1. Context
Fungal infections (FIs) represent a significant complication following liver transplantation (1). Despite numerous advances in drug and device development, the risk of FI remains a grave concern for patient outcomes. Furthermore, delayed diagnosis of fungal infections significantly elevates the risk of morbidity and mortality in liver transplant recipients (2). Challenges associated with exposure to fungal pathogens encompass nonspecific clinical presentations, the emergence of resistant species, and variations in preventive therapies. Additionally, advanced age and non-hepatic comorbidities are the most prominent risk factors for fungal infections in candidates undergoing liver transplantation. Among the major organs affected by FIs in liver transplant recipients is the CNS, with several fungal species, including Cryptococcal and Candida, implicated (3).
2. Evidence Acquisition
The challenges posed by CNS fungal infections include delayed diagnosis, limited CNS penetration of many antifungal drugs, and the rising threat of antifungal resistance. This article provides a comprehensive review of the incidence and prevalence of CNS fungal infections in LTs, along with associated risk factors and the complexities involved in devising effective diagnostic and treatment strategies.
3. Results
3.1. Common Fungal Infections in the CNS
Fungal infections affecting the CNS are associated with significant morbidity and mortality due to the limited penetration of many antifungal medications into the CNS and the increasing prevalence of antifungal resistance (4). Studies indicate that the overall incidence of CNS fungal infections following liver transplantation ranges from approximately 1 to 4% (5, 6). Several studies have identified major fungal species implicated in CNS fungal infections, including Candida spp., Cryptococcus spp., Aspergillus spp., Blastomyces dermatitidis, Histoplasma capsulatum, Coccidioides spp., and Zygomycete (7, 8). Depending on the specific fungal species involved, CNS fungal infections can lead to various disorders, such as brain abscesses, acute and chronic meningitis, rhinocerebral disease, and involvement of the skull base and spinal cord (9).
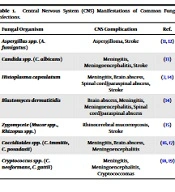
Table 1 presents the most common clinical fungal species associated with CNS infections and their clinical manifestations. It is worth noting that advancements in surgical techniques and post-operative care have led to a recent decrease in the incidence of CNS fungal infections following liver transplants (10).
| Fungal Organism | CNS Complication | Ref. |
|---|---|---|
| Aspergillus spp. (A. fumigatus) | Aspergilloma, Stroke | (11, 12) |
| Candida spp. (C. albicans) | Meningitis, Meningoencephalitis, Stroke | (13) |
| Histoplasma capsulatum | Meningitis, Brain abscess, Spinal cord/paraspinal abscess, Stroke | (7, 14) |
| Blastomyces dermatitidis | Brain abscess, Meningitis, Meningoencephalitis, Spinal cord/paraspinal abscess | (14) |
| Zygomycete (Mucor spp., Rhizopus spp.) | Rhinocerebral mucormycosis, Stroke | (15) |
| Coccidioides spp. (C. immitis, C. posadasii) | Meningitis, Brain abscess, Meningoencephalitis | (16, 17) |
| Cryptococcus spp. (C. neoformans, C. gattii) | Meningitis, Meningoencephalitis, Cryptococcomas | (18, 19) |
Central Nervous System (CNS) Manifestations of Common Fungal Infections.
3.1.1. Aspergillus Species
The risk of Aspergillus infection in patients undergoing liver transplantation ranges from 1% to 9% (20, 21). According to findings from the Swiss Transplant Cohort Study, Aspergillosis (A. fumigatus, Aspergillus spp.) accounted for 8/11 (approximately 72%) of all fungal infections in the CNS (22). Several risk factors influence the incidence of Aspergillus infection, including diabetes, prolonged surgical duration, re-transplantation, acute kidney injury, cytomegalovirus (CMV) infection, and antibiotic resistance. Aspergillus species are ubiquitous in the environment, and pulmonary infection can result from the inhalation of airborne fungal conidia, depending on various factors (23). Among over 200 Aspergillus species, the most common infecting species in liver transplant recipients are Aspergillus fumigatus (73%), Aspergillus flavus (14%), and Aspergillus terreus (8%). Pulmonary infection is the predominant form of Aspergillus infection in liver transplant recipients, often occurring through inhalation (22, 23). However, Aspergillus infection can also involve the central CNS. The clinical presentations of CNS Aspergillus infection vary depending on the course of the infection and can include brain abscesses, meningitis, cranial sinus thrombosis, cerebritis, and ventriculitis (24). Consequently, patients may exhibit a range of symptoms such as fever, headaches, dizziness, lethargy, altered mental status, abnormal gait, and seizures (25). For example, CNS infection with Aspergillus fumigatus can lead to aspergilloma formation and CNS strokes (23). Diagnosing cerebral aspergillosis is challenging due to its poor prognosis (26). Brain imaging, including computed tomography (CT) and contrast-enhanced magnetic resonance imaging (MRI) of the brain, is essential for patients suspected of CNS involvement (27, 28). Triazole therapy is the standard treatment for Aspergillus infections, which has been shown to reduce overall mortality (20). However, it is important to note that all available antifungal drugs carry the risk of hepatotoxicity, which is further increased when used concurrently with immunosuppressive therapy. Studies indicate that despite the morbidity associated with Aspergillus infection in liver transplant recipients, the use of triazole therapy, specifically voriconazole, has improved outcomes (20). Additionally, when feasible, surgical resection of cerebral lesions, such as those affecting the paranasal sinuses, bones, and brain abscesses, should be considered (25).
3.1.2. Cryptococcal Species
Cryptococcosis, a common fungal infection in solid organ transplant recipients, often leads to CNS disease (29). According to the Infectious Diseases Community of Practice of Transplantation guidelines of the American Society, cryptococcosis is the third most frequent invasive fungal infection in liver transplant recipients (29). The Swiss Transplant Cohort Study reported that Cryptococcosis (C. neoformans) accounted for 3/11 (approximately 27%) of all fungal infections in the CNS (22). Cryptococcal infections significantly contribute to patient morbidity and mortality (29, 30). Cryptococcus can infect the lungs without causing symptoms when basidiospores and encapsulated yeast cells are inhaled from the environment. Cryptococcal infection can then spread to the CNS through direct invasion from the lungs (30, 31). The risk of Cryptococcal disease is particularly high in both pre- and post-transplant patients with end-stage liver disease (ESLD) due to the physiological abnormalities associated with ESLD, including hypogammaglobulinemia, complement deficiency, phagocyte dysfunction, and impaired cell-mediated immunity (32, 33). Furthermore, the use of immunosuppressive drugs after liver transplantation increases the risk of Cryptococcal infections in patients with compromised cell-mediated immunity (34). Cryptococcus species, which are ubiquitous fungi, can be found in soil and bird droppings. Among the various species, Cryptococcus neoformans and Cryptococcus gattii are clinically significant and capable of causing invasive disease in humans with diverse manifestations. C. neoformans typically behaves as an opportunistic fungus in immunocompromised patients (35). In contrast, solid organ transplant recipients infected with C. gattii are more likely to develop disseminated infection and CNS disease, which can result in higher mortality rates (36). Clinical manifestations of Cryptococcus infection in the brain may include mass lesions and meningitis. Therefore, it is crucial to screen for Cryptococcal disease in liver transplant recipients presenting with symptoms such as fever, subacute mental status changes, headaches, and brain mass lesions (29). Recent studies have shown that mortality rates following Cryptococcal infection after liver transplantation are high. However, the presence of Cryptococcal infection is not an absolute contraindication for proceeding with liver transplantation (33).
3.1.3. Candida Species
Candida species, known to colonize the genitourinary tract, gastrointestinal tract, and skin, are common pathogenic organisms (6). Some studies have indicated that approximately 4 – 5% of CNS lesions are associated with Candida infections (37-39). Invasive Candida infections, which can disseminate into CNS lesions, have a high mortality rate exceeding 60%. Central venous catheter colonization is a major risk factor contributing to Candida infections in nearly 50% of transplant recipients. Manifestations of Candida CNS invasion often include cerebral microabscesses, symptomatic cerebral abscesses, meningitis with subacute symptoms (in less than 15% of cases), and vascular complications such as subarachnoid hemorrhage (38, 40). Among the pathogenic species, C. albicans is a significant contributor (6). Specific risk factors associated with C. albicans infection in liver transplant recipients include repeated laparotomy, anastomotic leak, tracheal aspirates, wound exudates, and choledochojejunostomy (41, 42). In recent years, there has been a shift from susceptible Candida species to more resistant ones, such as Candida glabrata and Candida krusei, possibly due to the widespread use of prophylactic and empirical antifungal drugs (2).
3.1.4. Other Invasive Fungi
Invasive molds like Scedosporium, Mucomycetes, and Fusarium species are relatively uncommon following liver transplantation due to the lower overall immunosuppressive burden in these patients (43). Scedosporium species are associated with approximately 25% of non-Aspergillus infections in transplant recipients, making them significant pathogens in immunocompromised individuals (44). Mucormycosis, caused by Mucomycetes, can occur in liver transplant recipients with a likelihood of 4 – 16 cases per 1000 patients (45, 46). Fusarium species rarely cause infections after liver transplants, with only six reported cases between 1979 and 2020 according to a recent review (47). Nevertheless, the incidence of infections caused by these fungal species is on the rise, primarily due to the use of more potent immunosuppressant drugs following transplantation (48).
Some fungal species, including Histoplasma, Blastomyces, and Coccidioides, cause endemic fungal infections. Coccidioides species primarily infect individuals in the southwestern United States. In contrast, both Histoplasma and Blastomyces species are native to the Mississippi River Valleys and Ohio (49-53). The occurrence of endemic fungal infections after liver transplantation is rare, with an overall reported incidence of 0.2% (53). The main reasons for the occurrence of endemic fungal infections outside endemic regions include donor-derived infections, travel to remote areas, and reactivation (16).
3.2. Prevalence and Epidemiology of CNS Fungal Infections After LT
This section provides information on the prevalence and epidemiology of CNS fungal infections after liver transplantation. Aspergillus infections, affecting 1 to 9% of cases, are influenced by various factors such as surgery, immunosuppression, overall health, and medication. Understanding the prevalence and epidemiology of invasive aspergillosis (IA) is crucial for improving outcomes in liver transplant recipients (3).
Two separate studies conducted in Iran offer valuable insights into this matter. The study at Imam Khomeini Hospital, conducted from 2014 to 2019 and involving 850 liver transplant patients, found that the prevalence of IA was 2.7%. This study identified several risk factors, including elevated serum creatinine, the need for renal replacement therapy, specific induction therapies, post-transplant complications, bacterial pneumonia, prior antibiotic use, cytomegalovirus infection, and the duration of stay in the intensive care unit (54).
Conversely, the study at Montasryieh Hospital, carried out from August 2019 to August 2020 and involving 86 liver transplant recipients, reported a higher prevalence of IA, reaching 11%. The majority of patients (93.3%) experienced early-onset IA, with 80% of them diagnosed with pulmonary aspergillosis (55). Both studies emphasize the importance of early detection, targeted antifungal treatment, and understanding specific risk factors associated with IA in liver transplant recipients. These findings provide valuable insights into the epidemiology of IA and guide future interventions for better outcomes in Iranian liver transplant recipients.
Cryptococcus infections involving C. neoformans and C. gattii have an overall incidence of 0.3% to 5%, with C. gattii leading to increased mortality and CNS involvement (29, 56). Candida species, responsible for 68 to 93% of post-liver-transplant invasive fungal infections, show an increasing trend. A study in Spain reported an increase in C. glabrata cases from 18.8 to 30.4% between 2010 - 2011 and 2016 - 2018, while cases of C. albicans decreased. Non-albicans species may result in higher mortality, and prior azole use is linked to an increased isolation of C. glabrata (6, 57).
Invasive molds like Scedosporium, Mucomycetes, and Fusarium are infrequent after liver transplantation but are on the rise due to potent immunosuppression. Scedosporium species account for 25% of non-Aspergillus mold infections. The estimated incidence of mucormycosis in liver transplant recipients is 4 - 1.6%, and Fusarium typically manifests as a local infection, with disseminated fusariosis being rare (44).
It is important to note significant CNS involvement in brain fungal infections post-liver transplant, particularly with Cryptococcus species, where 54 to 62% of patients develop CNS disease (56). Table 2 summarizes the prevalence and associated risk factors for various fungal infections affecting the CNS post-liver transplantation, providing a comprehensive overview for monitoring and managing complications, especially those impacting the brain. Understanding these factors is vital for early diagnosis and the application of targeted therapies, ensuring optimal outcomes for recipients.
| Fungal Infection Type | Prevalence in Liver Transplant Recipients | Risk Factors | Ref. |
|---|---|---|---|
| Aspergillus | 1 - 9% | Prolonged surgical time, re-transplantation, steroid-resistant rejection, CMV infection, diabetes, broad-spectrum antibiotics | (3, 54, 55) |
| Imam Khomeini Hospital: 2.7% | Elevated serum creatinine, renal replacement therapy, specific induction therapies, post-transplant complications, bacterial pneumonia, prior antibiotic use, cytomegalovirus infection, duration of ICU stay | ||
| Montasryieh Hospital: 11% | Early-onset IA (93.3%), pulmonary aspergillosis (80%) | ||
| Cryptococcus | 0.3 – 5% | C. neoformans: Immunocompromised and immunocompetent; | (29, 56) |
| C. gattii: More severe in immunocompetent | |||
| CNS disease in 54 – 62% of cases | |||
| Candida | 68 – 93% | A broad range of species; increasing non-albicans cases over time | (6, 57) |
| Other Molds | Varies | Scedosporium: 25% of non-Aspergillus mold infections; | (44) |
| Fusarium: Rare dissemination |
Spectrum and Prevalence of Fungal Infections Following Liver Transplantation
3.3. Related Risk Factors for CNS Fungal Infections
Numerous factors are associated with the development of CNS fungal infections in liver transplant patients (58). Identifying high-risk patients for fungal infections can significantly aid in reducing diagnostic delays, predicting appropriate prevention strategies, decreasing the incidence of drug-resistant fungi, managing drug interactions, particularly with immunosuppressants, and alleviating overall healthcare costs (59).
Over the past few decades, multiple studies have focused on identifying these risk factors. Some prominent risk factors that significantly impact the incidence of Aspergillus and Candida infections include re-transplantation, CMV disease, post-liver transplantation hemodialysis, immunosuppression, fulminant hepatitis as an indication for liver transplantation, and prolonged transplantation duration (59-61).
3.4. The Association Between Fungal Infection and Prophylactic Drug Administration
Fungal infections caused by Aspergillus and Candida are among the most common infections following liver transplantation (62). In 2015, a retrospective study conducted by Eschenauer et al. examined three main groups that received targeted prophylaxis with voriconazole (54% of patients), fluconazole (5% of patients), and no antifungal drugs (38% of patients). Comparing these groups to a patient group that received universal prophylaxis with voriconazole revealed no statistically significant difference in the incidence of fungal infections (6.8% in targeted vs. 4.2% in universal). This led to the conclusion that a targeted approach to antifungal therapy in liver transplant patients offers advantages in terms of safety, cost-effectiveness, and reduced side effects (63).
Similarly, in 2016 in Spain, a comparison was made between high-risk patients who received caspofungin and those who received fluconazole. The results showed similar efficacy in preventing fungal infections in liver transplant recipients (64).
Echinocandins are important prophylactic agents, especially in regions with a high prevalence of drug-resistant non-Albicans Candida. However, their higher cost compared to fluconazole poses a limitation for less affluent countries (7).
Although prophylactic antifungal drugs are generally well-tolerated, they can contribute to drug-resistant Candida infections. Therefore, selecting the appropriate patients, agents, and drugs is a crucial step in prevention.
4. Conclusions
The high risk of fungal infection incidence in transplant recipients continues to lead to morbidity, mortality, and poor outcomes in patients. Early diagnosis and antifungal prophylaxis should be considered promptly in high-risk patients. Indeed, early identification of high-risk patients based on their risk factors for developing fungal infections can significantly improve patient outcomes. Ongoing research is essential to help identify high-risk patients and ensure timely and effective implementation of preventive measures. In the current era, future research, including randomized and collaborative prospective studies on antifungal prophylaxis in organ transplantation, should aim for a better definition of fungal infection in liver transplant recipients and identify effective risk factors.