1. Background
The novel coronavirus, SARS-CoV-2, has caused a pandemic of a life-threatening, multi-organ disease named COVID-19 (1). Its outbreak began in late 2019 and early 2020 in Wuhan, China, affecting many people and then spreading rapidly worldwide (2). Evidence suggests that COVID-19 patients are subject to significant risks of thromboembolic complications, mainly affecting their intravenous systems and sometimes arterial vascular systems (3). Although the pathogenic mechanism of COVID-19 is not completely clear (4), it seems that coagulopathy is one of the severe problems COVID-19 patients grapple with (5). Based on preliminary investigations, thrombocytopenia (36.2%) and elevated D-dimer level (46.4%) are usually observed in COVID-19 patients (6). Nevertheless, the prevalence of these two conditions is even higher in patients affected by severe forms of the disease (57.7 and 59.6%, respectively) (6). The studies have shown that COVID-19 patients are subject to higher risks of diffuse intravascular coagulation (DIC) (6-8). Elevated D-dimer level, prolonged prothrombin, and increased fibrin degradation products have been associated with the poor prognosis of COVID-19 patients (8).
2. Objectives
The present study aimed to investigate the occurrence of coagulation disorders in COVID-19 patients and determine its relationship with the disease outcome.
3. Methods
This cross-sectional study was conducted on 106 COVID-19 patients hospitalized in Imam Khomeini Hospital, Ardabil, Iran. The patients’ affliction with COVID-19 was diagnosed and confirmed based on the results of RT-PCR, throat swab, and lung CT scan. On the first day of hospitalization, written consent was obtained from the patients before their demographic information, including age, gender, clinical symptoms, comorbidities, and history of smoking, was recorded. After the preliminary completion of the information forms, 3 cc of intravenous blood was sampled from each patient. Then, serum was separated to check the patients’ INR, PT, CBC, and D-dimer levels. Next, the patients were investigated and monitored for their clinical parameters, response to treatment, the need for ICU stay, percentage of arterial blood oxygen saturation, mortality, and related complications. The clinical information and test results were recorded in checklists. We excluded patients with a history of rheumatologic diseases, ischemic heart diseases, malignancies, organ transplantation, chronic liver diseases, kidney diseases, hemoglobinopathy, blood disorders, and those on anticoagulation drugs.
3.1. Ethical Approval
The Research Ethics Committee of Ardabil University of Medical Sciences approved the current study (IR.ARUMS.REC.1399.087).
3.2. Statistical Analysis
All statistical analyses were done using IBM SPSS software (version 24) (IBM SPSS Statistics, Armonk, USA). The normality of variables was proved using the Kolmogorov-Smirnov test. The Mann-Whitney U test was employed to compare variables with non-normal distribution. The predictive value of serum D-dimer level was determined via measuring the area under receiver operating characteristic (AUROC) curve. Finally, the optimal threshold value was obtained via the Youden index. A P value of less than 0.05 was regarded as statistically significant.
4. Results
Of 106 COVID-19 patients, 69 were discharged from the hospital, while 37 cases died. The mean age of the patients was 58.99 ± 15.94 years, and 56.6% were males. Moreover, the patients’ average length of hospital stay was 11.79 ± 8.22 days. Based on the disease outcome, the patients were divided into two groups: survived and deceased (Table 1). The demographic information and comorbidities of each group are represented in Table 1.
| Variables | All Patients (n = 106) | Non-survivors (n = 37) | Survivors (n = 69) | P Value |
|---|---|---|---|---|
| Age (y) | 58.99 ± 15.94 | 60.09 ± 17.12 | 58.43 ± 15.41 | 0.62 |
| Sex | 0.98 | |||
| Male | 60 (56.6) | 21 (56.8) | 39 (56.5) | |
| Female | 46 (43.4) | 16 (43.2) | 30 (43.5) | |
| Saturation (%) | < 0.001 b | |||
| > 93 | 23 (21.7) | 18 (48.6) | 5 (7.2) | |
| < 93 | 83 (78.3) | 19 (51.4) | 64 (92.8) | |
| Hospital stay (days) | 11.79 ± 8.22 | 11.03 ± 10.7 | 12.06 ± 6.59 | 0.65 |
| Pulmonary involvement | < 0.001 b | |||
| Low | 26 (24.5) | 4 (3.8) | 22 (20.8) | |
| Moderate | 35 (33) | 8 (7.5) | 27 (25.5) | |
| Severe | 45 (42.5) | 25 (23.6) | 20 (18.9) |
Demographic Characteristics, Underlying Disease, and Length of Hospital Stay of Patients by Groups a
The results showed a significant difference between the two groups regarding D-dimer, LDH, PT, and INR levels. However, the differences between the two groups were statistically insignificant in terms of hemoglobin level and platelet count. More specifically, serum D-dimer level, LDH, PT, and INR were significantly higher in deceased patients than surviving patients (Table 2).
| Variables | All Patients (n= 106) | Survivors (n= 37) | Non-survivors (n= 69) | P Value b |
|---|---|---|---|---|
| White Blood Cell | 7899.06 ± 4264.57 | 9589.19 ± 5362.35 | 6999.75 ± 3235.93 | 0.01 c |
| Hemoglobin | 13.46 ± 1.99 | 13.66 ± 2.23 | 13.36 ± 1.86 | 0.45 |
| Platelet | 200.15 ± 82.85 | 198.41 ± 84.44 | 201.09 ± 82.59 | 0.87 |
| D-dimer | 941.43 ± 958.90 | 1340.59 ± 915.48 | 727.39 ± 918.10 | < 0.001 c |
| PT | 13.36 ± 1.83 | 13.79 ± 1.91 | 13.13 ± 1.76 | 0.01 c |
| INR | 1.18 ± 0.29 | 1.24 ± 0.28 | 1.14 ± 0.28 | 0.03 c |
| PTT | 35.33 ± 7.34 | 35.65 ± 6.05 | 35.16 ± 7.99 | 0.625 |
| LDH | 813.19 ± 586.65 | 881.89 ± 414.06 | 719.19 ± 290.11 | 0.029 c |
Laboratory Findings of Patients by Groups a
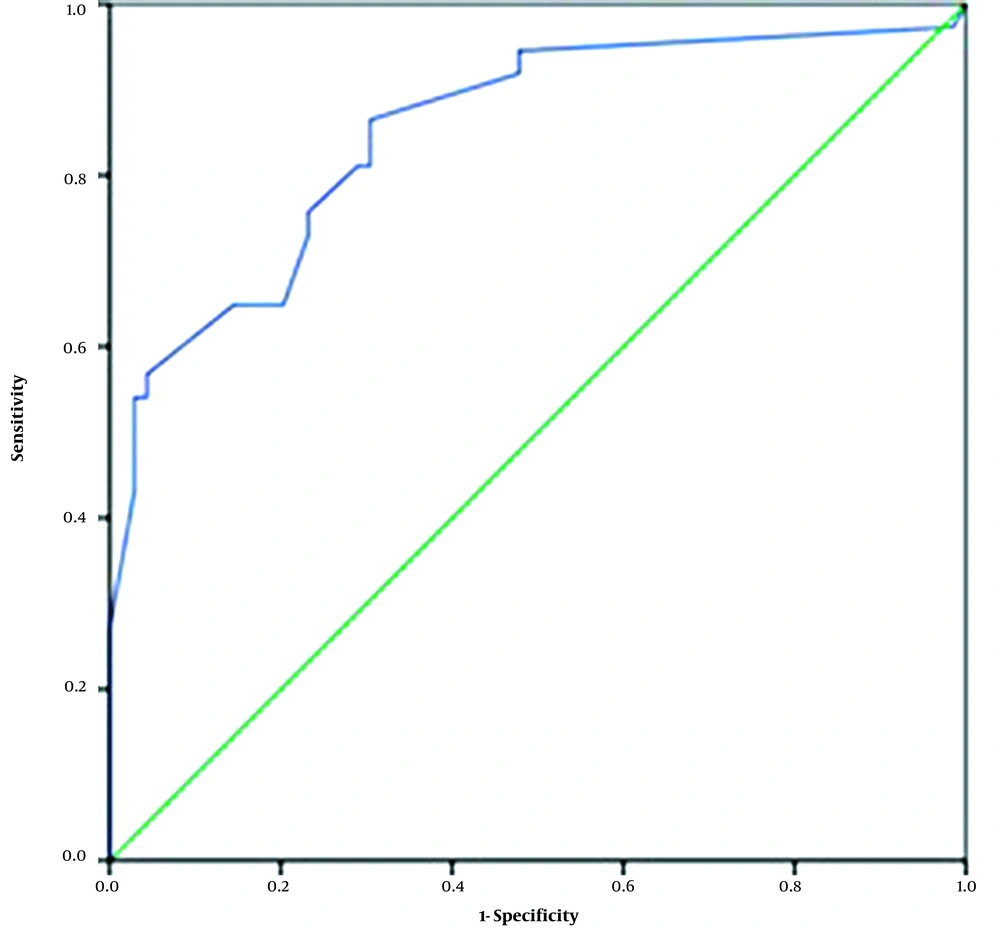
Binary logistic regression was applied to determine the relationship between mortality and study variables, as presented in Table 3. As can be seen, serum D-dimer level was a significant predictor of mortality such that each unit increase in D-dimer level increased mortality risk by 0.99% (OR = 0.994; 95% CI: 0.992 - 0.997). The receiver operating characteristic (ROC) curve was used to determine the cutoff point of serum D-dimer level to predict mortality. As shown in Figure 1, the area under the ROC curve was obtained to be 85% for D-dimer. Besides, its cutoff point was determined to be 450 μg/dL with a sensitivity of 98% and specificity of 97%.
| Variables | Sig. | Exp (B) | 95% CI for EXP (B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| PT | 0.772 | 1.081 | 0.641 | 1.823 |
| INR | 0.297 | 0.190 | 0.008 | 4.320 |
| D-dimer | 0.000 a | 0.994 | 0.992 | 0.997 |
| LDH | 0.986 | 1.000 | 0.998 | 1.002 |
Results of Logistic Regression to Determine the Relationship Between Study Variables and Disease Outcome a
5. Discussion
This study was conducted to investigate the occurrence of coagulation disorders in COVID-19 patients and determine its relationship with the disease outcome. The results indicated that the prevalence of coagulation disorders was significantly higher in deceased patients than in surviving ones. Moreover, a positive correlation was observed between serum D-dimer level and mortality risk. Therefore, the level of D-dimer can be used as a prognostic risk factor in COVID-19 patients. In our study, the cause of patient death was severe pulmonary involvement and hypoxia, although myocarditis, sepsis, Pulmonary Thromboembolism (PTE), and multiple organ failure due to COVID-19 could also increase mortality.
Tang et al. attempted to determine the poor prognosis of COVID-19 patients based on the aberrant coagulation parameters in the first 28 days of hospitalization. Their findings revealed that during these 28 days, elevated D-dimer level, prolonged PT, and higher age were associated with the highest levels of mortality, while higher platelet counts were associated with the lowest levels of mortality (8). The findings of their study regarding the relationship of elevated D-dimer, PT, and age with mortality are consistent with the findings of the present study.
A meta-analytic study by Lippi et al. demonstrated that the platelet count in COVID-19 patients was significantly lower than normal. Moreover, they found that the risk of being afflicted with thrombocytopenia was five times more in patients suffering from severe COVID-29 than in normal patients (9). However, this finding is not in line with our findings. This inconsistency might be related to that we checked the patients' platelet counts only at the beginning of the study, while the patients might develop thrombocytopenia during hospitalization, which was not investigated in the current study.
In Brazil, Dolhnikoff et al. conducted a pathological study on 10 deceased patients (five males and five females with a mean age of 67.8 years). Pathological observations were indicative of a higher incidence of coagulation disorders among patients in critical condition. They also showed that renal microthrombosis was more prevalent among these patients (10).
In a retrospective study, with findings in line with ours, Yin et al. compared the coagulation status and clinical characteristics of patients with SARS-CoV-2-induced severe pneumonia (COVID-19 group) and patients with non-SARS-CoV-2-induced severe pneumonia (non-COVID-19 group). They observed that coagulation disorders usually accompanied severe COVID-19. Therefore, they suggested that higher levels of D-dimer could help decide on the initiation of anticoagulation therapy (11).
In the present study, 87% of the patients had elevated D-dimer levels. In line with our finding, Yao et al. (12) observed elevated D-dimer levels in 74.6% of the patients. Besides, the D-dimer level significantly increased as the severity of COVID-19 symptoms increased. The clinical observations and CT results confirmed this finding. In their study, the hospital mortality rate was 6.9%.
Furthermore, the mean D-dimer level was significantly higher in deceased patients than surviving patients. Moreover, the hospital mortality rate was predicted based on the D-dimer level of higher than 2.14 mg/L, with a sensitivity of 88.2% and specificity of 71.3% (12). This D-dimer level in the current study was 450 μg/dL. Thrombocytopenia and elevated D-dimer levels can be explained by the over-activation of coagulation cascades and platelets. Viral infections induce a systemic inflammatory response and cause an imbalance in procoagulant and anticoagulant hemostatic mechanisms (13). Multiple pathogenic mechanisms are involved, including endothelial dysfunction, increased von Willebrand factor, Toll-like receptor activation, and tissue factor pathway activation (13). After recognizing the antigen, platelets become activated and interact with it. White blood cells are also activated, and clot formation is accelerated (14). Platelets are the primary mediators of inflammation that detect infectious agents via perceiving the interaction of cell-surface receptors and pathogens as well as the activation of and interaction among macrophages, monocytes, endothelial cells, platelets, and lymphocytes. Therefore, they play an essential role in the prognosis of viral infections (15).
5.1. Conclusions
The present study indicated that coagulation disorders were more prevalent in patients with severe COVID-19. It was also found that serum D-dimer level was positively associated with mortality. Although coagulation disorders in COVID-19 patients are still being investigated, the evidence thus far suggests that thrombotic coagulation disorder is quite prevalent in severe COVID-19. The results also indicated that D-dimer has higher sensitivity than other coagulation markers in severity. As bleeding is not as common as thrombotic events, anticoagulant therapy is recommended.