1. Background
Dengue fever (DF) is primarily an urban disease of the tropics (1), but currently it has become a global problem (2). A study estimated that the incidence of dengue is 390 million per year (3). The incidence of dengue infection has an increase trend every year. World health organization reported that the incidence of dengue infection increased from 2.2 million in 2010 to 3.2 million in 2015 (4). A report using 1,636 country-years of case reports of dengue from 76 countries found a substantial increase in the incidence of dengue between 1990 and 2013, with the number of apparent cases more than doubling every decade, from 8.3 million (3.3 - 17.2 million) in 1990 to 58.4 million (23.6 - 121.9 million) in 2013 (5). The highest dengue incidence rates occurred in Southeast Asia, with an annual average of 34.3 cases per 1000 people (5).
Fluid therapy is the only treatment for the management of dengue infection to date and there is no specific treatment (6, 7). Vaccination is an effective method to prevent certain infectious diseases (8) and it is the most important achievement of public health (9). Effective dengue vaccine is difficult to develop because it has to protect against all four serotypes of dengue virus (10). Nevertheless, several dengue vaccine candidates (CYD, DENVax, TV003/TV005, TDENV PIV, V180, and D1ME100) have been tested in clinical trials (10) and one of them, CYD, has been approved in some countries. In vaccination programs, a new vaccine has the potential to bring a variety of problems. The problem of dengue vaccine that is categorized as a new vaccine is whether the public will accept and be willing to purchase the vaccine (11). If so, what attitudinal factors are associated with public hesitancy or acceptance and willingness to pay (WTP).
2. Objectives
The present study aimed to provide data regarding socioeconomic and attitudinal factors associated with acceptance and WTP towards dengue vaccine. This study sought to provide solid data that could be used to generate recommendations for vaccination program policy-makers.
3. Methods
3.1. Study Setting
A systematic review with a meta-analysis was conducted to assess the associated factors regarding acceptance and WTP towards dengue vaccine. Interested data from previous studies were collected for calculating combined odds ratios (ORs) and 95% confidence intervals (95% CIs) using fixed or random effect model. If the data were not qualified for meta-analysis, the data were described narratively. Articles were searched in PubMed and Embase (updated: September 10, 2016). The study was conducted on September-October 2016.
3.2. Study Procedures
The procedures of this study were: (1) identifying the potentially relevant studies through PubMed and Embase; (2) determining eligibility of the study; (3) collecting the abstract and full text data from the studies; (4) collecting the data for calculating OR95%CI; and (4) analyzing data statistically.
3.3. Eligibility Criteria and Data Extraction
Eligibility criteria consisted of predefined inclusion criteria. Studies were included in the analysis if they met the following inclusion criteria: (1) evaluating the factors associated with dengue vaccine acceptance or WTP towards dengue vaccine and (2) providing sufficient data for calculation of OR and 95%CI. If the data did not meet the inclusion criteria, the data were only described narratively.
3.4. Search Strategy and Literature
Potential studies, restricted to English, were searched using specified key words. The search strategy involved the use of combination of the following key words: dengue vaccine", "vaccine acceptance" and "willingness to pay". The reference lists of the retrieved articles were hand-searched. If more than one article was published using the same study data, only the study with the largest sample size was included.
3.5. Statistical Analysis
The association of explanatory factor with dengue vaccine acceptance and WTP was estimated by calculating pooled OR95%CI. The pooled ORs was determined by Z tests (P < 0.05 was considered statistically significant). A Q test was employed to evaluate whether the heterogeneity existed. Random effect model was used to calculate OR95%CI if heterogeneity existed (P < 0.10). Fixed effect model was used to calculate OR and 95%CI if no heterogeneity existed. These tests were performed if the data were qualified with inclusion and exclusion criteria. A comprehensive meta-analysis (CMA) 2.0 was used to analyze the data.
4. Results
4.1. Characteristics of the Studies
A total of 196 potentially relevant papers regarding vaccine acceptance and 107 papers regarding WTP were identified. Of these, 189 and 99 papers regarding vaccine acceptance and WTP were excluded, respectively, due to obvious irrelevance by reading their titles and abstracts. After reading the full texts, five additional papers regarding vaccine acceptance were excluded because they did not provide sufficient data for calculation of OR95%CI. Therefore, two studies regarding dengue vaccine acceptance were included in the meta-analysis (12, 13). While, all papers (eight papers) regarding WTP for dengue vaccine were excluded because they were not qualified to calculate OR95%CI. Nevertheless, four papers regarding WTP for dengue vaccine were included for narrative review (12, 14-16).
4.2. Quantitative Data Synthesis and Source of Heterogeneity Regarding Vaccine Acceptance
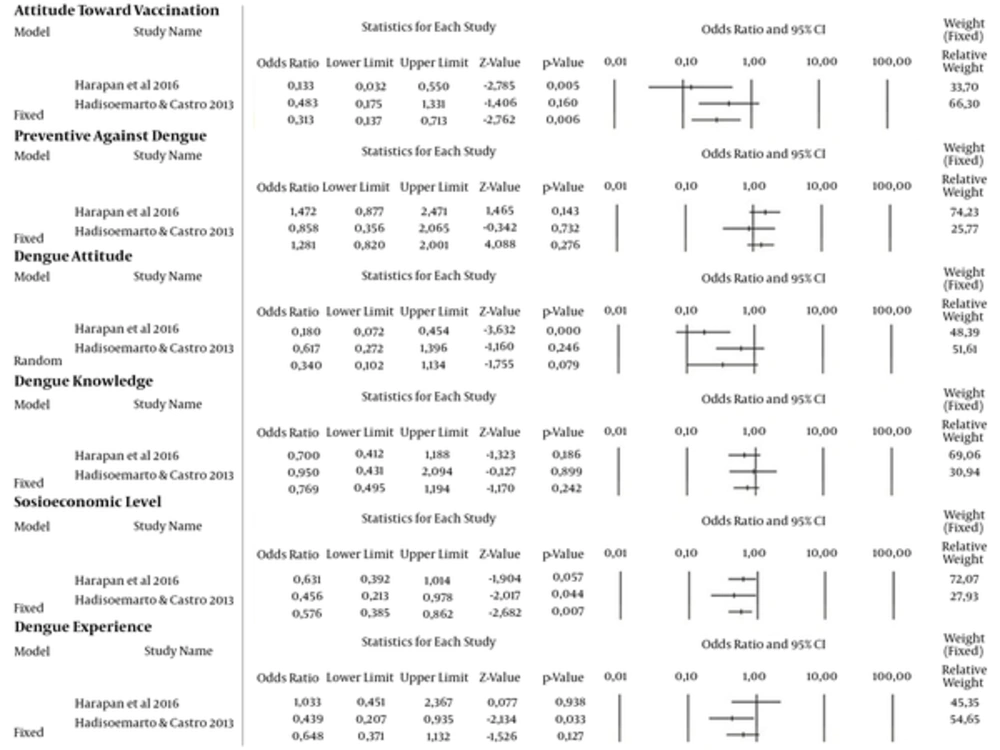
In total, 1151 participants from two studies regarding dengue vaccine acceptance were identified (12, 13). The results showed that attitude toward vaccination (OR95%CI = 0.313 [0.137 - 0.713], P = 0.006) and socioeconomic level (OR95%CI = 0.576 [0.385 - 0.862], P = 0.007) had significant associations with dengue vaccine acceptance. While, other variables including preventive measures against dengue (OR95%CI = 1.281 [0.820 - 2.001], P = 0.276), attitude towards dengue (OR95%CI = 0.340 [0.102 - 1.134], P = 0.079), knowledge on dengue (OR95%CI = 0.769 [0.495 - 1.194], P = 0.242), and dengue experience (OR95%CI = 0.648 [0.371 - 1.132], P = 0.127) had no association with dengue vaccine acceptance. See Table 1 and Figure 1 for details.
| Factor | Location (Reference) | Sample Size (n) | Poor (n) | Good (n) | OR (95%CI) | P | ph | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Poor | Good | Willing | Not | Willing | Not | |||||
| Socioeconomic level | Aceh (13) | 261 | 391 | 222 | 39 | 352 | 39 | 0.576 (0.385 - 0.862) | 0.007 | 0.480 |
| Bandung (12) | 198 | 292 | 181 | 17 | 280 | 12 | ||||
| Attitude towards vaccination | Aceh (13) | 555 | 97 | 479 | 76 | 95 | 2 | 0.313 (0.137 - 0.713) | 0.006 | 0.147 |
| Bandung (12) | 48 | 451 | 43 | 5 | 427 | 24 | ||||
| Preventive measures against dengue | Aceh (13) | 497 | 155 | 442 | 55 | 131 | 24 | 1.281 (0.820 - 2.001) | 0.276 | 0.299 |
| Bandung (12) | 108 | 392 | 101 | 7 | 370 | 22 | ||||
| Dengue attitude | Aceh (13) | 489 | 163 | 416 | 73 | 158 | 5 | 0.340 (0.102 - 1.134) | 0.079 | 0.051 |
| Bandung (12) | 110 | 384 | 101 | 9 | 364 | 20 | ||||
| Dengue knowledge | ||||||||||
| Dengue experience | Aceh (13) | 595 | 57 | 524 | 71 | 50 | 7 | 0.648 (0.371 - 1.132) | 0.127 | 0.135 |
| Bandung (12) | 151 | 349 | 137 | 14 | 334 | 15 | ||||
Factors Associated with Dengue Vaccine Acceptance (Willingness vs. Not-Willingness)
Evidence for heterogeneity between studies was found in the attitude towards dengue variable (P = 0.051); therefore, the data were assessed using random effect model. Evidence for heterogeneity was not found regarding other variables including attitude towards vaccination (P = 0.147), socioeconomic level (P = 0.480), preventive measures against dengue (P = 0.299), knowledge on dengue (P = 0.528), and dengue experience (P = 0.135). Therefore, fixed effect model was used to calculate OR95%CI.
4.3. Narrative Review Regarding Willingness to Pay Towards Dengue Vaccine
Narrative review was used to analyze WTP towards dengue vaccine because the data were not qualified for meta-analysis. In four studies (12, 14-16), there were 12 factors that were assessed related to WTP towards dengue vaccine. They were attitude towards vaccination, preventive measures against dengue, attitude towards dengue, knowledge on dengue fever, knowledge on dengue viruses, socioeconomic levels, dengue experience, knowing someone who had dengue, vaccine price, having family member(s) suffering from dengue, and previous vaccine purchase. Of those, preventive measures against dengue (P = 0.029; P < 0.05; P = 0.036) (14-16), attitude towards dengue (P = 0.005) (14), knowledge on dengue fever (P = 0.050; P = 0.024) (12, 16), knowledge on dengue viruses (P = 0.028) (14), socioeconomic levels (P < 0.01) (12, 15), dengue experience (P = 0.041), and vaccine price (P < 0.01) (15) were associated with WTP. Other factors had no significant association with WTP towards dengue vaccine (Table 2).
| Country (n) | Variables | OR (95%CI) or Correlation Coefficient | P | Reference |
|---|---|---|---|---|
| Indonesia (476) | Attitude towards vaccination | 0.249 (-0.028 - 0.526) | 0.078 | (14) |
| Preventive measures against dengue | 0.232 (0.024 - 0.440) | 0.029 | ||
| Dengue attitude | 0.340 (0.105 - 0.576) | 0.005 | ||
| Dengue fever knowledge | -0.114 (-0.318 - 0.089) | 0.271 | ||
| Dengue viruses knowledge | 0.231 (0.025 - 0.437) | 0.028 | ||
| Socioeconomic levels | -0.086 (-0.351 - 0.178) | 0.522 | ||
| Dengue experience | 0.202 (-0.143 - 0.548) | 0.251 | ||
| Indonesia (438) | Socioeconomic levels | 0.563 (0.280 - 0.847) | < 0.01 | (12) |
| Preventive measures against dengue | -0.038 (-0.247 - 0.171) | 0.72 | ||
| Dengue fever knowledge | 0.227 (0.01 - 0.44) | 0.05 | ||
| Knowing someone who had dengue | 0.129 (-0.04 - 0.30) | 0.15 | ||
| Philippines (205) | Dengue viruses knowledge | -0.017 | > 0.05 | (15) |
| Dengue fever knowledge | -0.138 | > 0.05 | ||
| Preventive measures against dengue | 0.367 | < 0.05 | ||
| Have family member(s) who suffered from dengue | 0.081 | > 0.05 | ||
| Vietnam (386) | Dengue fever knowledge | NA | 0.024 | (16) |
| Dengue experience | NA | 0.041 | ||
| Preventive measures against dengue | NA | 0.036 | ||
| Previous vaccine purchase | NA | 0.08 | ||
| Thailand (379) | Dengue fever knowledge | NA | 0.061 | (16) |
| Dengue experience | NA | 0.043 | ||
| Preventive measures against dengue | NA | 0.173 | ||
| Colombia (392) | Dengue fever knowledge | NA | 0.084 | (16) |
| Dengue experience | NA | 0.084 | ||
| Preventive measures against dengue | NA | 0.059 | ||
| Previous vaccine purchase | NA | 0.114 |
Factors Associated with Willingness to Pay Towards Dengue Vaccine
5. Discussion
5.1. Factors Associated with Dengue Vaccine Acceptance
Vaccine acceptance is an important predictor to determine the acceptance of the society of the vaccine. Vaccine acceptance is a problem that may arise to new vaccines including dengue vaccine. Data regarding dengue vaccine acceptance is very limited. However, several studies had reported vaccine acceptance in the context of other diseases (17-20) and they were very helpful for immunization programs. We reviewed several factors associated with dengue vaccine acceptance. Until now (updated-January 2, 2017), only two studies (11, 12) evaluated factors associated with dengue vaccine acceptance. Although there were several factors associated with vaccine acceptance from individual study (attitude towards vaccination, preventive measures against dengue, attitude towards dengue, knowledge on dengue fever, socioeconomic level, and dengue experience), our meta-analysis revealed that only attitude towards vaccination and socioeconomic level had significant associations with dengue vaccine acceptance.
Attitude towards vaccination is an individual perspective toward the vaccination program and it was revealed to be correlated with vaccination coverage rates (21). Attitude towards vaccination was shown to be associated with acceptance towards vaccine against infectious diseases such as H1N1 (22), measles (23), rubella (23), and human papillomavirus (24). These results indicate that a society with a good attitude towards vaccination has a tendency to be able to receive a new vaccine. Therefore, to improve dengue vaccine acceptance and increase community attitude, the socialization of dengue vaccine might be essential.
Our meta-analysis data also showed that dengue vaccine acceptance was associated with socioeconomic level. Other studies also revealed consistent findings in the context of other infectious diseases including human papillomavirus (25, 26), influenza (27), and cholera (28). These results suggest that high socioeconomic level is closely associated with better dengue vaccine acceptance. Therefore, to improve the dengue vaccine acceptance, socialization programs should intensively target populations with low socioeconomic level.
5.2. Factors Associated with Willingness to Pay Towards Dengue Vaccine
We evaluated several factors that had the possibility to be correlated with WTP towards dengue vaccine and tried to conduct meta-analysis, but the data were not suitable for meta-analysis. Therefore, we analyzed the data narratively. There were four studies identified with different results (Table 2).
First, a study by our group found that preventive measures against dengue, attitude towards dengue, and knowledge on dengue viruses were associated with WTP (14). Second, another study in Bandung showed that only knowledge on dengue fever and socioeconomic levels were associated with WTP (12). Third, a study in Metro Manila (Philippines) found that vaccine price, socioeconomic levels, and preventive measures against dengue were associated with WTP. The last study was conducted in Vietnam, Thailand, and Colombia (16). In Vietnam, knowledge on dengue fever, dengue experience, and preventive measures against dengue had significant associations with WTP, while among Thai only dengue experience was associated with WTP. Interestingly, none of the variables was associated with WTP towards dengue vaccine in Colombia.
One of interesting finding is no constant association between socioeconomic status and WTP. Our study (14) revealed no association but another study in Indonesia (12) showed a strong association. It might indicate that the socioeconomic variable behaves differently across regions in Indonesia due to the diverse contexts of local specific situations.
There are some limitations in this study. First, false positive findings regarding dengue vaccine acceptance could occur due to small sample size even when combined. Second, data regarding WTP towards dengue vaccine could not be analysed statistically and therefore, they were analyzed using narrative review. Third, studies regarding dengue vaccine acceptance and WTP towards dengue vaccine were very limited and therefore, they could not be explored specifically.
5.3. Conclusion
The meta-analysis reveals that attitude towards vaccination and socioeconomic status are associated with dengue vaccine acceptance while other variables (preventive measures against dengue, attitude towards dengue, knowledge on dengue, and dengue experience) have no association. Limited data suggest that some factors are associated with WTP towards dengue vaccine including socioeconomic level and attitudinal factors such as knowledge on dengue fever and dengue viruses, attitude towards dengue, preventive measures against dengue, and dengue experience.