1. Background
In December 2019, coronavirus disease 2019 (COVID-19) emerged in China and since then has affected many people worldwide. Studies show that the COVID-19 mortality rate (3.7%) is markedly higher than the influenza rate (1%) (1). The disease has spread with no definite geographical and age categories (2, 3), and acute respiratory distress syndrome (ARDS) is the main leading cause of death (4). Insufficient information about COVID-19 characteristics and behavioral patterns and the absence of specific treatments for the disease have made challenging conditions. The current suggested drugs in COVID-19 treatment are in the clinical trial phase, and Therefore supportive treatments have often been recommended (5, 6).
Limited data have been provided as predisposing factors, such as NSAID consumption (7). COVID-19 spread worldwide as an unexpected disaster and has remained a global public health concern thus far. It is crucial to investigate presumed related factors, predisposing conditions, and therapeutic or preventive strategies. It has been demonstrated that COVID-19 has a wide range of manifestations, including fever, cough, fatigue, sputum production, headache, hemostasis, acute cardiac injury, hypoxia, dyspnea, diarrhea, and ARDS. A severe immune reaction, both systemic and localized, breaks out after the infection (8, 9). The ABO blood group as a biomarker has been studied in Iran, although rarely, mostly for other diseases, rather than COVID-19. Studies demonstrate that some certain diseases are directly related to the ABO blood grouping system. For example, blood group O people are more susceptible to duodenal and type 2 diabetes, whereas blood group A people have a higher risk for gastric cancer. Studies have demonstrated some predisposing factors in susceptibility to COVID-19 and disease severity, such as age, gender, and co-morbidities.
2. Objectives
However, the influencing role of ABO-Rh has been rarely investigated in Iran. In this study, we investigated whether ABO blood groups have a significant association with COVID-19 infection.
3. Methods
Firstly, the study protocol was approved by the Ethics Committee of the Guilan University of Medical Sciences (GUMS) and registered (code: IR.GUMS.REC.1399.026). This retrospective descriptive multicenter study was conducted in academic, governmental, and private wards of hospitals in Rasht, Guilan Province, Iran. Retrospectively, all the files of the admitted patients with suspected COVID-19, in peak conditions of the disease, were reviewed between March 1 and May 30, 2020, using the Census method. Files with incomplete data were excluded. The required data, including epidemiological and clinical information and outcomes, were obtained from electronic records. Moreover, the blood group distribution in healthy and normal populations was extracted from the Guilan Blood Transfusion Department compared with COVID-19 cases. Finally, the archived data were analyzed with SPSS version 21.
4. Results
A total of 249 cases were analyzed, of whom 134 (53.8%) were male, and 115 (46.2%) were female, with the mean age of 57.53 ± 17.73 years. Of the cases, 109 were collected from governmental centers, and the rest were collected from private hospitals. The most common co-morbidities were diabetes with 71 (37.6%) cases, followed by cardiovascular diseases with 65 (34.4%) cases. The main symptom at the admission time was dyspnea with 170 (24.5%) cases followed by fever with 159 (22.9%) cases (Table 1). Of all the patients, 155 (62.2%) were discharged from the hospital, and the rest died. The most common blood group among our patients was O Rh-positive with 91 (36.5%) cases. Overall, only eight percent of the COVID-19 cases had an Rh-negative factor. Rh-positive was significantly higher among the male patients with 101 (44.1%) cases compared to their female counterparts (Table 2). No meaningful correlation was found between outcomes and blood groups regarding ABO types (P = 0.89) and Rh factors (P = 0.456) (Table 3).
| No. (%) | |
|---|---|
| Co-morbidities | |
| Cardiovascular | 65 (34.4) |
| Respiratory | 34 (18) |
| Cerebrovascular | 8 (4.2) |
| Diabetes | 71 (37.6) |
| Malignancy | 6 (3.2) |
| Immune deficiency | 5 (2.6) |
| Total | 189 (100) |
| Symptoms | |
| Fever | 159 (22.9%) |
| Cough | 129 (18.6%) |
| Dyspnea | 170 (24.5%) |
| Myalgia | 52 (7.5%) |
| Rhinorrhea | 6 (0.9%) |
| Headache | 20 (2.9%) |
| Nausea | 30 (4.3%) |
| Weakness | 83 (12%) |
| GI problems | 44 (6.3%) |
| Total | 693 (100%) |
The Prevalence of Co-Morbidities and Symptoms of COVID-19 Patients
| Blood Group | No. (%) |
|---|---|
| AB+ | 18 (7.2) |
| AB- | 4 (1.6) |
| B- | 3 (1.2) |
| B+ | 55 (22.2) |
| A- | 4 (1.6) |
| A+ | 65 (26.1) |
| O- | 9 (3.6) |
| O+ | 91 (36.5) |
| Total | 249 (100) |
The Prevalence of ABO Typing and Rh Factor of COVID-19 Patients
| Blood Group and Rh | Treatment Results, No. (%) | |
|---|---|---|
| Death | Cure | |
| AB- | 0 (0) | 4 (100) |
| AB+ | 7 (38.9) | 11 (61.1) |
| B- | 1 (33.3) | 2 (66.7) |
| B+ | 20 (36.4) | 35 (63.6) |
| A- | 1 (25) | 3 (75) |
| A+ | 27 (41.5) | 38 (58.5) |
| O- | 4 (44.4) | 5 (55.6) |
| O+ | 34 (37.4) | 57 (62.6) |
| Total | 94 (37.8) | 155 (62.2) |
The Relationship Between Blood Groups and the Outcome (P = 0.895)
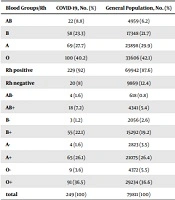
The ABO blood group distribution in the general population of Guilan Province is shown as A, B, AB, and O with 29.9%, 21.7%, 6.2%, and 42.1% of the population, respectively. However, the collected data of the 249 COVID-19 cases demonstrated a blood group distribution of A, B, AB, and O, with 69 (27.7%), 58 (23.3%), 22 (8.8%), and 100 (40.2%) cases, respectively (P = 0.301) (Table 4). The Rh-positive proportion was significantly higher in the COVID-19 cases than in the general population (P = 0.038) (Table 4).
| Blood Groups/Rh | COVID-19, No. (%) | General Population, No. (%) | P-Value |
|---|---|---|---|
| AB | 22 (8.8) | 4959 (6.2) | 0.301 |
| B | 58 (23.3) | 17348 (21.7) | |
| A | 69 (27.7) | 23898 (29.9) | |
| O | 100 (40.2) | 33606 (42.1) | |
| Rh positive | 229 (92) | 69942 (87.6) | 0.038 |
| Rh negative | 20 (8) | 9869 (12.4) | |
| AB- | 4 (1.6) | 618 (0.8) | 0.147 |
| AB+ | 18 (7.2) | 4341 (5.4) | |
| B- | 3 (1.2) | 2056 (2.6) | |
| B+ | 55 (22.1) | 15292 (19.2) | |
| A- | 4 (1.6) | 2823 (3.5) | |
| A+ | 65 (26.1) | 21075 (26.4) | |
| O- | 9 (3.6) | 4372 (5.5) | |
| O+ | 91 (36.5) | 29234 (36.6) | |
| total | 249 (100) | 79811 (100) |
The Comparison Between Blood Groups and Rh Factor in Patients and the General Population
5. Discussion
According to the current evidence, the susceptibility of some diseases, particularly viral infections, is significantly related to ABO-Rh blood types. This work was planned based on the supporting literature. In this study, we found that the positive Rh factor was much higher among COVID-19 cases than in healthy controls. In contrast, we did not observe any meaningful correlation between the ABO system and the increased risk of COVID-19 infection. In contrast to this work, Li et al. (10) from China reported that blood group A was more prone to SARS-COV-2 infection, while group O may play a protective role against the infection. Abdollahi et al. (11) from Iran conducted a study on 397 COVID-19 patients, and in contrast to our research, they demonstrated that blood group AB had a higher risk of the infection while they did not find a significant relationship regarding Rh factor. Cheng et al. (12) demonstrated that blood group O was associated with a lower SARS coronavirus. Batool et al. (13) from Pakistan reported that blood group O people were less likely to obtain transfusion-related infections, while blood group A people were significantly at a higher risk of HIV and hepatitis B. Jing et al. (14) showed that blood group B people had a lower risk of contracting HBV. Naseri et al. (15) from Iran showed the significant role of Rh factor differences in susceptibility to HBV and HCV infection following transfusion. However, they did not find any correlation between the ABO system and the increased infection risk (15).
In contrast, Shakeel et al. (16) did not report any association between blood groups and the viral hepatitis risk. Jana et al. (17) from Nepal did not support the previous studies and revealed a close statistical association between blood group O and susceptibility to HBV infection. As mentioned above, the available data on the issue are limited and controversial. ABO blood type and Rh factor distribution is not constant and depends on geographical area and ethnic group. The relationship between blood groups and susceptibility to COVID-19 has been so far rarely investigated and has yielded controversial results. It is not possible to compare the results and provide a challenging discussion due to the lack of similar studies, indicating the novelty of this work. In this study, individuals with the positive Rh factor might be at a higher risk for the infection when compared with the negative Rh factor. Thus, they have to strengthen their protection properties to decrease the chance of the infection recurring. It could not be concluded that Rh-positive people are resistant to the virus, and it is wise to provide adequate information regarding the best personal protection against COVID-19 infection for any blood group. We acknowledge that our findings could not be expressed as a guideline in clinical practice, but they encourage future studies.
5.1. Strengths
To our knowledge, this topic has been rarely investigated in Iran, specifically Guilan Province. Furthermore, it was a multicenter study conducted in academic, governmental, and private hospitals.
5.2. Limitations
Although we found valuable information regarding COVID-19, we acknowledge some expected limitations due to a retrospective study’s nature. In this research, non-symptomatic, infected cases or those with mild and transient symptoms who were not hospitalized were not enrolled in the survey. Furthermore, a remarkable number of files were excluded due to incomplete data and the high load of admitted cases during the study period. Also, we were not aware of the health conditions of our patients at the time of discharge. Indeed, we could report death and could not consider any difference between complete healthy people and patients discharged with lung fibrosis or renal failure, or other complications due to COVID-19 infection. Finally, this survey’s healthy control population lacked data regarding age, gender, and co-morbidities. Thus, a multi-variant analysis to adjust the effect of these parameters was not performed.
5.3. Conclusions
We found that the proportion of Rh-positive was significantly higher in COVID-19 cases than in healthy individuals. However, no correlation was observed regarding ABO typing. Individuals with Rh-negative should not take the risk of infection lightly. Further research is recommended to confirm these findings and discover other influencing factors and responsible molecular mechanisms.