1. Background
Genital warts (GW), or condylomata acuminata, are one of the most common sexually transmitted infections (STIs) worldwide, caused by a variety of human papillomavirus (HPV) (1). Types 6 and 11 of this virus are responsible for 90% of all GW infection cases, which usually have benign effects; however, they are sometimes associated with genital tract malignancy (cervical dysplasia) and respiratory tract malignancy (2).
Various rates are reported for human papillomavirus (HPV) infection in different countries and even different regions of a county (3). In 2018, the global prevalence of HPV infection was 11.7%. It worth noting that Africa and Pacific regions tend to have the highest prevalence (4). It is generally assumed that approximately 16% of the world’s population carry the HPV virus (5). The latest statistics on GW prevalence are from 2012, in which, based on a systematic review, GW global prevalence (general population as a denominator) was estimated at 0.15% - 0.18%. However, the prevalence of the disease is very diverse in different regions: GW prevalence in Africa is reported to range from 2 to 14% (6), 5% in South Asia (7), and 13.6% in East Asia (3). Although the prevalence of HPV infection in Iran had been estimated at 5% - 15%, so far, no study has accurately reported GW prevalence among the Iranian population (8).
Although in most cases GW is benign and cause no severe health consequence (9), it may result in several negative psychological effects, such as stress and anxiety, embarrassment, anger, disgust, depression, and feelings of not being useful, which may, in turn, affect sexual activity (10). Moreover, these lesions may cause secondary malignancies such as cervical cancer. Additionally, people with GW caused by papillomaviruses are 20% more likely to have other STIs, which increases the risk of spreading HIV by 2 - 5 times. Therefore, a GW diagnosis may present a useful opportunity to prevent the development of highly dangerous sexually transmitted diseases like AIDS (11).
Since 1996 the Irian healthcare system is publishing data on GW prevalence. Because of stigmatization and shame surrounding STIs, most GW patients prefer referring to the private sector, instead of public healthcare centers, for diagnosis, treatment, and other healthcare services. Nevertheless, few private providers report their health information to national systems, as low as 5% - 14.4%. This means little certainty about the current recorded statistics of the country’s reporting system (12). Furthermore, several epidemiological and laboratory studies have sporadically investigated the prevalence of HPV infections and cervical cancer in the Iranian population, and have often sought to investigate the risk factors for GW; none of them have provided accurate information on the incidence and prevalence of GW across the country (13). Also, questioning people directly about STI-related symptoms, including GW, may be subject to response bias. Therefore, none of the above methods alone can provide necessary, accurate information about the prevalence of GW.
Many previous studies have been conducted on specific social groups, mostly were focused on the national female population. While men play a key role in the transmission of STIs, few studies have assessed GW in men (14). Hence, the currently available evidence can not be generalized to the general population. For instance, a cross-sectional study on 483 biopsy specimens of epithelial cells of the urethra, penis axis, head of the penis, scrotum, and anus of Iranian men have investigated the prevalence of HPV infection and its genotype distribution and reported related virus DNA present in 269 cases. HPV type 6 is the most common genotype (46.2%), followed by HPV type 11 (15). Another study conducted in Kermanshah Province, intended to study the epidemiology of GW among women referred to a dermatology clinic affiliated to the Kermanshah University of Medical Sciences, reported that 206 women were diagnosed with GW with clinical symptoms (8).
The city of Bushehr is the center of one of the southern provinces of Iran, with a population of 219,076 people, of whom more than 95% are Muslim. As a large regional city, Bushehr is not an exception to the issue of GW. According to the best knowledge of the authors, no estimation is provided about the prevalence and incidence of GW in Bushehr. Bushehr has a significant immigrant population due to its industrial sectors. Hence, similar to other similar areas, it can be assumed that the prevalence of high-risk behaviors that lead to the transmission of GW is higher in this region. However, according to the statistics of the Ministry of Health in 2018, the number of cases of GW (NCGW) was 20 people. According to unofficial surveys, though, the NCGW appears to be more than the recorded cases in the clinics of midwives, general practitioners, and specialists in dermatology, obstetrics and gynecology, urology, and infectious diseases.
Therefore, to estimate the true NCGW, the optimal method is to conduct an indirect study that combines the above methods, so that information collected from both individuals and clinics be used. In this way, the generalizability of the results can be increased.
2. Objectives
The present study, which is the first experiment of its kind in Iran, intended to estimate the number of cases of genital warts (NCGW) in Bushehr using the multiplier method. It can be regarded as the first step towards conducting further related studies and can pave the way for estimating the total number and prevalence of GW in Iran.
3. Methods
This cross-sectional study was performed in two separate phases for 2 months (June and July) in 2019 in Bushehr City.
3.1. Phase 1: Data Collection-GW Patients Referred to Private and Public Clinics
According to a report by the Medical Council of Bushehr Province in 2019, 92 private clinics belonging to general practitioners and specialists (in obstetrics and gynecology, dermatology, and urology) and midwifery clinics in Bushehr. Forty private clinics (including 14 general practitioners, 8 midwives, 10 gynecologists, 3 dermatologists, and 5 urologists), in addition to 8 public clinics, were enrolled in the present study, using the convenience sampling technique. Inclusion criteria were as follows: (1) providing informed consent to participate; (2) having a private clinic or working in hospitals and clinics in Bushehr; (3) a minimum of two years’ of medical experience in Bushehr; and (4) consulting more than 50 patients per week. Exclusion criteria included a reluctance to participate or withdrawing from the study. The referral patterns were such that a percentage of patients were referred directly to the centers and a percentage were referred by other physicians. Therefore, the patients may potentially have been registered in two centers.
People reported single or multiple lesions in the vulva, perineum, anus, vagina, cervix, penis, scrotum, and urethra. Their lesions were diagnosed as GW, and were often painless, though some reported accompanying symptoms such as itching, burning, vaginal discharge, and bleeding. Accordingly, physicians and midwives reported those patients with clinical GW symptoms who were resident in Bushehr. Most diagnoses were based on visual examinations, and sometimes laboratory tests were also used. To collect information on patients with GW from selected private and public clinics, a researcher-made checklist comprised of 10 items was used. The first 5 items were about demographic characteristics (age, sex, marital status, and location), and items 5 to 10 included clinical information (lesion location, diagnosis, treatment, and history of infection). The face and content validity of the checklist were qualitatively reviewed through expert meetings with eight physicians and midwives. For all patients, checklists were filled by a physician or secretary. Then, all checklists were collected.
3.2. Phase 2: General Population Survey About GW History and Treatment in the Past Month, July 2019
To survey the population, a researcher-made checklist was adapted from a standard questionnaire, whose content validity had been confirmed in previous studies. Its Kuder-Richardson index was 75% (16). The checklist included items about: (1) GW infection in the past month; (2) type of post-infection procedure; (3) if seeking treatment, provider that health services were received; and (4) demographic characteristics. The evaluation of the face and content validity of this checklist was conducted during expert meetings consisting of gynecologists, dermatologists, urologists, infectious diseases specialists, midwives, and general practitioners as well as epidemiologists.
The sample size was estimated as 852 subjects using the “n = (Z2 pq/ d2)” formula, based on the mean prevalence of 10% for HPV in Najafi et al.’ study (8), a 95% confidence interval, and 0.02014 error. Participants were selected using a multi-stage, non-random sampling technique. Each of the two municipal areas of Bushehr was considered as a floor. Then, in each area, the most densely populated places were identified as clusters; on each floor, several clusters were non-randomly selected. Sampling from the selected clusters was performed non-randomly and regularly (1 individual every 10 minutes) among eligible passers-by on all days of the week and during busy hours (0900 h to 1300 h and 1800 h to 2300 h). The inclusion criteria were: (1) the ability to answer the questions; (2) living for at least two years in Bushehr; and (3) aged over 18 years. The exclusion was criterion was the unwillingness to participate.
As some items were gender-specific, we used both female and male interviewers. The interviewers were familiar with medical sciences as well as the local culture. After selecting the individuals and explaining the purpose of the study, participants were assured of the confidentiality of the information. Besides, they were informed that they can refuse two participate. Afterward, items were asked, and the answers were recorded. To reduce people’s misunderstandings of GW, especially for people with low or no literacy, the interviewers also explained all the symptoms associated with the disease GW and showed them pictures of warts if needed.
In order to describe the data obtained from patients with GW referred to the selected private and public clinics, descriptive statistics indicators such as frequency and percentage frequency were used. Chi-square test was used for investigating the association between GW infection and variables of age, marital status, and education level. The survey analysis was also used to calculate GW prevalence in the general population, by considering the weighted sample probability and finite population correlation, as well as the effects of place of residence (municipal areas) and gender.
Finally, to estimate the number of patients with GW in Bushehr (S), an indirect multiplier method was used, in which the estimation of the hidden population was performed using two independent data sources (17). The S = P1/P2 × M formula was used, in which multiplier (M) represents the total number of patients who were referred to private and public clinics in June, P1 indicates the ratio of the patients with GW to the total number of those referred to clinics in June, and P2 shows the ratio of people with a history of GW in the past month who were referred to private clinics.
Finally, the S was calculated separately for each medical specialty and gender. Then, by considering that only some private clinics participated in the present study, the estimated values of S were adjusted based on the participation percentage of private and public clinics (government clinics had a 100% participation). In order to estimate the NCGW accurately and also to estimate the confidence interval, the Monte Carlo method was used in STATA version 14. Therefore, NCGW was estimated in a probability distribution with a 95% uncertainty level (UCI) ranging from 2.5 to 97.5% by creating a random model based on the range of desired parameter values (with specific mean and standard deviation).
4. Results
4.1. Description of GW Patients Referred to Private and Government Clinics
Urologists have the highest rate of participation, followed by gynecologists, dermatologists, midwiferies, specialists in infectious diseases, and general practitioners. The total number of the registered cases of GW in the private and public clinics was 186 (59.14% male). Additionally, 173 (93%) cases were reported by private clinics. The mean age of patient age was 30.83 ± 8.07, most of them (n = 99 or 53.2%) were in the age group of 25 to 34 years, particularly the age of 30. Most of the participants were living in the city of Bushehr (n = 149 or 80.11%). While the lowest number of participants was from other cities (n = 37 or 19.89%) (Table 1).
| Variable | Number of Cases of Genital Warts (NCGW) | |
|---|---|---|
| Female (N = 76) | Male (N = 110) | |
| Age group | ||
| < 18 | 1 (0.9) | 0 (0.0) |
| 18 - 24 | 30 (27.2) | 9 (11.8) |
| 25 - 34 | 58 (27.7) | 41 (53.9) |
| 35 - 44 | 18 (16.3) | 16 (21.0) |
| 45 - 54 | 3 (2.7) | 8 (10.5) |
| ≥ 55 | 0 (0.0) | 2 (2.6) |
| Marital statues | ||
| Single | 26 (23.6) | 34 (44.7) |
| Married | 78 (70.9) | 39 (51.3) |
| Divorced | 5 (4.5) | 3 (3.9) |
| Widow | 1 (0.9) | 0 (0.0) |
| Residence | ||
| Bushehr | 89 (80.9) | 60 (78.9) |
| Out of Bushehr | 21 (19.0) | 21 (16.0) |
| Referred | ||
| Yes | 62 (56.3) | 13 (17.1) |
| No | 48 (43.6) | 63 (82.8) |
| Place referred | ||
| Laboratory | 13 (20.9) | 3 (23.0) |
| Laser center | 2 (3.2) | 0 (0.0) |
| Obstetricians | 6 (9.6) | 0 (0.0) |
| Dermatologist | 42 (67.7) | 10 (76.9) |
| Urologist | 2 (3.2) | 0 (0.0) |
| History of infection | ||
| New | 90 (81.8) | 45 (67.1) |
| Recurrence | 18 (16.3) | 28 (41.7) |
| Resistant | 2 (1.8) | 3 (4.4) |
Most of the urban people were from the villages and towns around Bushehr, including Choghadak, AliShahr, Borazjan, Khormuj, Kangan, and Asaluyeh. About 71% of the infected men (54 cases) had warts on their penis, and about 42.7% of the infected women (47 cases) had warts on their perineum. According to the findings, the most widely used diagnostic method by physicians and midwives was physical examination (77.7%), and the most common therapeutic options were cryotherapy and electrocautery.
4.2. Description of GW History in the Past Month in the General Population
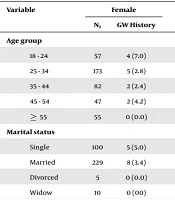
A total of 852 people living in Bushehr were included in the study. The response rate of women and men was 90% and 94%, respectively. The main reasons for non-response were unwillingness to participate or lack of time to fill the checklist. Most of the patients were in the age group of 18 to 24 years. There was a significant difference in women concerning age group (Table 2). In general, the estimated prevalence of GW was 2% in men (CI 95%: 1.9% - 2.1%) and 3.6% in women (CI 95%: 3.3% - 3.9%). There was no statistically significant difference concerning the prevalence of GW between the two genders.
| Variable | Female | P-Value | Male | P-Value | ||
|---|---|---|---|---|---|---|
| N1 | GW History | N2 | GW History | |||
| Age group | 0.032 | 0.738 | ||||
| 18 - 24 | 57 | 4 (7.0) | 72 | 3 (4.1) | ||
| 25 - 34 | 173 | 5 (2.8) | 154 | 5 (3.2) | ||
| 35 - 44 | 82 | 2 (2.4) | 86 | 2 (2.3) | ||
| 45 - 54 | 47 | 2 (4.2) | 54 | 1 (1.8) | ||
| ≥ 55 | 55 | 0 (0.0) | 72 | 0 (0.0) | ||
| Marital status | 0.220 | 0.957 | ||||
| Single | 100 | 5 (5.0) | 168 | 5 (2.9) | ||
| Married | 229 | 8 (3.4) | 261 | 6 (2.2) | ||
| Divorced | 5 | 0 (0.0) | 2 | 0 (0.0) | ||
| Widow | 10 | 0 (00) | 7 | 0 (0.0) | ||
| Education level | 0.443 | 0.944 | ||||
| Illiterate | 13 | 0 (00) | 16 | 0 (00) | ||
| Elementary | 27 | 0 (00) | 42 | 1 (2.3) | ||
| Under diploma | 40 | 3 (7.5) | 28 | 1 (3.5) | ||
| Diploma | 135 | 6 (4.4) | 132 | 3 (2.2) | ||
| Graduate | 199 | 4 (2.0) | 220 | 4 (1.8) | ||
Frequency of GW in the Population, Based on Demographic Characteristicsa
Of patients with GW, 22 (91.6%) reported that their lesions were located on the external parts of the genital tract, and 13 (54.1%) reported they got GW after using public swimming pools or epilation. About 7.6% of people with a history of GW mentioned traditional methods as the main source of treatment. About 66.6% of patients were referred to a physician for the treatment of their disease, of whom 5 (83.3%) men were referred to dermatologists and 6 (46.1%) women to gynecologists. Of the people who were referred to different medical wards, only 4 (20%) were referred to the laboratory to diagnose the HPV virus. Also, of all participants, 39 (4.5%) reported that they had had GW infection during the previous 6 months (Table 3).
| Variable | Female, No. (%) | Male, No. (%) |
|---|---|---|
| Wart lesions | ||
| Outside genital area | 13 (100) | 9 (81.1) |
| Inner parts of the genitals | 0 (0.0) | 0 (0.0) |
| Anus | 0 (0.0) | 2 (18.1) |
| Source of infection | ||
| Spouse | 0 (0.0) | 1 (9.0) |
| Girl/boy friend | 0 (0.0) | 2 (18.1) |
| Others (pool, waxing, etc.) | 5 (38.4) | 3 (27.2) |
| I do not know | 8 (61.5) | 5 (45.4) |
| The type of action taken after infection | ||
| No action | 2 (15.3) | 3 (27.2) |
| Self-medication using traditional medicines | 1 (7.6) | 0 (0.0) |
| Attending a pharmacy for over-the-counter medicine | 0 (0.0) | 2 (18.1) |
| Visiting physician | 10 (76.9) | 6 (54.5) |
| Referred to physician | ||
| Obstetrics and gynecologist | 7 (70.0) | 0 (0.0) |
| Dermatologist | 1 (10.0) | 6 (100) |
| General practitioner | 1 (10.0) | 0 (0.0) |
| Midwife | 1 (10.0) | 0 (0.0) |
| Referred to the laboratory | ||
| Yes | 2 (20.0) | 2 (33.3) |
| No | 8 (80.0) | 4 (66.6) |
Characteristics of People with a History of GW in the General Population
4.3. Estimation of NCGW in One Month by Multiplier Method
The estimated total number of GW in one month (i.e. patients referred to a general practitioner, dermatologist, gynecologist, midwife, urologist, and infectious disease specialist) was 258, 195, 77, 48, 22, 22, and 9, respectively, which there was a considerable gender difference.
The crude incidence rate of GW in general practitioner private clinics was estimated as 55 males (95% UCI, 27 to 167 individuals) and 22 females (95% UCI, 11 to 47 individuals). However, only 30.6% of general practitioners participated in the study. After matching these cases with participation percentages, 184 males with GW (95% UCI, 97 to 536 individuals) and 79 females with GW (95% UCI, 39 to 157 individuals) were reported (Table 4).
| Specialist | Female | Male | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| m: All People Referred to Private and Government Clinics | GW Positive Cases in People Who Went to Clinics (N) | All the Patients Who Reported the Disease Went to the Clinics | P1 | P2 | Number of Crude GW (S1) CI (95% UCI) | Percentage of Physician Participation | Number of Adjusted GW (S1) CI (95% UCI) | m: All People Referred to Private and Government Clinics | GW Positive Cases in People Who Went to Clinics (N) | All the Patients Who Reported the Disease Went to the Clinics | P1 | P2 | Number of Crude GW (S1) CI (95% UCI) | Percentage of Physician Participation | Number of Adjusted GW (S1) CI (95% UCI) | |
| Gynecologist | 6356 | 37 | 6 | 0.005 | 0.46 | 58 (30 - 124) | 76.9 | 77 (40 - 164) | - | - | - | - | - | 84 (41 - 242) | - | - |
| Dermatologist | 1110 | 20 | 1 | 0.018 | 0.07 | 32 (16-68) | 60 | 53 (27 - 112) | 907 | 32 | 5 | 0.035 | 0.45 | 18 (9 - 53) | 60 | 142 (69 - 421) |
| Urologist | 156 | 0 | 0 | 0.0 | 0.0 | 0 | 83.3 | 0 | 1042 | 7 | 1 | 0.006 | 0.09 | - | 83.3 | 22 (10 - 63) |
| Midwife | 1071 | 16 | 1 | 0.014 | 0.07 | 25 (13 - 54) | 52.3 | 48 (25 - 102) | - | - | - | - | - | 55 (27 - 167) | - | - |
| General Practitioner | 4415 | 14 | 1 | 0.003 | 0.07 | 22 (11 - 47) | 30.6 | 74 (39 - 157) | 2943 | 21 | 0 | 0.007 | 0 | 0 | 30.6 | 184 (91 - 536) |
| Infectious diseases specialist | 75 | 2 | 1 | 0.026 | 0.07 | 3 (1 - 6) | 33.3 | 9 (5 - 20) | 75 | 0 | 0 | 0 | 0 | 84 (41 - 242) | 33.3 | 0 |
5. Discussion
This cross-sectional study intended to estimate the numbers of cases of GW (NCGW) in the Bushehr adult population by the multiplier method. The estimated NCGW in one month using the adjusted multiplier method was 348 and 261 in men and women, respectively. Meanwhile, the numbers of cases reported by Bushehr University of Medical Sciences in June were 12 and 49 in men and women, respectively, which nearly is one-ninth of the estimated number in the present study.
The frequency of GW patients referred to clinics during the study period was estimated using the adjusted multiplier method, separated by the medical specialty, as follows: 42.3% for general practitioners, 31% for dermatologists, 12.6% for gynecologists 7.6% for midwives, 3.6% for urologists, and 1.4% for infectious disease specialists. A study conducted in India reported that most people with GW were referred to dermatologists (18). However, similar studies conducted in South Korea and Taiwan showed that most GW patients were referred to gynecologists (19, 20).
In the present study, we interviewed 852 people living in the city of Bushehr, the estimated prevalence of GW in men and women was 2% and 3.6%, respectively. According to a 2016 meta-analysis study, the overall prevalence of HPV in healthy, non-cancerous Iranian women was 9.4 % (95% CI: 6.8% - 12.02 %) (21). According to previous studies, HPV is more prevalent than GW, since only a limited number of HPV types cause GW. As the prevalence of HPV types 6 and 11 was estimated at nearly 50.2% (22) and since more than 90% of GW are caused by HPV types 6 and 11, if we consider healthy women as the representative of the overall society, GW prevalence in Iranian women can be estimated at about 4.2%, which is approximately equal to estimated prevalence in the present study (i.e. 3.6%). However, our estimated prevalence is higher than many other studies conducted on female populations. For instance, lower GW prevalence is estimated among women in India (1.17%) (18), South Korea (1.0%) (20), and Germany (0.7%) (23).
However, some previous studies in Iran have reported a higher prevalence for GW. For instance, a retrospective study by Yousefzadeh et al. (24), on 851 women aged 18 to 65 years, reported a GW frequency of 31.1%. Another study by Tabari et al. (25), in Babol City on spouses with GW, found that about 25% of spouses had GW. Another study reported the prevalence of low-risk HPV related to GW in women with uterine infections at 47.3% (26). Hence, the value reported in the present study is lower than other previous studies conducted in Iran. One clear reason for this difference is that the present study was conducted on a general population, while these other studies examined high-risk populations. In general, according to the latest systematic review, the prevalence of GW in the global general population typically varies from 0.13% to 0.20%. Also, no significant difference was observed in regional GW incidence and prevalence rates. However, studies conducted based on genital tract examination in the general population have reported relatively higher estimates (1% - 5%) (9).
The highest frequencies reported clinics (private and public) and the general population (self-reports) were in the age groups of 25 - 34 and 18 - 24 years, respectively. Similarly, other studies also mentioned these age groups as the most affected groups. For instance, in the study by Soori and Noroozi-Nejad (12) , the highest frequency of GW was in the age group of 20 - 30 years (47.3%), followed by 31 - 40 years (24.7%). The Center for Disease Control and Prevention (CDC) reported an association between age (under 30 years) and HPV infection rates (27). However, positive cases under the age of 18 have also previously been reported by physicians, which are considered to pose other social dangers. Despite higher incidence rates, the 18 - 24 age group tends to have the lowest rate of health care utilization often. It is therefore recommended that education and prevention programs should be directed towards younger age groups and adolescents.
The NCGW in Bushehr was found to be higher in men than women. Since private clinics reported fewer male patients than females, it may be inferred that men appear to pay less attention to this aspect of their health. According to a population survey, only half of the male patients who were referred to private clinics actually attended there; the rest either took no action to treat their illness or used traditional methods and/or directly referred to a pharmacy. However, more than two-thirds of women attended referrals to private clinics after contracting GW. A 2015 study in Iran found that women generally reported higher rates of sexually transmitted diseases compared to men, most likely due to their greater likelihood to seek out healthcare (15). In other studies, though, GW prevalence has been reported as higher in men than women (20).
According to the findings of the present study, less than half of private clinics referred GW patients to the laboratory, and less than one-third of the general population with GW reported that physicians referred them to the laboratory. A 2018 prospective study conducted on women with genital lesions in India found that 5% of patients with visible cysts were incorrectly diagnosed with GW (28). Therefore, a large number of people are potentially identified and then treated as GW patients without valid laboratory diagnoses, and this factor mistakenly led to increased prevalence of GW.
Since each private clinic had a different participation percentage, the best estimation for GW, using the multiplier method, was the number of positive cases (frequency). However, as the possibility of duplication can not be rejected, particularly in private clinics, it was not possible to report the overall S; for this reason, the S value was separately reported for each specialty and gender. We did our best to remove duplications (e.g., through comparing first and last names of each ID or national codes), but due to ethical issues, direct conversation with patients was not possible. We hope to increase the accuracy of data in the next steps, which will result in more reliable and accurate information on the prevalence and incidence of GW in the population of Bushehr. Other methods will also add to the accuracy, such as modeling or using laboratory data and information collected from laser centers.
One of the most important strengths of this study was using an indirect method and a combined technique (i.e., population-based and clinic-based), which probably has reduced the risk of bias and increased the generalizability of the findings. However, the authors suggest using modeling techniques in future studies to estimate the exact number of GW cases so that potential overlap be eliminated. The findings also suggest that the Ministry of Health should design and implement better strategies for reporting sexually transmitted diseases, including GW, to collect more accurate data. For example, applying incentive and punishment schemes may be a useful step towards this goal.
5.1. Limitations
One of the limitations of the present study was the possible reporting bias. GW is known to be a disease associated with social stigma, so asking people anonymously on the street was the best available option to collect data. For this reason, though, many people may refuse to disclose their GW, which leads to social desirability response bias. To minimize this bias, an attempt was made to develop a sincere, compassionate connection with the individuals surveyed, in order to ensure that their information remained confidential. Also, because GW may develop on the internal parts of the genital tract, people may not be aware of their infection, causing under-reporting. Conversely, people may report any genital lesions as GW, which can lead to over-reporting.
Another limitation of the current study is its relatively small sample size (852 subjects). Besides, participants were asked whether they had visited these private clinics in June due to GW infection. However, the total number of people who visited these clinics in the same period was 18,150. Probably the selection error has occurred; however, this is quite normal, as such limitations are observed in most self-reported studies (26).
The third limitation was that those with GW who were registered at a selected clinic were not necessarily the same people who reported visiting the selected clinics. Although it is difficult to confirm or disprove any of these assumptions, in the multiplier method, all of these assumptions are possible. To reduce these limitations, the authors suggest performing combined laboratory-clinical studies to examine GW, in addition to self-reported assessments.
5.2. Conclusions
In the present study, the multiplier method was used to investigate the prevalence of GW. The findings revealed that men are at increased risk of developing GW compared to women. However, using city-wide questionnaires and survey analysis, the prevalence was found to be higher in women than men. Despite these data, it remains important to pay attention to both sexes at all ages, especially adolescents and young people, in order to prevent and diagnose GW.
It worth noting that the number of GW cases in the population is likely to be significantly higher than what is reported previously. Due to data discrepancies between different departments, it is recommended that the STI reporting system be improved in order to obtain valid data, which is the basis for designing appropriate GW control and prevention programs.