1. Introduction
Chest computed tomography (CT) has a high sensitivity for the diagnosis of COVID-19, and it is considered an important tool for COVID-19 detection in epidemics. However, imaging manifestations of viral pneumonia have similar CT findings. Here, we report two cases of suspected patients whose final diagnosis was not COVID-19 infection. This reminds us to emphasize the important role or CT in the early detection of COVID-19 and avoid overdiagnosis during clinical procedures.
2. Case Presentation
2.1. Case 1
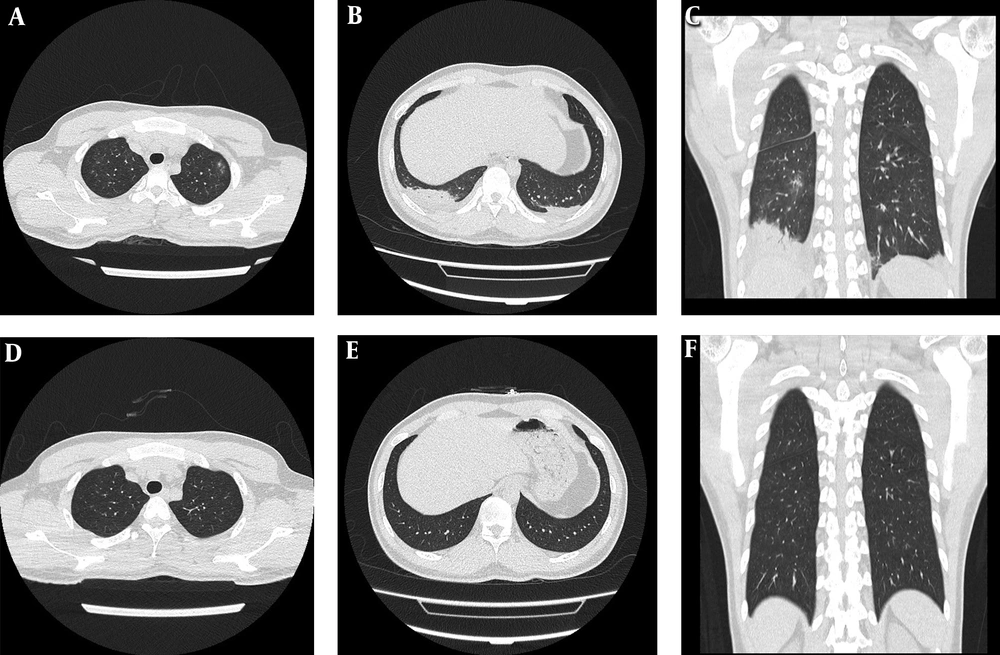
A 24-year-old man, border officer, who lived in Zhuhai, China, and had close contact with people from Hubei Province at work, was admitted to the hospital on February 4 due to limb weakness. On the night of February 5, the patient showed a mild fever of 37.3°C. The chest CT examination showed multiple ill-defined ground-glass opacities (GGO) in both the upper lobe and the middle lobe of the right lung, and consolidation lesions in the subpleural area of both lungs, with a small amount of bilateral pleural effusions and likely bibasilar compression atelectasis (Figure 1A-C). Due to the special nature of the patient’s work, the patient was suspected of having COVID-19 infection after consultation with the hospital expert group. Then, he was transferred to the isolation ward for isolation treatment on February 6, and close contacts were advised to avoid. On February 6, 8, and 9, the repeat RT-PCR 2019-nCoV nucleic acid assays were negative for three consecutive times, and the body temperature was normal for three consecutive days. On February 9, the chest CT was re-examined after three days of therapy and showed the near-complete resolution of inflammation (Figure 1D-F). The person was considered not suffering from COVID-19 infection, and allowed to leave the isolation room. Based on the test result of potassium (K < 1.32 mmol/L) upon admission, hypokalemia was considered. After the potassium supplement, blood potassium returned to the normal level. The endocrinologist noticed that the patient had pulmonary exudate due to hypokalemia. A thyroid function examination indicated hyperparathyroidism accompanied by periodic paralysis.
2.2. Case 2
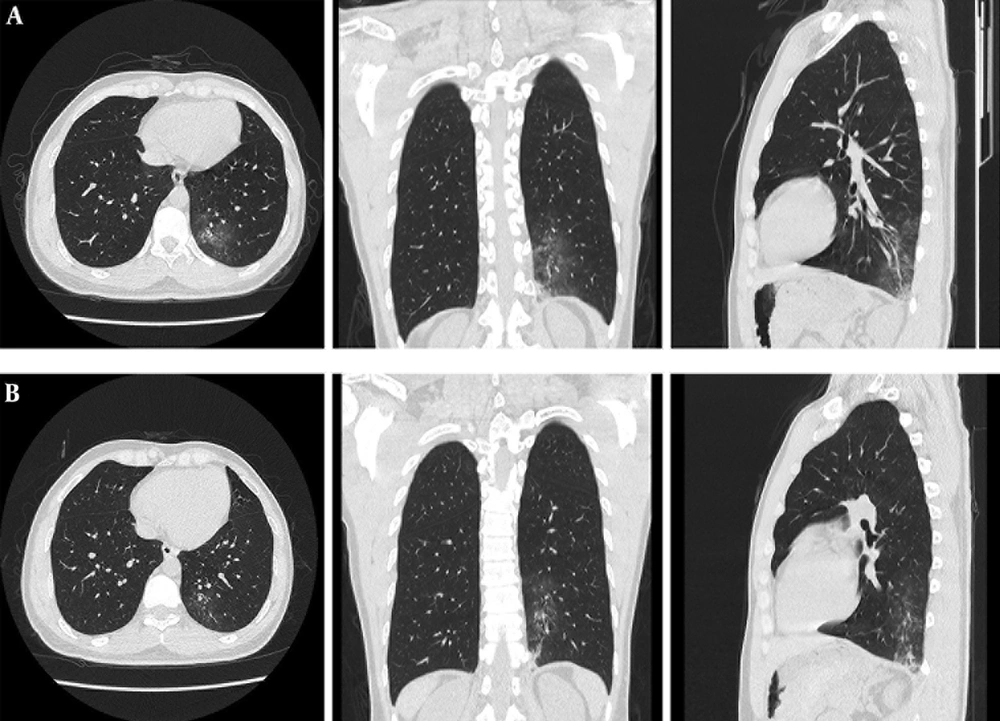
A 34-year-old man, hospital logistics buyer, who was in charge of purchasing protective equipment during the COVID-19 epidemic, had close contact with many people. No fever and cough symptoms, aversion to cold, appeared on February 6. A chest CT examination was performed on February 7. Axial unenhanced chest CT showed consolidation surrounded by GGO in the lower lobe of the left lung with a typical air bronchogram, and one pure GGO lesion in the lower lobe of the right lung (Figure 2A). Follow-up CT images on day 3 after admission showed improvement in the extent of GGO, absorption with fewer lesions, and decreased lesion density. The lower lobe of the left lung showed smaller regions of patchy consolidation (Figure 2B). This patient recovered uneventfully after 10 days.
Unenhanced chest CT images in a 24-year-old man. A, Axial image shows multiple ill-defined ground-glass opacities in both upper lobes; B and C, patchy fuzzy shadows and patchy consolidation can be seen in the subpleural area of both lungs, and a piece of ground-glass opacities in the middle lobe of the right lung with a small amount of bilateral pleural effusions and likely bibasilar compression atelectasis; D, E, and F, CT scan obtained after three days of therapy shows complete resolution.
Unenhanced chest CT images in a 34-year-old man. A, The three-dimensional CT image shows consolidation surrounded by ground-glass opacity in the lower lobe of the left lung with a typical air bronchogram; B, CT scan obtained after three days shows mild improvement in the lower lobe of left lung consolidation.
3. Discussion
The early diagnosis of COVID-19 is important for disease treatment and control. According to current research, the chest CT examination is highly sensitive and specific for COVID-19 diagnosis (1-3). During February 2020, real-time reverse transcriptase-polymerase chain reaction (RT-PCR) testing could not meet the diagnostic requirements because of the sharply increasing number of suspected COVID-19 patients in Wuhan, Hubei, China (4). On February 8, 2020, the “clinical diagnosis cases” were added in the fifth edition of the new NCP diagnosis and treatment plan released by the National Health Commission of People’s Republic of China. Accordingly, patients in Hubei Province who have ground-glass lesions in CT examinations should be considered as clinical diagnosis cases (5). These patients must be hospitalized and isolated. COVID-19 can be clinically diagnosed as long as suspected cases show imaging features of viral pneumonia. However, our report of two cases of suspected patients reminds us to emphasize the important role of CT in the early detection of COVID-19 and avoid overdiagnosis during clinical procedures.