 905 households | Describing the health-seeking behavior during the Ebola |
The Selected Studies
Of 17 reviewed studies, 14 (82.35%) studies were about epidemic outbreaks, and the rest concerned pandemic outbreaks. All studies emphasized the positive effect of mHealth in epidemic/pandemic outbreaks. Table 3 shows the location of the studies by countries and the World Health Organization (WHO) regions.
| Numbers | WHO Regions | Countries | Numbers of Studies | Total Numbers |
|---|---|---|---|---|
| 1 | African Region (AFRO) | Kenya | 1 | 10 |
| Guinea | 1 | |||
| Liberia | 2 | |||
| Sierra Leone | 3 | |||
| Nigeria | 2 | |||
| Ethiopia | 1 | |||
| 2 | Region of the Americas (PAHO) | US | 1 | 3 |
| Canada | 1 | |||
| Haiti | 1 | |||
| 3 | Eastern Mediterranean Region (EMRO) | - | - | - |
| 4 | European Region (EURO) | - | - | - |
| 5 | South-East Asia Region (SEARO) | India | 1 | 1 |
| 6 | Western Pacific Region (WPRO) | China | 1 | 5 |
| South Korea | 1 | |||
| Japan | 1 | |||
| New Guinea | 1 | |||
| Singapore | 1 |
The Location of Selected Studies
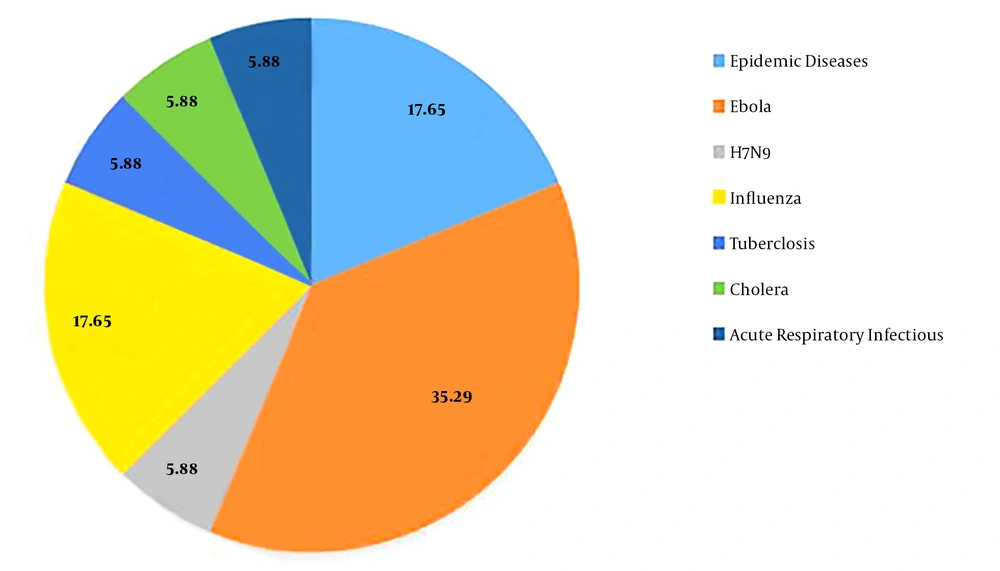
Figure 1 shows the epidemic/pandemic diseases. Based on Figure 1, most of the studies were about Ebola (35.28%).
The results showed that mHealth can be applied in five main categories (Table 4).
| Main Applications of mHealth | Application Types |
|---|---|
| Public health aspects | Control of the epidemic spread (13) |
| Notification in outbreaks (12) | |
| Surveillance: population, healthcare workers, real-time surveillance (10-12, 22, 25) | |
| Interventions on nutrition behaviors and nutrition-related health outcomes (27) for quarantine and isolation | |
| Contact tracing and monitoring (14, 20, 27), epidemic tracking (23) | |
| Vaccine reminder systems (28) | |
| Analyzing trends and forecasting (29), disease mapping systems (13), and health-seeking behavior (26) | |
| Public awareness (30) and patient self-monitoring (23) | |
| Data management | Data collecting (22) |
| Data transmission between healthcare centers (31) | |
| Reduce health disparities due to facilitating data exchange (17) | |
| Easy access to near real-time information (23) | |
| Providing timely, high quality, geo-coded, case-based data (25) | |
| Educational programs | Patient and public education (16) |
| Health care provider and student education in epidemic conditions (15, 32) | |
| Identifying sociodemographic information for people education (16) | |
| Patient identification and diagnosis | Patient identification (25) |
| Patient and physician relationship (tele-visit) (17) | |
| Mobile laboratories (19) | |
| Disease testing for screening (25) | |
| Treatment | Fever Coach (22) |
| mHealth Clinic (24, 33) | |
| Home visit (tele-visit) (34) |
The mHealth Applications in Epidemic/Pandemic Outbreaks
However, the main reason for using mHealth in outbreaks was to support people and patients. Furthermore, health care providers, managers, and policymakers were other mHealth stakeholders.
4. Discussion
One of the effective ways of tackling epidemic/pandemic outbreaks is to use communicational health information technologies, such as mHealth. For tackling and controlling COVID-19 as an emerging pandemic, we should use the capabilities and applications of mHealth. Some countries with high epidemic/pandemic outbreaks used mHealth to encounter this condition. The AFRO and WPRO countries had the most use of mHealth in epidemic/pandemic outbreaks. One of the main causes of high-level mHealth use in these two regions can be the high prevalence of epidemic/pandemic diseases.
The results of the study showed that the most use of mHealth was related to Ebola, an infectious disease that is more prevalent in AFRO. Also, for influenza, which has the most similarity to COVID-19 among the mentioned diseases, the policymakers and managers used mHealth, especially in providing remote healthcare services for patients (17, 25). The results of the study showed that the application of mHealth in epidemic/pandemic outbreaks can be divided into five main categories, as follows:
4.1. Public Health Aspects
One of the most important parts of the control and elimination programs of an epidemic/pandemic outbreak is public health programs (35). Thus, mHealth can be used as a supportive method for implementing public health programs in an epidemic/pandemic outbreak (10). Based on the results of the study, the main role of mHealth is in public health aspects. The most useful application of mHealth was in surveillance purposes, which include community surveillance, healthcare workers surveillance, and real-time surveillance (10-12, 22, 25). Due to the high prevalence of COVID-19 in the world, its surveillance is very important and mHealth can play a pivotal role. Also, one of the other problems in controlling COVID-19 is inefficient contact tracing (36) to prevent its spread. Research shows that contact tracing and monitoring by mHealth are an appropriate way (14, 20). Thus, it is proposed to use mHealth capabilities for contact tracing of COVID-19 cases. Also, mHealth can be used for vaccine reminder systems, epidemic tracking, public awareness, trend analysis and forecasting, health-seeking behavior, and patient self-monitoring (23, 26, 28-30). All of these applications can be used for COVID-19 as an emerging pandemic outbreak.
4.2. Data Management
In an outbreak condition, data management is an important function that is a foundation for other practices and programs (37). mHealth technology can be used as a key method for better data management in outbreaks (38). Moreover, mHealth can be used for data collection (22), data transmission between healthcare centers (31), health disparities reduction due to facilitating data exchange (17), easy access to near real-time information (23), and timely, high quality, geo-coded, and case-based data provision (25). In the case of COVID-19, the use of mHealth is recommended due to the importance of timely and accurate data exchange (39).
4.3. Educational Programs
Patient and public education, as well as healthcare provider training, is very important during an epidemic/pandemic outbreak (40-42). Research shows that mHealth is an effective method for implementing educational programs during an epidemic/pandemic outbreak (15, 32). Moreover, mHealth can be used to identify sociodemographic information for people education (16) by the analysis of available data. This is an appropriate method to educate people about COVID-19 based on their sociodemographic information. These mobile-based educations for COVID-19 can be provided through multiple methods such as texts, pictures, voices, videos, and online voice/video communication.
4.4. Patient Identification and Diagnosis
Patient identification can be made using various technologies, and one of the fast and low-cost methods of patient identification is mHealth (43). Due to the high accessibility of mobile phones in the society, accounting for more than 7.26 billion users all over the world in 2020 (44), one of the appropriate ways of identifying COVID-19 cases is mHealth. Also, mHealth is a proper method for improving the patient-physician relationship (17), implementing mobile laboratories (19), and testing for screening (25). These applications provide a good opportunity for establishing social distancing as an important way of controlling COVID-19 (45).
4.5. Treatment
The treatment of epidemic/pandemic communicable diseases such as COVID-19 imposes a high risk on health care providers (39). Information technology is a good option for decreasing the direct contacts of patients with healthcare providers (46). Based on the results, mHealth can be used for fever Coach (22), home visits (tele-visits) (34), and mHealth clinics (24, 33). These are practical to COVID-19 for tackling the disease.
5. Conclusions
The main applications of mHealth for epidemic/pandemic outbreaks include public health aspects, data management, educational programs, patient identification and diagnosis, and patient treatment. In the case of COVID, mHealth is one of the best choices to use in the patients’ and physicians’ relationship as tele-visit, to fever coach, real-time information provision for healthcare providers, and disease detection based on data obtained from different locations. Due to the low cost, ease of use, availability, and accessibility of smart mobiles, the use of mHealth is proposed to tackle COVID-19 at present. However, to eradicate COVID-19, we should use all applications of mHealth as a supportive method alongside other health information technologies. It is suggested that further studies be done to achieve more exact results about the mHealth role in epidemic/pandemic outbreaks and more apps and mobile-based software be developed in similar conditions.