1. Background
In December 2019, a group of pneumonia-like illnesses with unknown origin was identified in Wuhan, Hubei province, China (1). A novel coronavirus (2019-nCov), named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was recognized as an organism in charge of the concerned diseases (2). The World Health Organization (WHO) called the disease caused by SARS-CoV-2 Coronavirus disease-2019 (COVID-19) (3). The virus spread globally and caused an ongoing pandemic quickly. By November 23, SARS-CoV-2 infected about 60 million people and killed above 1.4 million infected individuals (4).
A wide range of COVID-19 clinical manifestations, from symptom-free to death, has been introduced in previous studies (5, 6). Researchers from different countries are reporting newer symptoms continuously (7-9). Many infected individuals are supposed to be symptom-free (9); however, the most common symptoms are mild upper airway inflammation, including fever, dry cough, loss of smell, taste accompanied with fatigue, and muscle soreness (5, 10). Thrombosis occurs in some patients manifesting as CVA or MI (11). Other symptoms are less common (10, 12, 13). COVID-19 has been associated with various mortality rates worldwide, ranging from 0.17 to 1.7% (14). Heterogeneous mortality rates are attributed to age, gender, and comorbidities (15-18).
Individuals with underlying comorbidities present higher mortality rates and suffer from more severe symptoms, and longer hospital and ICU stay (19, 20). In this regard, diabetes mellitus (DM), hypertension, obesity, cardiovascular disorders, cancer, and chronic lung diseases are the most common comorbidities (6, 21-25). Moreover, COVID-19 patients are at an increased risk of developing cardiovascular disorders and thromboembolism (26, 27). In the US, black ethnicity represents a higher mortality rate considering race as a prognostic factor (28).
In Iran, as a country with high infection and mortality rates, there is no comprehensive evaluation of risk factors among a large sample.
2. Objectives
The present study aimed to evaluate the disease outcomes and severity according to different chronic underlying diseases in Iranian tertiary hospital cases.
3. Methods
3.1. Study Design and Participants
This retrospective cohort study included patients diagnosed with COVID-19, who were admitted to Baharloo Hospital, Tehran, Iran, from February 2020 to March 2020. In Baharloo Hospital, the patients were triaged mainly based on the WHO's case definition (29, 30); however, imaging criteria were also evaluated, as proposed by European Centre for Disease Control (ECDC), and physicians ordered chest computed tomography (CT) for probable cases (30, 31). Inclusion criteria were confirmed case of COVID-19, patients with available medical records, and those with informed consent. The COVID-19 diagnosis was confirmed by a positive SARS-CoV-2 RT-PCR using throat and nose swab from the upper respiratory tract sample or was clinically diagnosed based on lung imaging findings, especially chest CT scan ground glass pathognomonic features consistent with coronavirus pneumonia (31-33) when RT-PCR tests were not available. The admission criteria were as follows: (1) oxygen saturation (SO2) < 93% without supplementary oxygen, and (2) observing the COVID-19 symptoms on the patient's CT scan (i.e., the involvement of more than half of the lungs). However, we admitted patients with comorbidities if they had severe symptoms and signs of COVID-19 on their chest CT scan but not reduced SO2 levels.
3.2. Ethical Approvals, Registrations, and Patient Consents
All study procedures were approved by the Ethics Committee of the Tehran University of Medical Sciences (Code: IR.TUMS.VCR.REC.1399.209). The written informed consent form was obtained from all participants or their proxies.
3.3. Data Collection
Epidemiological, demographic characteristics, and the treatment and clinical outcomes of these patients were extracted from their medical records. Collected data included information about previous medical conditions, underlying diseases, ICU admission, and complications at the time of discharge and death.
3.4. Grading Criteria for COVID-19
The COVID-19 severity was classified according to the interim guidelines proposed by the WHO. The patients were classified into four categories (namely mild, moderate, severe, and critical) based on the patients' symptoms, laboratory results, and imaging findings at admission. Patients with slight clinical symptoms without imaging finding and those with fever or respiratory symptoms were considered as mild and moderate cases, respectively. Patients with respiratory distress and a respiratory rate > 30 times per minute, and fingertip blood oxygen saturation < 93% at rest were considered as severe cases. Patients were regarded as critical cases if they met one of the following prerequisites: shock, respiratory failure requiring mechanical ventilation, and other organ failure requiring ICU treatment.
3.5. Statistical Analysis
We calculated the number and percentage for the categorical variables and used chi-squared test to evaluate differences in categorical variables between the groups. Moreover, mean and standard deviation (SD) were presented for the numerical variables. Kolmogorov-Smirnov test was used to determine the normal distribution of numerical variables. We used parametric tests to evaluate the differences in the variables with normal distribution between the research groups. In contrast, we used nonparametric tests for variables with non-normal distribution. Statistical analysis was conducted using IBM SPSS software version 24 (IBM Corporation, Armonk, NY). Statistical significance was set as P < 0.05.
4. Results
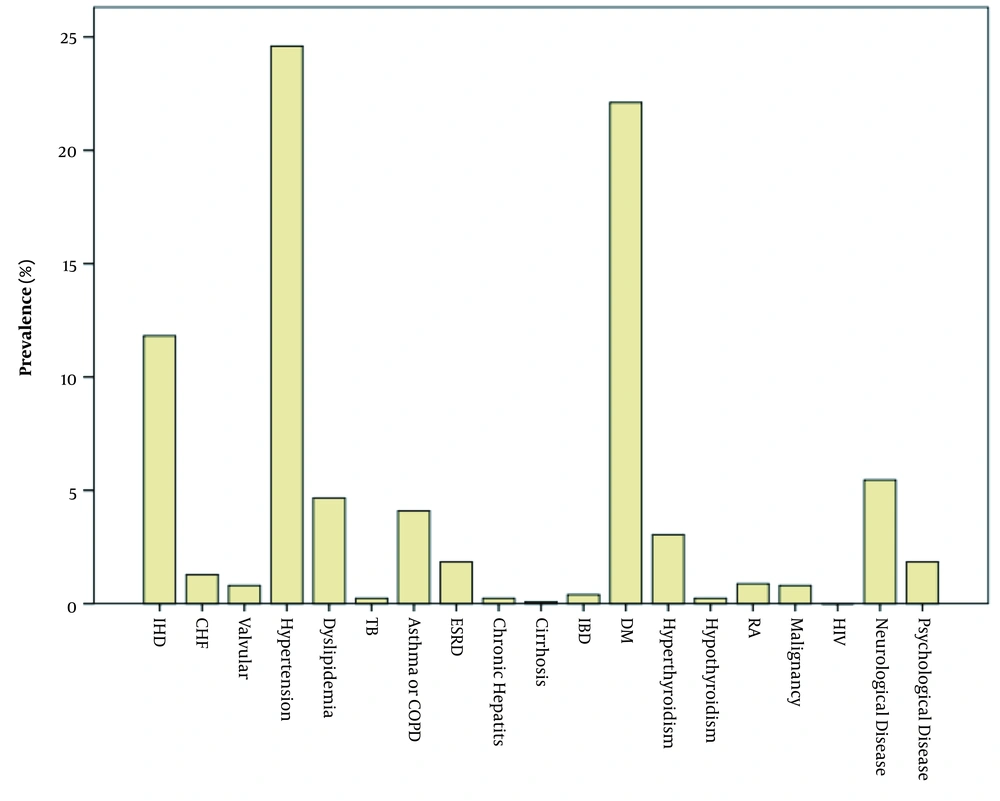
In this study, 1244 patients with a mean age of 53.29 ± 17.61 years were randomly selected and enrolled in the study. Out of the 1244 patients, there were 549 (44.1%) females and 695 (55.9%) males. Moreover, 731 (58.8%) cases were SARS-CoV-2 RT-PCR positive, and 513 (41.2%) patients were negative. Our data showed that 573 (46.1%) of patients had at least one comorbid condition, among which hypertension (24.6%), DM (22.1%), and ischemic heart disease (IHD) (11.8%) were the most common underlying diseases in these patients. On the other hand, 671 patients (53.9%) were healthy. Figure 1 shows the prevalence of underlying diseases in COVID-19 patients. The participants’ demographic characteristics, RT-PCR test result, and habitual history regarding their underlying diseases are presented in Table 1. We prescribed hydroxychloroquine and oseltamivir, lopinavir/ritonavir, naproxen and ribavirin as single or combination regimens for patients. Hypertension, dyslipidemia, and thyroidal diseases were significantly more common among females than males (P < 0.05). On the other hand, ESRD and DM were significantly more common among males (P < 0.05). In general, underlying diseases were significantly more common among females compared to males (50.1 vs. 42.9%; P = 0.007). The COVID-19 patients with an underlying disease were significantly younger compared to those with no underlying disease (6205 vs. 45.82; P < 0.001). Mean body mass index (BMI) was not significantly different in those with and without underlying diseases (P = 0.063). The COVID-19 patients with no underlying disease significantly had a more positive RT-PCR test compared to those with underlying diseases (64.2 vs. 52.4%; P < 0.001). Smoking, drug abuse, and alcohol consumption were not significantly different among the individuals with and without underlying diseases (P = 0.472).
| Variables | Cardiac Diseases | Pulmonary Diseases | Hypertension | DM | Dyslipidemia | Thyroid Disease | ESRD | Neurological Diseases | Psychiatric Diseases | Other | No Underlying Diseases |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | |||||||||||
| Female | 61 (38.1) | 27 (50) | 163 (53.3) | 135 (49.1) | 34 (58.6) | 25 (61) | 3 (13) | 35 (51.5) | 14 (60.9) | 15 (55.6) | 274 (40.8) |
| Male | 99 (61.9) | 27 (50) | 143 (46.7) | 140 (50.9) | 24 (41.4) | 16 (39) | 20 (87) | 33 (48.5) | 9 (39.1) | 12 (44.4) | 397 (59.2) |
| Age (y) [mean (%)] | 67.78 (12.93) | 64.02 (15.35) | 66.57 (12.7) | 62.27 (14.18) | 64.84 (13.61) | 51.73 (15.5) | 70.52 (13.47) | 64.01 (18.69) | 49.09 (15.68) | 58 (16.15) | 45.82 (15.73) |
| BMI [mean (%)] | 27.16 (3.98) | 27.24 (3.79) | 29.11 (21.02) | 27.78 (6.94) | 28.3 (4.41) | 29 (4.3) | 28.66 (4.67) | 26.42 (3.57) | 27.34 (3.51) | 27.28 (4.37) | 29.26 (38.94) |
| PCR | |||||||||||
| Positive | 84 (52.5) | 24 (44.4) | 165 (53.9) | 159 (57.8) | 34 (58.6) | 15 (36.6) | 13 (56.5) | 28 (41.2) | 4 (17.4) | 8 (29.6) | 431 (64.2) |
| Negative | 76 (47.5) | 30 (55.6) | 141 (46.1) | 116 (42.2) | 24 (41.4) | 26 (63.4) | 10 (43.5) | 40 (58.8) | 19 (82.6) | 19 (70.4) | 240 (35.8) |
| Smoking, alcohol consumption, or drug abuse | 19 (18.6) | 9 (22.5) | 19 (9.8) | 22 (12.6) | 7 (16.3) | 2 (6.5) | 4 (26.7) | 5 (11.1) | 4 (22.2) | 3 (15) | 41 (14) |
Participants’ Demographic Characteristics of Regarding Underlying Diseases a
Table 2 shows the severity of COVID-19 and mortality regarding the underlying diseases. Patients with underlying cardiac diseases, DM, hypertension, dyslipidemia, ESRD, neurological diseases, and psychological diseases experienced more severe types of COVID-19 compared to those without these diseases (P < 0.05). The mortality rate was significantly higher in those with cardiac diseases, pulmonary diseases, hypertension, DM, and ESRD (P < 0.05). After adjusting for age and gender, only DM (OR = 1.56, P = 0.045) and cardiac diseases (OR = 1.88, P = 0.01) were independent risk factors for mortality in the COVID-19 patients.
| Underlying Diseases | Severity | Mortality | |||||
|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | P-Value | Yes | No | P-Value | |
| Cardiac disease | 0.001 | 0.001 | |||||
| Yes | 93 (66.3) | 23 (16.4) | 24 (17.1) | 35 (21.9) | 125 (78.1) | ||
| No | 744 (84.3) | 91 (10.3) | 48 (5.4) | 72 (6.6) | 1012 (93.4) | ||
| Pulmonary disease | 0.798 | 0.036 | |||||
| Yes | 38 (82.6) | 4 (8.7) | 4 (8.7) | 9 (16.7) | 45 (83.3) | ||
| No | 799 (81.8) | 110 (11.3) | 68 (7) | 98 (8.2) | 1092 (91.8) | ||
| Hypertension | 0.001 | 0.001 | |||||
| Yes | 188 (69.2) | 51 (19) | 30 (11.2) | 44 (14.4) | 262 (85.6) | ||
| No | 649 (86.1) | 63 (8.4) | 42 (5.6) | 63 (6.7) | 875 (93.3) | ||
| DM | 0.001 | 0.001 | |||||
| Yes | 172 (72) | 43 (18) | 24 (10) | 41 (14.9) | 234 (85.1) | ||
| No | 665 (84.8) | 71 (9.1) | 48 (6.1) | 66 (6.8) | 03 (93.2) | ||
| Dyslipidemia | 0.029 | 0.109 | |||||
| Yes | 42 (80.8) | 10 (19.2) | - | 2 (3.4) | 56 (96.6) | ||
| No | 795 (81.9) | 104 (10.7) | 72 (7.4) | 105 (8.9) | 1081 (91.1) | ||
| Thyroidal disease | 0.524 | 0.476 | |||||
| Yes | 33 (84.6) | 5 (12.8) | 1 (2.6) | 4 (9.8) | 37 (90.2) | ||
| No | 804 (81.7) | 109 (11.1) | 71 (7.2) | 103 (8.6) | 1100 (91.4) | ||
| ESRD | 0.001 | 0.041 | |||||
| Yes | 12 (52.2) | 7 (30.4) | 4 (17.4) | 5 (21.7) | 18 (78.3) | ||
| No | 825 (82.5) | 107 (10.7) | 68 (6.8) | 102 (8.4) | 1119 (91.6) | ||
| Neurological disease | 0.001 | 0.223 | |||||
| Yes | 41 (65.1) | 15 (23.8) | 7 (11.1) | 8 (11.8) | 60 (88.2) | ||
| No | 796 (82.9) | 99 (10.3) | 65 (6.8) | 99 (8.4) | 1077 (91.6) | ||
| Psychological disease | 0.001 | 0.603 | |||||
| Yes | 11 (52.4) | 8 (38.1) | 2 (9.5) | 2 (8.7) | 21 (91.3) | ||
| No | 826 (82.4) | 106 (10.6) | 70 (7) | 105 (8.6) | 1116 (91.4) | ||
| Other | 0.288 | 0.197 | |||||
| Yes | 17 (70.8) | 5 (20.8) | 2 (8.3) | 4 (14.8) | 23 (85.2) | ||
| No | 820 (82.1) | 109 (10.9) | 70 (7) | 103 (8.5) | 1114 (91.5) | ||
Severity and Mortality of Underlying Diseases a
5. Discussion
The present retrospective cohort study on 1244 COVID-19 cases provides information about the COVID-19 disease and its outbreak in Iran. Our findings suggested that around 57.8 % of individuals infected with COVID-19 had a severe disease; hence, a majority of cases needed to be hospitalized. As the Baharloo Hospital is a referral center in Tehran, a similar trend in the general population can be concluded. In our study population, there were 573 patients with at least one kind of co-existing chronic disease. The mean age of the patients was 53.29 years, indicating that individuals of all ages are susceptible to the virus. Male patients were more frequent than females, which is consistent with other studies (6, 15). This difference can be attributed to their different lifestyles, especially smoking. Cai indicated that smoking could increase angiotensin-converting enzyme 2 (ACE2) expression in the respiratory system (34). ACE2 is proved to be a receptor for SARS-CoV-2 (31). Moreover, the X chromosome and sex hormone play a critical role in innate and adaptive immunity, which can expose susceptible females to less infection (35).
The clinical diagnosis and CT scan results consistent with COVID-19 were used for patient admission. The CT scan results had greater sensitivity than the RT-PCR test. Our RT-PCR results were only positive in 58.8% of cases admitted to our center. The low rate of positive tests can be attributed to several reasons. First, the complicated sampling technique and the type of sample taken by the medical staff's limited expertise and the overwhelming condition during the outbreak could have affected the accuracy of the samples sent to the PCR laboratory. Second, the number of samples and tests from each patient could have influenced the RT-PCR test's sensitivity (36). Under this condition, the hospitals should not focus on the findings of the RT-PCR test to diagnose and treat the COVID-19 patients. Medical examination, including signs and symptoms, low oxygen saturation, and pulmonary involvement pattern in CT scan, was deemed adequate to support and treat patients, especially during the epidemic (37).
The prevalence of the population and the approximate number of individuals with chronic medical disorders provide planning details and have implications for allocating health care services. The occurrence of a pre-existing chronic condition is identified as a potential risk factor for the increased severity of SARS-CoV-2 infection. Our findings indicated that patients with chronic underlying disease experienced more severe forms of COVID-19. Moreover, the mortality rate tends to be higher in these patients. This finding of the present research was compatible with other studies (7, 38, 39). Surprisingly, there was no correlation between pulmonary disease and COVID-19 severity; this can be due to the small number of patients with pulmonary diseases. Mertz et al. demonstrated that in patients with comorbidities, the risk of death from influenza was significantly higher than the risk in individuals with no comorbidities (40). Since SARS-CoV-2 is a recently discovered pathogen, there is no pre-existing immunity to SARS-CoV-2 in human population. To date, there is no definite treatment to stop or minimize the spread of this virus. These complexities make the disease more dangerous for susceptible members of the population, including those with immune disorders, co-existing morbidity, and elderlies. In a systematic review by Javanmardi et al., the most prevalent underlying conditions in hospitalized patients with COVID-19 were hypertension, cardiovascular disease, diabetes, kidney disease, smoking, and COPD (17). Among the aforementioned comorbidities, cardiovascular disease was the most frequent and put patients at higher mortality rates. This might be due to increasing pro-inflammatory cytokines contributing to poorer immune function (41). In our study, hypertension, DM, and IHD were the three most common co-existing chronic diseases and had a significant impact on the disease severity and its mortality rate.
The mechanism underlying comorbid chronic diseases and the COVID-19 severity is poorly understood. However, for patients with cardiovascular diseases, ACE2, which mediates the SARS-CoV-2 to the lung, is also expressed in the cardiovascular system and can directly affect the cardiac function (42). Drug-induced cardiotoxicity is another mechanism exposing patients with cardiovascular disease at a higher risk of severe forms of COVID-19 (43). Moreover, immunohistochemistry has demonstrated that SARS-CoV-2 antigen accumulates in renal tubules with severe acute tubular necrosis, however, without indication of glomerular pathology or infiltration of tubulointerstitial lymphocytes (44). SARS-CoV-2 infection can cause a cytokine storm, which releases high levels of various cytokines and chemokines, including IL-2, IL-7, and IL-10 and hurts patients’ tissues (45). Yang et al. showed that ACE2 is also expressed in pancreatic islet cells targeted by the virus (46). Furthermore, ACE2 knockout mice have compromised B-cell pancreatic activity, implying a potential link between infection with SARS-CoV-2 and diabetes (47). Finally, through a compromised immune system, multiple chronic comorbidities, including hypertension, cardiovascular disease, chronic kidney disease, and diabetes, make the affected organs and tissues susceptible to the virus (48).
To the best of our knowledge, this study with large sample size is among the first reports in Iran. While the sample size in this study is a major advantage, more detailed information on patients, especially clinical outcomes, was not available at the time of review. Notably, this can limit the results of this data. However, the data provides information about the epidemiological characteristics of the COVID-19 cases in Tehran, Iran. Further research in outpatient, primary care, or community settings will provide a comprehensive understanding of clinical diagnosis, risk factors, and the scale of clinical severity under the same condition.
Further attempts should be made to resolve the afore limitation. Rapid, accurate, and practicable diagnostic tests are essential, however diagnostics selectionis based on physicians' clinical logic. Monitoring the disease and its epidemiological features, including virulence, host tolerance, transmissibility, and pathogenicity, requires careful national surveillance. At the national, regional, and global levels, efforts and interventions need to be made to interrupt the disease transmission chain.
In conclusion, the present findings demonstrate the remarkable impact of chronic underlying diseases on the risk of mortality and disease severity in patients with COVID-19, as previously stated in other reports. Hence, it is recommended to take prevention strategies more seriously. Regarding medical care services, it is also important to pay particular attention to patients with underlying diseases. As COVID-19 is known to be a global health threat, more comprehensive investigations are still suggested.