1. Background
Acinetobacter baumannii (A. baumannii) is a glucose non-fermentative, Gram-negative aerobic, non-motile coccobacillus, ubiquitous in nature, and persistent in hospital environment (1, 2). A. baumannii is also a nosocomial pathogen and accounts for almost 10% of hospital-acquired infections by 80% of all reported Acinetobacter infections, including bacteremia, ventilator-associated pneumonia, meningitis, wound, skin, soft-tissue infections, peritonitis, bloodstream, and urinary tract infections (2-8). In the past decade, A. baumannii strains resistant to all known antibiotics have now been emerged as a significant clinical problem worldwide (9-11). Ability of A. baumannii to persist and to survive for long periods of time on surfaces has made it as a frequentative cause of health-care associated infections. This bacteria can survive over long periods under dry conditions (7, 12). A. baumannii encodes multiple virulence factors; of them biofilm-forming ability is considered one of the key virulence attributes of this pathogen (5, 7).
A. baumannii biofilm associated protein (bap) is a cell surface protein and virulence factor. Bap protein in A. bumanii is a large protein (854-kDa) and homologous to staphylococcal protein and has been characterized in other bacteria genera typically in those are associated with nosocomial infection, such as Enterococcus spp. and Pseudomonas spp. The bap is significant for the formation of maturation biofilm on biotic and abiotic surfaces (4, 7). Quantitative comparison of biofilms formed by a wild-type and the bap-deficient mutant bacteria has been demonstrated that the mutant was unable to develop biofilm thickness, it has been shown that the bap gene is required for biofilm formation (13). A porin protein of A. baumannii, the 38-kDa outer membrane protein A (OmpA), plays an important role in the biofilm formation (3, 5, 7). The CsuA/BABCDE gene is required for formation of pili involved in adherence to abiotic surfaces. It has been demonstrated that inactivation of the csuE gene, as a part of the CsuA/BABCDE chaperone-usher complex, eliminates pili production and biofilm formation (14, 15). In A. baumannii autoinducer synthase (AbaI), part of the quorum sensing (QS) system is responsible for Acyl-homoserine lactones (AHL) production. The AHL is a major component of auto-inducer signals, which are used by gram negative bacteria for biofilm formation (5, 16).
Biofilm-forming ability in A. baumannii plays an important role in the pathogenesis and subsequently antibiotic resistance (17). Therefore, the purpose of the current study was to evaluate the biofilm formation status of A. baumannii isolated from wound, Lumbar Puncture, bloodstream, and urinary tract infections, and we also aimed to investigate the bap, ompA, csuE, and abaI genes involving in nosocomial infections pathogenesis in A. baumannii isolated from hospital environments and patients in Tehran, Iran.
2. Methods
2.1. Bacteria Isolates
The current descriptive study was performed on 120 non-duplicate isolates of A. baumannii who were isolated from UTI, bloodstream, catheter, wound, and sputum of hospitalized patients and as well as hospital environments from April to December 2014 in Imam Hossein teaching hospital in Tehran, Iran. Isolates were confirmed by conventional microbiological and biochemical tests such as oxidase test (Merck, Germany), motility, and growth at 44°C in the microbiology laboratory and then were confirmed by amplification of bla-oxa-51-like gene using PCR. Then the isolates were stored at -70°C for further investigated.
2.2. Biofilm Formation Analysis
2.2.1. Modified Congo Red Agar Tset (MCRA)
Phenotypic formation of biofilm in A. baumannii isolates was determine by culture on MCRA plates as formerly cleared by Arciola et al. (18). Briefly, Congo Red Agar (CRA) plates were collected with combining 36 gram of saccharose (Sigma, USA) and 0.8 gram of Congo red powder (Merck, Germany) to 1 liter of brain heart infusion (BHI) Agar (Merck, Germany). The plates were incubated at 37°C for 24 hours and subsequently at room temperature (20 - 25°C) for overnight. The colonies morphology was then explained based on colony color as red, almost black, black, and very black. Red colonies were considered unable to produce biofilm and almost black colors were classified as strains of a weak formation biofilm activity. Conversely, strains with black and very black colonies were indicative as intense biofilm producer strains.
2.2.2. Microtiter Plate Method
Biofilm formation was defined quantitatively using a modified microtiter plate assay as biofilm formation was measured quantitatively using a modified microtiter plate assay as described before (19). In summary, isolates were grown in Tripticase-Soy Broth (TSB, Merck, Germany) containing 0.5% glucose (Merck, Germany) and were incubated overnight at 37°C. Cultures were diluted 1:40 in TSB containing 0.5% glucose, afterwards from diluted solution, 200 μL was added to wells of a polystyrene plate and was incubated at 37°C for 48 hours. The wells that contained 200 μL of TSB containing 0.5% glucose were negative control. Wells were slowly washed three times with Phosphate Buffered Saline (PBS; pH 7.2; Invitrogen, USA), were fixed by methyl alcohol (Merck, Germany) for 20 minutes, were dried at 20 - 25°C (room temperature), and then were strained by 0.1% safranin (Merck, Germany). The safranin dye linked to the adherent cells was dissolved with 150 μL of 95% ethyl alohol (Merck, Germany) per well. Eventually, the optical density (OD) of each well was measured by using the ELISA reader (BioTek, USA) at 490 nm (A490). Optical density cut-off (ODc) was defined as 3 × standard deviation (SD) above mean OD of negative control. Biofilm formation with strains was analyzed and classified based on the absorbance of the safranin-stained attached cells (Table 1).
| Cut-Off Value Calculation | Mean of OD Values Results | Biofilm Formation Abilities |
|---|---|---|
| OD ≤ 0.059 | OD ≤ 0.059 | None |
| ODc< OD ≤ 2 × ODc | 0.059 < OD ≤ 0.118 | Weak |
| 2 × ODc < OD ≤ 4 × ODc | 0.118 < OD ≤ 0.236 | Moderate |
| OD > 4 × ODc | OD > 0.236 | Strong |
Assortment of Biofilm Formation Abilities with Microtiter Plate Assay
2.2.3. Gene Pattern Identification
DNA- Genomic was extracted from pure cultures using the high pure PCR Template Preparation Kit (Roche, Germany), according to the manufacturers instruction. The extracted DNA was used for polymerase chain reaction (PCR) test. In our study, A. baumannii isolates were screened for the presence of the bap, abaI, csuE, ompA, and blaPER-1genes using PCR. Sequences of the primers are defined in Table 2. PCR was managed on 25 μL of final volume using HotStarTaq Master Mix kit (SinaClon, Iran) containing 12.5 μL of 2x HotStarTaq Master Mix (containing 0.4 mM of each dNTP, 3 mM MgCl2, and 0.08 U/μLTaq DNA polymerase in reaction buffer) with 1 μL of each primer (20 pmol), 1 μL of the DNA template, and 9.5 μL of ddH2O. DNA amplification was accomplished in a thermocycler (Eppendorf, Germany) with a primary denaturation step at 94°C for 4 minutes, 30 amplification cycles for the bap, csuE, and ompA genes and 35 amplification cycles for the abaI gene, each with 45 seconds at 94°C, 45 seconds at various annealing temperatures for several genes (Table 2), and at 72°C for 45 seconds, followed with an extra extension step at 72°C for 5 minutes. The amplified products were electrophoresed on 1.5% agarose gel (Sigma, USA) and were visualized by ethidium bromide staining (Sigma, USA). Genes were sent for sequencing (Bioneer, Korea). A. baumannii ATCC 19606 was used as the producer of biofilm control strain due to the fact that it has been all genes of biofilm formation.
| Primre | Sequence (5′ - 3′) | Products Sizes, bp | Annealing, °C | Ref. |
|---|---|---|---|---|
| bap | Fw- ATAACTCGGCTGTTTACGG | 358 | 49 | This study |
| Rv- ACTGATGGTGTTGGAAGTG | ||||
| ompA | Fw- CTGGTGTTGGTGCTTTCTGG | 352 | 49 | This study |
| Rv- GTGTGACCTTCGATACGTGC | ||||
| abaI | Fw- CGCTACAGGGTATTTGTTGA | 370 | 46 | This study |
| Rv- TCGTAATGAGTTGTTTTGCG | ||||
| csuE | Fw- AGACATGAGTAGCTTTACG | 516 | 52 | (17) |
| Rv- CTTCCCCATCGGTCATTC | ||||
| blaPER-1 | Fw- GCAACTGCTGCAATACTCGG | 340 | 55 | (20) |
| Rw- ATGTGCGACCACAGTACCAG |
Primers Were Used in This Study
2.3. Statistical Analysis
The relationship between biofilm formation and the existence of biofilm related genes among A. baumannii isolates was appraisement by the Pearson Chi-Square test using SPSS version 21 (SPSS, Chicago, IL, USA) P values less than 0.05 were considered to be statically significant.
3. Results
Totally, 120 A. baumannii isolates, 98 clinical, and 22 environmental were evaluated for biofilm formation using Microtiter plate, Congo red agar methods, and the existence of genes related to biofilm by standard PCR. In this study, 13 (10.8%) isolates of A. baumannii showed biofilm formation, where 7 and 6 isolates were clinical and environmental, respectively. Biofilm formation was significantly more frequent in environmental (6 out of 22) samples than clinical (7 out of 98) ones (P = 0.014).
The GenBank provided accession number for bap (accession number KU1751177), ompA (accession number KU523791), csuE (accession number KY049981), abaI (accession number KU648404), and blaPER-1(accession number KU672727).
In term of the severity of biofilm formation, 9 isolates (7.5%) showed black/very black colonies considered as strong biofilm producers, while 4 isolates (3.3%) showed almost black colonies indicating weak biofilm producers (Table 3). In the MCRA method, relationship between the severity of biofilm formation in clinical and environmental isolates is considered to be not statistically significant (P values more than 0.05).
| Method/Biofilm Formation | Clinical Isolates (n = 98) | Environmental Isolates (n = 22) | Total (n = 120) |
|---|---|---|---|
| Modified Congo red agar | |||
| Very black | 4 (4.1) | 2 (9.1) | 6 (5) |
| Black | 3 (3.1) | 0 (0) | 3 (2.5) |
| Almost black | 0 (0) | 4 (18.2) | 4 (3.3) |
| Red | 91 (92.8) | 18 (81.8) | 107 (89.2) |
| Microtiter plate assay | |||
| Strong | 3 (3.1) | 2 (9.1) | 5 (4.15) |
| Moderate | 3 (3.1) | 0 (0) | 3 (2.5) |
| Weak | 1 (1) | 4 (18.2) | 5 (4.15) |
| None | 91 (92.8) | 18 (81.8) | 107 (89.2) |
Formation Biofilm of A. baumannii Isolates in Congo Red Agar Method and Microtiter Plate Assaya
Moreover, in the Microtiter plate method, 5 isolates (4.2%) of the strains were strong biofilm producers, 3 clinical isolates, and 2 environmental isolates; in addition, 3 isolates (2.5%) were moderate biofilm producers that were all clinical, and 5 isolates (4.2%) were found to be weakly adherent, where 4 isolates were environmental. The relationship between severity of biofilm formation in clinical and environmental isolates by both methods were considered to be not statistically significant (P values more than 0.05).
Whereas among the clinical strains of A. baumannii, by culturing them on Modified Congo red agar (MCRA) and Microtiter plate method were 7.2% and 6.2% of the strains were found to be strong, respectively (Table 3).
Considering the environmental A. baumannii isolates in both methods, 18.2% of were strong and weak biofilm producers, respectively. Overall, by both methods, 89.2% of studied A. baumannii isolates were non-biofilm producers while 10.8% were biofilm producers. There were no differences in sensitivity or specificity by both methods. The biofilm formation abilities of clinical strains were found to be slightly less than those of environmental strains.
3.1. Biofilm Related Genes
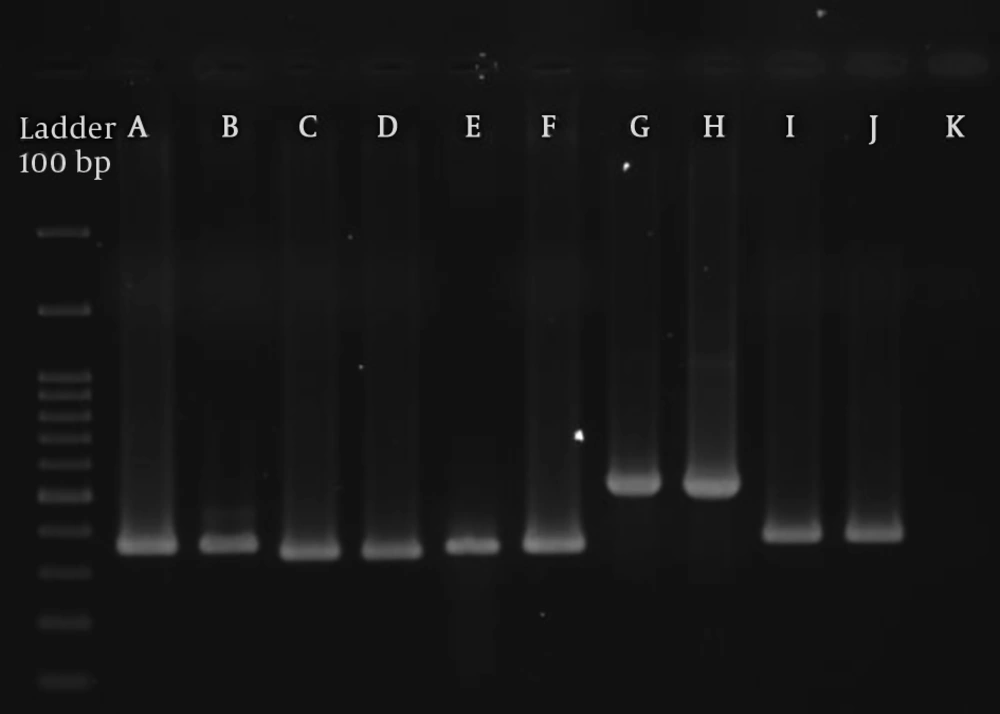
All isolates were investigated for the bap, abaI, csuE, ompA, and blaPER-1genes. The abaI, csuE, and ompA genes were present in all (100%) A. baumannii isolates. The bap and blaPER-1genes were found in 17 (14.2%) and 16 (13.3%) isolates, respectively. Distribution of the bap gene in clinical and environmental isolates was 8.4% and 31.8%, respectively and all of the blaPER-1genes were clinical samples. Between biofilm formation and the bap gene have not relationship of the A. baumannii samples by biofilm phenotype were positive for the existence of the bap genes while 7 of the isolates was not showed the bap gene. Relationship between the bap and blaPER-1genes in clinical and environmental isolates was statistically significant (P values less than 0.05). The bap gene in environmental strains was found to be higher than those of clinical strains. The PCR product of the bap, abaI, ompA, and csuE genes from A. baumannii isolates is shown in Figure 1.
PCR-product of the bap, abaI, csuE, ompA, and blaPER-1genes from A. baumannii isolates. A: positive control of bap gene; B: bap gene (358bp); C: positive control of blaPER-1gene; D: blaPER-1gene (340 bp); E: positive control of ompA gene; F: ompA gene (352 bp); G: positive control of csuE gene; H: csuE gene (516 bp); I: positive control of abaI gene; J: abaI gene (370 bp); K: negative control.
4. Discussion
The purpose of the current study was to evaluate the biofilm formation by A. baumannii obtained from wound, Lumbar Puncture, bloodstream, and urinary tract infections, and the investigation of the bap, abaI, csuE, ompA, and blaPER-1genes involving in nosocomial infection pathogenesis in A. baumannii isolated from environment and patients in Imam Hossein hospital in Tehran, Iran.
In this study we evaluated the biofilm formation and its severity status with Congo Red Agar (MCRA) and Microtiter plate method. MCRA technique was easy to perform and of course due to less washing steps, its result was more reliable. Several washing steps in Microtiter plate method may result in distrust. This difference may be due to several factors such as multiple washing steps in Microtiter plate method.
Our results with MCR agar and Microtiter plate methods showed that the biofilm formation rate was low (10.8%) and biofilm formation was significantly more frequent in environmental (6 out of 22) samples than clinical (7 out of 98) ones (P = 0.014). Kumari et al. (10) and Cevahir et al. (1) studies showed that biofilm formation was abundant in their studied samples.
Formation biofilm ability and adhesiveness in A. baumannii play a key role in the host pathogen interplay and in infections related with medical devices, involving a range of bacterial conditions, multiple environmental cues, and cell signals. Recently, adequately attention has been directed toward the correlation among the genetic factors involved in cohesion to eukaryotic cells and those signified in the initial step of biofilm production on abiotic surfaces (5). According to the condition of biofilm formation, many of the gene products have already been demonstrated to play key roles in the adhesiveness and biofilm production of A. baumannii on both biotic and abiotic surfaces. The biofilm-associated protein (bap), expressed on the cell surface of bacteria, first reported by Loehfelm and et al. (2008) in A. baumannii have a role in intercellular adhesion, thus, most probably biofilm maturity on distinct substrata (4, 5, 13). Other proteins seem to play an important role in biofilm formation on surfaces, of these, the outer membrane protein; ompA, the 38 kDa porin protein with pore size 1.3 nm, plays a major role in the attachment phase of an A. baumannii on abiotic surfaces, and also in the pathogen interaction (3, 5, 21).
Early studies on the A. baumannii ATCC 19606 T strain reported that pili formation is intermediated by the csuE, which is required for the first stages of bacterial adhesion on abiotic surfaces, resulting in biofilm formation and development (5). The A. baumannii M2 strain was demonstrated to produce an N-acyl-homoserine lactone (abaI), which as a Quorum Sensing molecule is significant for the production of biofilm on abiotic surfaces (5). The blaPER-1is an extended-spectrum-lactamase, which was found in Acinetobacter spp. and P. aeruginosa biofilm formation was markedly reduced. In this bacterium, biofilm formation is enhanced by the presence and expression of the blaPER-1gene. Other studies have been demonstrated that clinical isolates of MDR A. baumannii had a high ability to produce biofilm and adherence to respiratory epithelial cells (9, 22-24).
Our results showed that the csuE gene was 100% in all clinical and environmental isolates, which has also been shown in the previous studies (25, 26). The most probable explanation for existence of the csuE gene in all isolates is that all the isolates had pili. In this study 120 (100%) isolates have the ompA gene and abaI gene. We did not find a study based on quantitative assessment of clinical and environmental isolates related to the ompA gene and abaI gene. In this study 17 (14.2%) isolates were positive for the bap gene, of them 10 (8.4%) clinical isolates and 7 (31.8%) belonged to the environmental isolates. Relationship between biofilm formation and the bap gene was not statically significant. Our findings do not support the study of Goh et al. (4), in which they showed that the bap gene were very frequent in the studied isolates. One possible explanation for this discrepancy is that they studied on a smaller number of A. baumannii, all from clinical sources with resistant to carbapenem. The frequency of the blaPER-1gene varies based on different studies; i.e. Yong and et al. detected the blaPER-1genein 54.6% Acinetobacters in Korea, often in the patient sputum of intensive care unit (ICU) (27). Lee et al. showed the blaPER-1in all multidrug-resistant (MDR) clinical isolates of A. baumannii (28).
We found 13.3% studied isolates were positive for the blaPER-1gene. According to the results of the study, biofilm formation in environmental A. baumannii isolates was more than clinical isolates. One possible explanation for the betterment in the environmental isolates might be attributed to the increased gene exchanges between environmental A. baumannii isolates. Importantly our study revealed that the MCRA technique is significantly better than the Microtiter plate method for evaluation phenotypic biofilm formation.
Overall, the abaI, csuE, and ompA genes were detected in all isolates regardless the biofilm status, while the bap and blaPER-1genes was found in some of the A. baumannii isolates from patients and environmental; therefore, in the studied isolates, no relationship between biofilm formation and the presence of interested genes was found. For better understanding of the relationship among biofilms status and related genes in A. baumannii pathogenesis, further studies considering all other virulence markers genes in both genomic and proteomic level are recommended.
4.1. Conclusions
The Congo red agar method was better than the Microtiter plate technique for phenotypic evaluation of biofilm formation in the A.baumannii. According to the current study, the abaI, csuE, and ompA genes were detected in all isolates while the bap and blaPER-1genes was more frequent in clinical samples. No correlation was found among biofilm production severity and genes status. More studies are recommended for detection of biofilm related genes role on the host - pathogen interaction.