1. Background
The COVID-19 outbreak originated in Wuhan City, China, in December 2019 (1). Although COVID-19 preferentially affects the respiratory system, it has been demonstrated that coronaviruses (especially β-coronaviruses to which COVID-19 belongs) do not limit their presence to the respiratory tract and frequently invade the nervous system (2-5).
SARS-CoV-2 infection is associated with a wide spectrum of neurological syndromes affecting the entire neuraxis, including delirium or encephalopathy, headache, agitation, vertigo, cerebrovascular events, meningitis, encephalitis, impaired sense of smell or taste, peripheral nerves involvement, and so forth (6-12). In many cases, neurological manifestations have been reported even without respiratory symptoms (13).
2. Objectives
We aimed to report the frequency and type of neurological manifestations in patients with COVID-19 based on all consecutive adult hospitalized patients in our center.
3. Methods
In this retrospective, prospective observational cohort study, data were collected from February to July 2020 at Bu-Ali Sina University Hospital, Sari, Iran. The study included 420 consecutive hospitalized patients with a laboratory-confirmed diagnosis of SARS-CoV-2 infection.
Clinical data were retrospectively extracted from patients’ medical files from February to April 2020. Data on all neurologic symptoms were checked by 2 neurology residents. In the case of incomplete or doubtful data, symptoms were rechecked by telephone call. Neurology residents recorded patient symptoms and signs through face-to-face interviews and physical examinations. All hospitalized patients with positive SARS-CoV-2 RNA polymerase chain reaction (PCR) from nasopharyngeal swabs were included in the study.
Demographic data on age, sex, past medical history, comorbidities (hypertension, diabetes, cardiac disease, cerebrovascular disease (CVD), malignancy, chronic kidney disease, liver dysfunction, and so forth), clinical symptoms at the onset of the disease (fever, cough, anorexia, nausea/vomiting, diarrhea, sore throat, abdominal pain, dizziness, paresthesia, headache, and other nervous system symptoms), laboratory findings, chest computed tomography (CT) scan, and neuroimaging (brain CT or magnetic resonance imaging (MRI) if available) were recorded.
Neurological manifestations fell into 5 categories: nonspecific central nervous system (CNS) manifestations (dizziness, headache, impaired consciousness, seizure, and myalgia), acute CVD, meningitis/encephalitis, peripheral nervous system manifestations (taste impairment, smell impairment, vision impairment, and Guillain-Barre syndrome), and inflammatory disorders (myelitis and acute disseminated encephalomyelitis). If patients suffered from one of the nonspecific signs but documented any other categories, they were classified into a specific category.
Before enrollment, verbal consent for retrospective cases by telephone call or written consent for prospective cases was obtained from patients or an accompanying relative for patients who could not give consent. The study was performed in accordance with the principles of the Declaration of Helsinki. This study was approved by the Ethics Committee of Mazandaran University of Medical Science (code: IR.MAZUMS.REC.1399.124).
3.1. Statistical Analysis
All analyses were performed using SPSS version 24.0 (SPSS Inc, Chicago, IL, USA). Quantitative data were presented as mean ± SD, and qualitative data were presented as frequency and percentage. An independent sample t test was used to assess quantitative data, and a chi-squared test was applied to relate categorical variables and qualitative data. P values less than 0.05 were considered statistically significant.
4. Results
A total of 420 patients were admitted to the hospital with confirmed COVID-19 infection from April to July 2020. Of the 420 patients admitted due to COVID-19 infection, 221 (52.6%) were male, and 199 (47.4%) were female. The mean age of patients was 58.26 ± 16.89 (min = 15, max = 97). Thirty-seven patients (8.8%) reported a recent travel history, and 92 patients (22.1%) reported close contact with a patient infected with COVID-19. The most common systemic comorbidities were hypertension (39.8%), diabetes mellitus (35.5%), and heart disease (19.76%). Table 1 shows baseline comorbidities in our COVID-19 patients.
| Variables | Male | Female | All Patients |
|---|---|---|---|
| Hypertension | 66 (30) | 101 (51.5) | 167 (39.7) |
| Diabetes mellitus | 60 (27.3) | 89 (45.2) | 149 (35.4) |
| Heart disease | 44 (20) | 39 (19.9) | 83 (19.7) |
| Kidney disease | 9 (4.1) | 11 (5.6) | 20 (2.6) |
| Other diseases | 3 (1.5) | 6 (3) | 8 (1.9) |
| No comorbidity | 126 (57.3) | 85 (43.4) | 211 (50.23) |
Comorbidity and Past Medical History of Hospitalized Patients with COVID-19 a
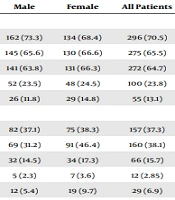
In terms of clinical symptoms, the most common manifestations at the onset of the disease were fever (70.5%), dry cough (64.76%), and difficulty breathing (65.46%). Of the 420 patients hospitalized with COVID-19, 282 (67%) showed some form of neurological symptoms. Concerning nonspecific neurological symptoms, 203 (48.33%) patients reported headache, dizziness, impaired consciousness, and seizure. Seizures happened in 12 patients (2.85%), of whom 3 patients were identified with previous epilepsy. One of them was complicated by status epilepticus, and two of them were after intracranial hemorrhages. Seizures were generalized tonic and clonic in all patients. Among patients hospitalized with COVID-19, 35 (8.3%) had acute CVD, of whom 14 (3.33%) patients were hemorrhagic, and 21 (5%) patients had an ischemic stroke. Two patients had encephalitis (the RNA of SARS-CoV-2 was detected in cerebrospinal fluid (CSF), 1 patient had myelitis, and 83 (19.76%) patients had peripheral nervous system manifestations, including taste impairment, smell impairment, facial paresis, limb paresthesia, and Guillain-Barre syndrome (one patient). Table 2 represents the clinical manifestations of our COVID-19 patients.
| Clinical Symptoms | Male | Female | All Patients |
|---|---|---|---|
| General symptoms | |||
| Fever or chills | 162 (73.3) | 134 (68.4) | 296 (70.5) |
| Difficulty breathing | 145 (65.6) | 130 (66.6) | 275 (65.5) |
| Dry cough | 141 (63.8) | 131 (66.3) | 272 (64.7) |
| Nausea or vomiting | 52 (23.5) | 48 (24.5) | 100 (23.8) |
| Diarrhea | 26 (11.8) | 29 (14.8) | 55 (13.1) |
| Nonspecific CNS symptoms | |||
| Muscle or body aches | 82 (37.1) | 75 (38.3) | 157 (37.3) |
| Headache | 69 (31.2) | 91 (46.4) | 160 (38.1) |
| Dizziness | 32 (14.5) | 34 (17.3) | 66 (15.7) |
| Seizure | 5 (2.3) | 7 (3.6) | 12 (2.85) |
| Impaired consciousness | 12 (5.4) | 19 (9.7) | 29 (6.9) |
| Acute CVD | |||
| Ischemic stroke | 10 (4.5) | 11 (5.5) | 21 (5) |
| Hemorrhagic stroke | 8 (3.6) | 6 (3.01) | 14 (3.3) |
| Meningitis/encephalitis | 2 (0.9) | 0 | 2 (0.4) |
| PNS manifestations | |||
| Loss of taste or smell | 30 (13.6) | 32 (16.3) | 62 (14.7) |
| Paresthesia | 3 (1.4) | 6 (3.1) | 9 (2.1) |
| Inflammatory disorders | 0 | 1 (0.5) | 1 (0.2) |
The Clinical Manifestations of Patients with COVID-19
Of the 35 patients with acute CVD, 29 (82.9%) had hypertension disease (P = 0.0001), and 12 (34.03%) had diabetes mellitus (P = 0.50). Also, 16 (45.7%) patients had previous heart disease (P = 0.0001). The mean age of patients with CVD was 71.96 ± 14.45 years, which there was a significant difference compared to other COVID-19 patients (57.07 ± 16.57 years; P = 0.0001).
Of the 420 patients, the mortality rate was 11.7% (49 patients). The mean age of deceased patients was 68.73 ± 14.04. There was a significant association between the age of patients and mortality (P = 0.0001). The mean age of the living patients was 56.85 ± 16.76 years. Of the 49 deceased patients, 8 (16.3%) had cerebrovascular events (P = 0.049).
5. Discussion
Neurologic symptoms of COVID-19 have been reported since the outbreak of the pandemic (3). Nonspecific neurologic symptoms (such as headache, dizziness, and seizure) can be associated with this disease (6, 13). This study suggested that 67% of patients with COVID-19 had at least one of the neurological symptoms. Previous studies reported the prevalence of the neurologic manifestations of COVID-19 within the range of 36.4% - 57.4% (3, 14). Liotta et al. reported that 62.7% of hospitalized patients with COVID-19 suffered from neurological manifestations (15). Several studies have described the presence of COVID-19 particles in the cytoplasm of frontal lobe neurons, brain endothelial cells, and CSF in COVID-19 patients (16, 17). In addition, the breakdown of the blood-brain barrier and the presence of inflammatory cytokines can play an important role in the involvement of CNS and cause neurological symptoms (16, 18). In this study, the most common background comorbidities were hypertension, diabetes mellitus, and heart disease, similar to previous studies (14, 19). CVD was observed in 8.3% of COVID-19 patients. There was a significant association between CVD and background comorbidities. Researchers have shown that the association of stroke with COVID-19 may result from hyper coagulopathy and endothelial damage and, consequently, the release of inflammatory cytokines (20, 21). However, we found higher rates of CVD compared to previous studies (14, 22, 23). Headache and myalgia were the most common nonspecific neurological symptoms of COVID-19. Previous studies have shown that 44% to 70% of hospitalized patients have myalgia (24, 25). Myalgia is caused by widespread inflammation and cytokine response, which is a common symptom in patients with viral infections (26). Our research has demonstrated 2 cases of Guillain-Barre syndrome (GBS) and myelitis. Therefore, a dysimmune or parainfectious response provoked by COVID-19 infection should be considered.
The limitation of this study is a lack of information on the severity of COVID-19 and its relationship with neurological symptoms. The data obtained were retrospective; thus, some important information may have been lost.
5.1. Conclusions
Neurologic symptoms are common in admitted patients with COVID-19. They are various and appear from mild symptoms (such as symptoms of sensory insights) to life-threatening CNS disorders. The neurologic symptoms due to COVID-19 infection may be related either to direct impairment of neurologic tissues or indirectly to inflammatory cytokine release. As a result of coagulation disorder in patients with COVID-19, some conditions (such as stroke) can be seen, even during recovery.