1. Background
SARS-CoV-2 was first identified in Wuhan, China in Dec 2019. Chest CT was more useful than RT-PCR in COVID-19 diagnosis during the epidemic. CT scans can predict disease progression and detect its consequences (1, 2). Bullous and cystic diseases of the lung in COVID-19 patients have been declared in some case reports (3). No large-scale study has examined the clinical characteristics of COVID-19 patients with pulmonary bullae and cystic diseases or their impact on survival. This study reviewed chest CT scans of COVID-19 patients to investigate the clinical characteristics of pulmonary bullae and cystic diseases and see whether these diseases are associated with survival.
2. Methods
2.1. Study Design and Participants
This cross-sectional study obtained ethical approval from the Ethics Committee of Tehran University of Medical Sciences. All participants remained anonymous.
We enrolled Thirty-four severe COVID-19 patients hospitalized in Imam Khomeini and Sina hospitals from July 2021 to February 2022. An experienced radiologist (S. M.) reviewed the chest CT scans of all patients for pulmonary bullae or cysts. Patients with COVID-19 and bullous disease of the lung were included, and the relevant data were extracted from the hospital information system. Moreover, the size, side, and number of bullae were recorded. This research was approved by the Ethics Committee of Tehran University of Medical Sciences. The patients were followed for 30 days for survival analysis. Age, sex, underlying comorbidities and mode of breathing by individual patients were recorded.
2.2. Chest CT Protocols and Interpretation
All CT scans were obtained with one kind of CT system. All patients underwent unenhanced CT with a 16-slice CT scanner (CT emotion 16, Siemens Healthcare, Erlangen, Germany). Given the probability of COVID-19, all necessary protective measures have been taken according to the Iranian Ministry of Health guidelines (4).
A radiologists with Iranian Board Certification, who was blinded to RT-PCR result and COVID-19-related symptoms, reported all CT scans by consensus. She described main CT scan features (ground-glass opacity (GGO) + pulmonary bullae).
2.3. Statistical Analyses
SPSS version 26 (SPSS Inc, Chicago, Ill, USA) was used to analyze the data. The Kolmogorov–Smirnov test was used to assess the normality of continuous data. Normally and non-normally distributed data, and categorical variables are presented as the means (SD) and the medians (IQR), and numbers (%), respectively. The survival data were used to generate Kaplan-Meier curves, and survival was compared by the log-rank test. Statistical significance was considered at a P value < .05 (two-tailed).
3. Results
3.1. Demographic and Clinical Characteristics
Thirty-four patients with COVID-19 and lung bullae were identified and included in this study. Included patients averagely aged 53.05 (16.80) years, and 11 (32.4%) were ≥ 70 years old (Table 1). Eighteen patients (52.9%) were male. The frequency of smoking was 32.4% in our population.
| Variables | Values |
|---|---|
| Age, mean ± SD | 53.05 ± 16.80 |
| ≥70 (%) | 11 (32.4) |
| Sex (male), No. (%) | 18 (52.9) |
| Smoking, No. (%) | 11 (32.4) |
| Comorbidities, No. (%) | |
| HTN | 13 (38.2) |
| DM | 15 (44.1) |
| CKD | 5 (14.7) |
| Respiratory comorbidities, No. (%) | |
| Asthma | 2 (5.9) |
| COPD | 5 (14.7) |
| Pneumothorax | 3 (8.8) |
| Mode of breathing, No. (%) | |
| Spontaneous | 21 (61.8) |
| CPAP/NIV | 6 (17.6) |
| Intubation | 7 (20.6) |
| Side of bullae, No. (%) | |
| Left | 14 (41.2) |
| Right | 13 (38.2) |
| Bilateral | 7 (20.6) |
| Size of bullae, No. (%) | |
| Small a | 17 (50) |
| Medium b | 10 (29.4) |
| Large c | 7 (20.6) |
| Number of bullae, No. (%) | |
| Single | 20 (58.8) |
| Multiple | 14 (41.2) |
Abbreviations: DM, diabetes mellitus; HTN, hypertension; CPAP, continuous positive airway pressure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; NIV, noninvasive ventilation.
a < 5 cm.
b 5 - 10 cm.
c > 10 cm.
Regarding systemic comorbidities, 38.2% had hypertension (HTN), 44.1% had diabetes mellitus (DM), and 14.7% had chronic kidney disease (CKD). Regarding respiratory comorbidities, 5.9% had asthma, 14.7% had chronic obstructive pulmonary disease (COPD), and 8.8% had a pneumothorax.
The breathing of 61.8% of patients was spontaneous, 17.6% were on noninvasive ventilation (NIV)/continuous positive airway pressure (CPAP), and 20.6% were intubated.
All included patients had bullae in their lungs. Of these, 41.2% were located in the left lung, 38.2% were in the right lung, and 20.6% were bilateral. Most bullae were small (50%) and medium (29.4%). Finally, the majority of patients had a single bulla (58.8%).
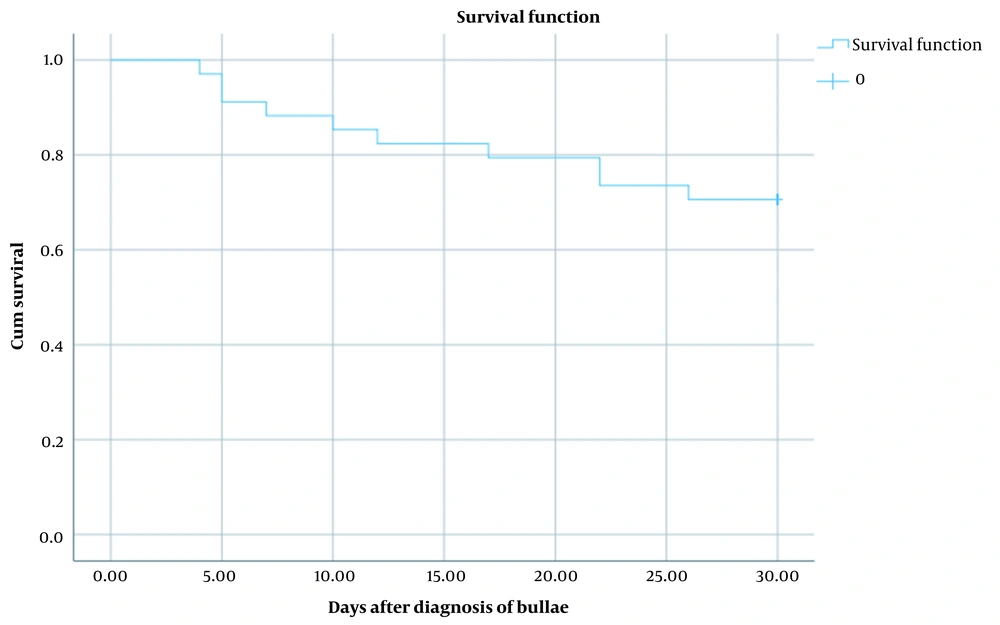
3.2. Survival Analysis
We followed the patients for 30 days after diagnosis of bullae. The mortality rate was 29.4% (10 patients) in this period. The average survival time for deceased patients was 13 (8.17) days. Figure 1 shows the survival plot of the patients (mean, 95% CI: 22.03 - 27.96).
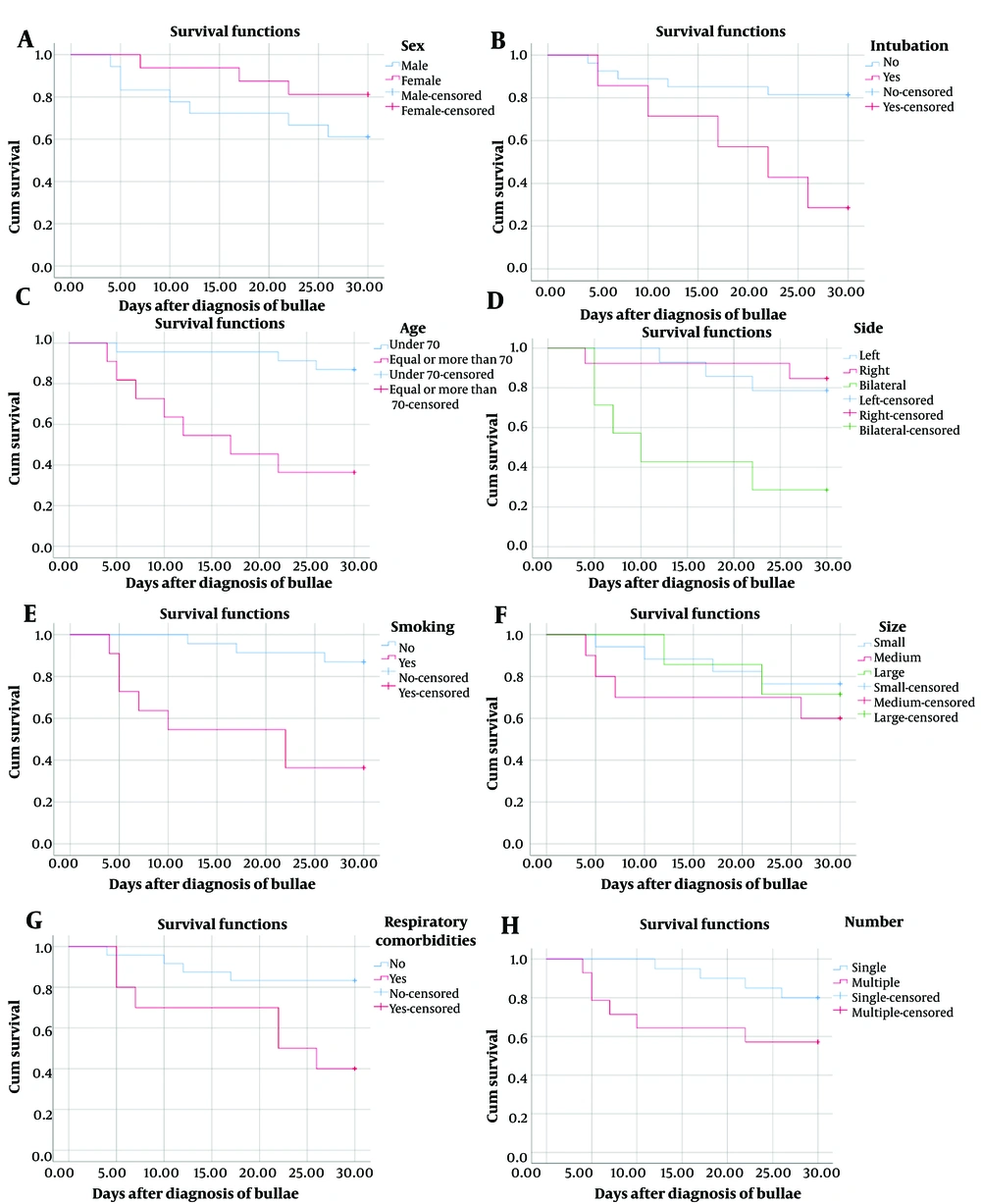
3.3. Associated Factors of Survival Time
In this section, we investigated the factors influencing the survival time in cases with bullae and COVID-19. For this purpose, we assessed the possible effects of sex, age, smoking, respiratory comorbidities, intubation, and the side, size, and number of bullae on the survival of patients. Our results demonstrated that increased age (P = 0.001), smoking (P = 0.001), respiratory comorbidities (P = 0.013), intubation (P = 0.008), and bilateral bullae (P = 0.005) are associated
with lower survival time in patients with COVID-19 and bullae (Figure 2 and Table 2). No significant association was found between survival time and sex, as well as the size and number of bullae.
| Variables | Mean | 95% CI | Log Rank P-Value |
|---|---|---|---|
| Sex | 0.188 | ||
| Male | 23.00 | 18.31 - 27.68 | |
| Female | 27.25 | 24.14 - 30.35 | |
| Age | 0.001 | ||
| < 70 | 28.39 | 26.22 - 30.55 | |
| ≥ 70 | 17.90 | 11.79 - 24.02 | |
| Smoking | 0.001 | ||
| No | 28.47 | 26.65 - 30.29 | |
| Yes | 17.72 | 11.23 - 24.21 | |
| Respiratory comorbidities | 0.013 | ||
| No | 26.79 | 23.82 - 29.76 | |
| Yes | 20.70 | 14.32 - 27.07 | |
| Intubation | 0.008 | ||
| No | 26.29 | 23.17 - 29.41 | |
| Yes | 20.00 | 13.29 - 26.70 | |
| Side | 0.005 | ||
| Left | 27.21 | 24.25 - 30.17 | |
| Right | 27.69 | 23.93 - 31.45 | |
| Bilateral | 15.57 | 7.72 - 23.42 | |
| Size | 0.597 | ||
| Small | 26.11 | 22.46 - 29.76 | |
| Medium | 22.20 | 15.30 - 29.09 | |
| Large | 26.28 | 21.50 - 31.06 | |
| Number | 0.095 | ||
| Single | 27.85 | 25.70 - 29.99 | |
| Multiple | 20.92 | 15.04 - 26.81 |
4. Discussion
This study is the first to provide large-scale evidence of COVID-19 coexisting with pulmonary bullous disease. We found 34 COVID-19 patients with lung bullae, mostly located in the left or right lung. Factors such as age, smoking, respiratory comorbidities, intubation, and bilateral bullae were associated with lower survival time. However, there was no significant association between survival time and sex, size, or number of bullae. These findings are important and add to the growing literature on COVID-19 radiological manifestations, which can cause permanent airflow obstruction and emphysema not typically observed in other viral infections.
Male patients aged 30 - 55 with no prior pulmonary history or mechanical ventilation have developed bullae after COVID-19. Bullous lung changes can occur as early as 14 days after infection, with severity ranging from mild-to-moderate COVID-19 (5, 6).
Radiological abnormalities can persist for more than 3 months after initial SARS-CoV-2 infection in up to 50% of survivors, which is consistent with previous coronavirus infections like SARS and Middle East respiratory syndrome (7, 8).
Some findings emerge later in the infection. In acute infection, CT manifestations vary depending on clinical progression. GGO and consolidations can progress to mild reticular abnormalities in some patients by week 2, while consolidations can worsen until week 3 (9).
Diagnosing pneumatic cysts is challenging. Differentiating cysts from cavities is crucial due to their varying causes and symptoms. Cysts are more common in subpleural areas and usually suggest bullae, emphysema, or honeycombing (10, 11). The incidence of cystic disease associated with COVID-19 is uncommon, ranging from 9% to 25% (12). If the patient does not have pre-existing emphysema or interstitial disease, the existence of cysts can increase the specificity of the COVID-19 diagnosis because these findings have not been reported in other viral pneumonia (13). This study is limited regarding the causality relationship between COVID-19 and pulmonary bullous disease. The mechanism of bleb and bullae formation is unclear, but studies indicate late-stage ARDS in mechanically ventilated patients is associated with more bullous lesions and structural changes. Late-stage ARDS presents as a restrictive lung disease with emphysema-like lesions. Structural changes over time may lead to air-filled cavities kept open by a one-way valve, resulting in large lung bullae (14). A case report detected a lung bulla on CT after a pneumothorax despite no initial bullae before COVID-19 treatment, suggesting COVID-19 pneumonia caused lung injury. The report suggests corticosteroid therapy at the start of hospitalization may be associated with bulla development (15). The recorded respiratory comorbidities in our study were asthma, COPD, and pneumothorax, and we did not present any information on whether these pulmonary bullous diseases occurred before or after COVID-19 infection. As a result, this coexistence might be coincidental.
Pulmonary bullae can be secondary to fibrosis, parenchymal damage, or low compliance with mechanical ventilation. It can also occur spontaneously in the late and intermediate stages of ARDS. Some believe it's linked to the consolidation resorption process (6, 16, 17). A CT scan with the expiratory phase should be conducted when the patient has risk factors linked to post-acute COVID-19 or cystic lesions.
4.1. Conclusions
The first large-scale cross-sectional study to report the coexistence of COVID-19 and pulmonary bullous disease. Although our results do not establish a causal relationship between the two, clinicians should be aware of this complication in COVID-19 patients. Findings also suggest that bilateral bullae are associated with lower survival time. Further studies are needed to determine the incidence and causality relationship between COVID-19 and lung bullae.