1. Background
The coronavirus disease 2019 (COVID-19) has become a global health challenge in recent months, which has caused acute respiratory distress syndrome, respiratory and multiorgan failure, and an increase in the mortality rate of patients with metabolic syndrome (MetS) (1, 2). Nutrition is a determinant factor of health (3). A recent study suggested that malnutrition can affect immune cell metabolism and function (4). Nearly 33.6% of adults in Iran are suffering from MetS, which is possibly caused by following the western diet (WD) containing high amounts of saturated fat (HFD), refined carbohydrates and sugars, and low levels of fiber, unsaturated fats, and antioxidants (5, 6). Modern diet seems an important factor influencing the severity symptoms of COVID-19, through damaging the immune system (7, 8).
A recent systematic review introduced nutrients with probable antivirus properties (9). However, up to now, no research has evaluated the history of food intake and incidence of COVID-19 infection. Patients with history of diabetes, hypertension, and heart disease have a worse prognosis and are at greater risk for more severe symptoms and mortality due to COVID-19.
2. Methods
2.1. Study Design and Participants
We conducted retrospective case-control research on 98 patients with diabetes, hypertension, and/or heart disease, of whom 37 cases were positive for COVID-19 with clinical symptoms. A total of 37 COVID-19 positive patients that recurred, had laboratory-confirmed SARS-CoV-2 infection diagnosed by RT-PCR of nasopharyngeal swabs, and were hospitalized and/or referred to the outpatient clinic of Khatam Al-Anbia Hospital, Shushtar, Khuzestan province, Iran, between June and Aug 2020 were studied. We compared the case group with 61 patients with MetS exposed to SARS-CoV-2 and asymptotic (control group).
The control group was selected from physicians, nurses, and staff working in hospitals and medical centers and also close family members of infected patients with SARS-CoV-2 that encountered the virus without clinical symptoms of COVID-19.
The Medical Ethics Committee of the Faculty of Medical Sciences, Shushtar University of Medical Sciences, approved the research protocol according to the guidelines of the 2013 Helsinki Declaration (registration No.: IR.SHOUSHTAR.REC.1399.015).
Dietary intakes of participants were recorded using a Food Frequency Questionnaire (FFQ), which was designed and validated for the Iranian population (10). The frequency of food groups (based on the food pyramid) eating in the last year was asked in forms of daily, weekly, monthly, yearly, or never and then converted and reported to the unit per day.
2.2. Statistical Analyses
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request. Categorical variables were reported as frequency and percentages. Categorical variables were compared using the chi-square test. Continuous data with normal or non-normal distribution were described using mean ± standard deviation (mean ± SD) or median (25th and 75th percentile), respectively. The Mann-Whitney U test and independent t-test were used to compare continuous variables. Logistic regression was used to estimate the strength of the association between daily food groups and the odds ratios (ORs) of COVID-19. All statistical analyses were performed using Statistical Package for the Social Sciences) (SPSS) version 17.0 (SPSS Inc, Chicago, IL, USA). Two-sided P-values with P < 0.05 were considered statistically significant.
3. Results
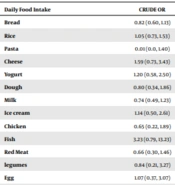
In our study, the case and control groups were matched in terms of body mass index (BMI), gender, and age. There was no significant difference in the demographic characteristics of participants between the two groups. The median BMI of all participants was 26.46 kg/m2. Also, 54% of all subjects had a consumption of nutritional supplements in the last six months, and there was no significant difference in the type of nutritional supplements between cases and controls. Table 1 demonstrates a comparison of daily food groups intake between two groups. Unexpectedly, we observed no significant difference in the median intake of food groups in the last year between MetS patients with clinical symptoms of COVID-19 compared to the controls. The results of the logistic regression models regarding the relationship between the intake of daily food groups and the occurrence of COVID-19 and OR and 95% confidence intervals (CI) are provided in Table 2. The CRUD OR showed that the adequate consumption of any food group was not associated with the occurrence of COVID-19.
| Characteristics | Asymptotic Group (Controls); n = 61 | COVID-19 Positive with Clinical Symptoms (Cases); n = 37 | P-Value b |
|---|---|---|---|
| Age (y) c | 33.62 (22, 59) | 32.86 (17, 51) | 0.60 |
| Weight (kg) c | 73.43 (43.5, 110.5) | 69.78 (50.5, 95.0) | 0.20 |
| Height (cm) d | 166.97 ± 9.29 | 164.47 ± 8.27 | 0.17 |
| BMI (kg/m2) c | 26.27 (16.94, 39.06) | 26.05 (15.40, 34.89) | 0.80 |
| Gender e | 0.59 | ||
| Female | 38 (62.3) | 25 (67.6) | |
| Male | 23 (37.7) | 12 (32.4) | |
| Physical activity e | 0.82 | ||
| Active | 6 (9.8) | 3 (8.1) | |
| Minimally active | 34 (55.8) | 23 (62.2) | |
| Inactive | 21 (34.4) | 11 (29.7) | |
| Educational level e | 0.17 | ||
| Elementary | 8 (13.1) | 10 (27) | |
| Diploma | 16 (26.2) | 6 (16.2) | |
| College | 37 (60.7) | 21 (56.8) | |
| Income e | 0.24 | ||
| Upper-middle | 15 (24.6) | 4 (10.8) | |
| Middle | 26 (42.6) | 18 (48.6) | |
| Lower-middle | 20 (32.8) | 15 (40.6) | |
| Marital status e | 0.59 | ||
| Married | 54 (88.5) | 34 (91.9) | |
| Single | 7 (11.5) | 3 (8.1) | |
| History of smoking e | 0.09 | ||
| No | 46 (75.41) | 33 (89.2) | |
| Yes | 15 (24.59) | 4 (10.8) | |
| Nutritional supplement consumption in last six months e | 0.28 | ||
| No | 29 (47.5) | 17 (45.9) | |
| Yes | |||
| Vitamin C | 3 (4.9) | 4 (10.8) | |
| Iron | 2 (3.3) | 4 (10.8) | |
| Vitamin D3 | 21 (34.4) | 11 (29.7) | |
| Multivitamin | 6 (9.9) | 1 (2.8) | |
| Daily food intake (per unit) c | |||
| Bread | 2.84 (1.0, 7.0) | 2.50 (1.0, 7.0) | 0.24 |
| Rice | 1.54 (0.14, 4.6) | 1.59 (0.14, 4.50) | 0.76 |
| Pasta | 0.21 (0.01, 0.90) | 0.11 (0.01, 0.40) | 0.07 |
| Cheese | 1.3 (0.0, 4.5) | 1.00 (0.07, 3.0) | 0.15 |
| Yogurt | 0.50 (0.0, 2.0) | 0.56 (0.0, 3.0) | 0.61 |
| Dough | 0.39 (0.0, 2.0) | 0.34 (0.0, 2.0) | 0.60 |
| Milk | 1.26 (0.0, 3.0) | 1.40 (0.0, 2.0) | 0.23 |
| Ice cream | 0.20 (0.0, 3.0) | 0.23 (0.0, 3.0) | 0.74 |
| Chicken | 0.60 (0.0, 2.0) | 0.54 (0.0, 2.0) | 0.44 |
| Fish | 0.23 (0.0, 0.85) | 0.33 (0.0, 0.85) | 0.10 |
| Red meat | 0.67 (0.0, 4.0) | 0.54 (0.0, 4.0) | 0.30 |
| legumes | 0.28 (0.0, 2.0) | 0.27 (0.0, 1.0) | 0.81 |
| Egg | 0.44 (0.0, 2.0) | 0.45 (0.0, 2.0) | 0.89 |
| Fruit | 1.85 (0.0, 4.0) | 1.7 (0.07, 4.0) | 0.71 |
| Vegetables | 1.40 (0.0, 5.50) | 1.12 (0.00, 5.50) | 0.38 |
Abbreviation: BMI, body mass index.
a Values are expressed as mean ± SD, median (25 th, 75 th percentiles) or No. (%).
b P-value < 0.05 was considered significant.
c Data were analyzed by Mann-Whitney U test.
d Data were analyzed by independent t- test.
e Data were analyzed by chi-square test.
| Daily Food Intake | Crude OR | P-Value | Adjusted OR Model 1 | P-Value |
|---|---|---|---|---|
| Bread | 0.82 (0.60, 1.13) | 0.24 | 0.82 (0.59, 1.12) | 0.22 |
| Rice | 1.05 (0.73, 1.53) | 0.76 | 1.10 (0.75, 1.59) | 0.61 |
| Pasta | 0.01 (0.0, 1.40) | 0.08 | 0.01 (0.0, 1.37) | 0.09 |
| Cheese | 1.59 (0.73, 3.43) | 0.23 | 1.50 (0.69, 3.26) | 0.30 |
| Yogurt | 1.20 (0.58, 2.50) | 0.60 | 1.08 (50, 2.37) | 0.83 |
| Dough | 0.80 (0.34, 1.86) | 0.61 | 0.80 (0.34, 1.89) | 0.62 |
| Milk | 0.74 (0.49, 1.23) | 0.16 | 0.73 (0.48, 1.12) | 0.15 |
| Ice cream | 1.14 (0.50, 2.61) | 0.74 | 1.14 (0.50, 2.62) | 0.74 |
| Chicken | 0.65 (0.22, 1.89) | 0.43 | 0.62 (0.21, 1.82) | 0.38 |
| Fish | 3.23 (0.79, 13.23) | 0.10 | 2.91 (0.70, 12.05) | 0.13 |
| Red meat | 0.66 (0.30, 1.46) | 0.31 | 076 (0.30, 1.88) | 0.55 |
| legumes | 0.84 (0.21, 3.27) | 0.81 | 0.83 (0.21, 1.32) | 0.80 |
| Egg | 1.07 (0.37, 3.07) | 0.89 | 1.31 (0.40, 4.22) | 0.64 |
| Fruit | 0.94 (0.69, 1.28) | 0.70 | 0.91 (0.95, 1.26) | 0.57 |
| Vegetables | 0.88 (0.65, 1.17) | 0.38 | 0.87 (0.65, 1.16) | 0.36 |
a OR was calculated by the logistic regression model. Model 1 adjusted for energy intake, BMI, and consumption of nutritional supplements.
4. Discussion
Our study is the first case-control research to compare dietary food intakes in MetS patients with clinical symptoms of COVID-19 and controls. The obtained data support that no specific food groups or nutritional supplements have an effect on the occurrence of COVID-19. However, a previously published opinion suggested mechanisms involved in the potential role of diet and nutrients in the prevention of COVID-19 via the strengthening of the immune system and reducing inflammation and oxidative stress (11, 12). The possible mechanisms that underlie such beneficial roles are not completely understood and other unknown factors may play a role.
Although dietary intake and nutritional supplements may offer excellent promise for preventing clinical symptoms of COVID-19, up to now, studies are not enough for recommending these supplements above the Recommended Dietary Allowances (RDA) for prevention and/or treatment of COVID19. SARS-CoV-2 is a new virus with an unknown function; hence, more studies are required to confirm these suggestions and provide hypotheses and opinions.