1. Background
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, has profoundly impacted global health, economies, and social well-being (1). Over recent years, a new variant of the virus, named Omicron, has emerged and rapidly spread worldwide, posing significant challenges to public health systems. The Omicron variant is characterized by numerous mutations in the spike protein, which plays a crucial role in viral entry into host cells. The increased transmissibility and potential for immune evasion exhibited by this variant have raised concerns about its impact on vaccine effectiveness (2, 3).
Vaccination remains the cornerstone of strategies to control the COVID-19 pandemic (4). The rapid development and deployment of vaccines have provided hope for reducing the burden of disease and returning to a sense of normalcy (5, 6). However, the continuous evolution of the virus and the emergence of new variants necessitate ongoing evaluation of vaccine efficacy against these variants (7). Understanding the effectiveness of COVID-19 vaccines in preventing and mitigating Omicron variant infections is crucial for guiding public health interventions and vaccine deployment strategies (8). Evaluating vaccine effectiveness in real-world settings provides valuable insights into the performance of vaccines under natural conditions and informs evidence-based decision-making (9).
The effectiveness of anti-COVID vaccines can be influenced by various variables (10). One crucial variable is the individual's immune response, which can vary based on factors such as age, underlying health conditions, and prior exposure to the virus. Additionally, the vaccine's effectiveness may differ across different variants of the virus, including emerging strains like the Omicron variant. The timing and completeness of the vaccination regimen also play a significant role in vaccine effectiveness (11). It is crucial to adhere to the recommended dosage schedule and receive all the required doses of the vaccine to maximize protection. Studies have shown that two doses of most COVID-19 vaccines provide higher effectiveness compared to a single dose. Additionally, maintaining immunity through booster shots, as recommended by health authorities, can further enhance vaccine effectiveness, especially in the face of new variants or waning immunity over time (12). Factors such as vaccine storage conditions, transportation, and administration techniques also contribute to the overall effectiveness of the vaccine (13). Ongoing studies and monitoring of vaccine effectiveness against these variants are essential to ensure optimal protection (14).
Anti-COVID vaccines have been instrumental in reducing the risk of death in patients (15). One category of vaccines that has shown efficacy in this regard is the non-vector-based vaccines, such as mRNA vaccines. These vaccines work by introducing a small piece of the virus's genetic material into the cells, triggering the production of a harmless viral protein. This stimulates an immune response, leading to the development of protective antibodies (15). Studies have demonstrated that mRNA vaccines significantly reduce the chances of severe illness, hospitalization, and death in individuals who have received the full vaccination regimen. The mRNA vaccines, such as the COVID-19 Sinopharm and SpikoGen vaccines, have been highly effective in preventing COVID-19 and its variants, including the Omicron variant (16).
Another category of vaccines that has proven effective in reducing the risk of death is the viral vector-based vaccines. Examples include the Oxford-AstraZeneca vaccines (17). Viral vector vaccines use a harmless virus as a carrier to deliver genetic material from the target virus. This genetic material prompts the production of viral proteins, triggering an immune response (18). These vaccines have demonstrated effectiveness in preventing severe disease and reducing the likelihood of death among vaccinated individuals. They provide a valuable tool in mitigating the impact of COVID-19 and preventing fatalities (19, 20).
While both vector-based and non-vector-based vaccines have shown efficacy in preventing and mitigating Omicron variant infections, there are some differences to consider (21). Vector-based vaccines typically require a single or double dose, depending on the specific vaccine, while non-vector-based vaccines, like mRNA vaccines, usually require two doses for full immunization (22). Additionally, storage and distribution requirements may differ between the two types of vaccines, with non-vector-based vaccines often requiring ultra-cold storage. Both types of vaccines have undergone rigorous testing and have been approved by regulatory authorities, providing important tools in the fight against the Omicron variant (21, 23).
2. Objectives
The present study aimed to examine the impact of COVID-19 vaccination on mortality rates among patients admitted to hospitals. This study also analyzes the characteristics of COVID-19 patients, their clinical presentations, comorbidities, and factors linked to mortality in hospitals associated with Mashhad University of Medical Sciences in Iran’s Razavi-Khorasan province. The outcome of this study explored potential variations in vaccine effectiveness across different vaccine types, age groups, and comorbidities. The study utilized data from multiple healthcare facilities in Mashhad, ensuring a diverse and representative sample of the population. This study provided a valuable opportunity to assess the real-world effectiveness of COVID-19 vaccines against the Omicron variant.
The findings of this study have important implications for public health authorities and healthcare professionals. The results inform vaccination strategies, guide public health interventions, and support evidence-based decision-making to mitigate the impact of the Omicron variant.
3. Methods
The study was conducted over a period of one year, from January 2021 to September 2022. It aimed to investigate the characteristics of COVID-19 patients, their clinical presentations, comorbidities, and the factors associated with mortality in those admitted to hospitals affiliated with Mashhad University of Medical Sciences in Razavi-Khorasan province, Iran.
3.1. Data Collection
Data were collected from the medical care monitoring system (MCMC) established by Mashhad University of Medical Sciences at the start of the pandemic in Iran to monitor COVID-19 patients in the country. The data from the MCMC in Razavi-Khorasan province are collected from six medical universities/faculties of the province and are continuously updated 24 hours a day. Moreover, the recorded information in the MCMC is matched with the patient’s information in the disease management portal in the Deputy of Health and hospital information system (HIS) of the medical universities. These facilities provide a diverse and representative sample of the population, allowing for robust analysis of vaccine effectiveness across different demographic and clinical characteristics. Prior to the statistical analysis of the demographics and clinical presentations of patients, researchers conducted data quality control and eliminated any duplicate reports from further evaluation.
3.2. Study Population
The study included patients who were admitted to hospitals in the area covered by Mashhad University of Medical Sciences due to definite or suspected reasons of COVID-19 infection with a positive PCR. This study was conducted in accordance with ethical guidelines and principles. The main exposure variable in this study is vaccination status. Vaccines are categorized into two groups based on their types: Vector-based and non-vector-based vaccines. The outcome of the study included the measurement of mortality and recovery of hospitalized patients infected with the Omicron variant among the vaccinated and unvaccinated groups.
3.3. Data Analysis
Data analysis involved the use of SPSS software to perform descriptive statistics and inferential analyses. The association between vaccination status and Omicron variant infections was assessed using logistic regression analysis. Odds ratios and corresponding 95% confidence intervals were calculated to estimate vaccine effectiveness. The significance level was set at 0.05, and confidence intervals were calculated to assess the precision of the results. Subgroup analyses were conducted to explore potential effect modifiers and assess the consistency of vaccine effectiveness across different strata.
The model used death or recovery as the response variable and included variables such as age, gender, number of days between symptom onset and hospitalization, SpO2 level, length of hospital stay (per day), and two types of vaccines (vector-based and non-vector-based) as separate inputs. Additionally, a dummy variable was used to account for the presence of underlying diseases, which varied among the subjects.
4. Results
Between January 2021 and September 2022, the 6th and 7th peaks of COVID-19 affected Iran, particularly in the area covered by Mashhad University of Medical Sciences. The Omicron variant was the most prevalent strain during this time. A total of 28,253 people were admitted to hospitals in the area due to suspected or confirmed COVID-19 infection, with 30% testing positive (8,616 people). The ratio of positive deaths to positive hospitalizations was 9.6. To ensure concordance with global studies, further analysis was performed only on individuals who had a positive PCR test.
Due to the variety of vaccines in three doses, the vaccines that the patients in this study received were divided into two categories: Vector-based and non-vector-based (Table 1). The distribution of the disease was nearly equal between genders, with 50% of patients being women and 50% being men. The most prevalent underlying disease was hypertension, accounting for 23% of cases, followed by diabetes and heart disease (Tables 2 and 3) indicates that men outnumbered women in every age group, except for the 19 - 49 age group where women accounted for 62% of hospitalized patients. The age group with the highest percentage of deaths (16%) was those aged 70 years and above. Table 4 displays the percentage of deaths in various age groups.
| Groups | Vaccine Name |
|---|---|
| Vector-based | COVID 19-AstraZeneca, COVID 19-Sputnic |
| Non-vector-based | COVID 19-Bharat Biotech, COVID 19-Sinopharm, COVIranBarakat, SpikoGen, SOBERANA 02, Razi Cov Pars, PASTOCOVAC Plus, FAKHRAVAC |
| Comorbidities | Yes | No |
|---|---|---|
| Cancer | 299 (3) | 8317 (97) |
| Chronic liver diseases | 61 (1) | 8555 (99) |
| Diabetic | 1290 (15) | 7326 (85) |
| Chronic blood diseases | 43 (< 1) | 8573 (≈ 100) |
| HIV/AIDS | 12 (< 1) | 8604 (≈ 100) |
| Immunodeficiency (acquired or congenital) | 23 (< 1) | 8593 (≈ 100) |
| Heart disease | 1097 (13) | 7519 (87) |
| Chronic kidney diseases | 233 (3) | 8383 (97) |
| Asthma | 218 (3) | 8398 (97) |
| Other chronic lung diseases except asthma | 318 (4) | 8298 (96) |
| Chronic neurological disorders | 164 (2) | 8452 (98) |
| History of hypertension | 2013 (23) | 6603 (77) |
a Values are expressed as No. (%).
| Age Group (y) | Female | Male | Total |
|---|---|---|---|
| 0 - 5 | 142 (39) | 218 (61) | 360 |
| 6 - 18 | 185 (46) | 213 (54) | 398 |
| 19 - 49 | 1264 (62) | 760 (38) | 2024 |
| 50 - 59 | 411 (49) | 423 (51) | 834 |
| 60 - 69 | 648 (47) | 735 (53) | 1383 |
| > 70 | 1509 (46) | 1755 (54) | 3264 |
a Values are expressed as No. (%).
| Age Group (y) | Recovered | Death | Total |
|---|---|---|---|
| 0 - 5 | 359 (100) | 1 (0) | 360 |
| 6 - 18 | 387 (97) | 11 (3) | 398 |
| 19 - 49 | 1968 (97) | 56 (3) | 2024 |
| 50 - 59 | 767 (92) | 67 (8) | 834 |
| 60 - 69 | 1244 (90) | 139 (10) | 1383 |
| > 70 | 2728 (84) | 536 (16) | 3264 |
a Values are expressed as No. (%).
Out of the hospitalized patients infected with COVID-19, 40% had not received any vaccine and only 2% had received four doses (Table 5). Individuals who received four doses of the vaccine were not included in the study due to the short time between receiving the fourth dose and being hospitalized. Each additional year of age increased the risk of death by 1.04 times (P < 0.001). There was no significant difference in death rates between men and women with COVID-19 infection (P = 0.06).
| Doses | No. (%) |
|---|---|
| 0 | 3445 (40) |
| 1 | 395 (5) |
| 2 | 2273 (26) |
| 3 | 2290 (27) |
| 4 | 213 (2) |
| Total | 8616 (100) |
After analyzing the data, it was found that the duration of hospital visits following the first symptoms did not significantly impact the likelihood of death (P = 0.13). However, for individuals with SpO2 levels below 93, the risk of death increased by 1.74 times (P < 0.001). Additionally, for each additional day spent in the hospital, the probability of death rose by 1.05 times (P < 0.001).
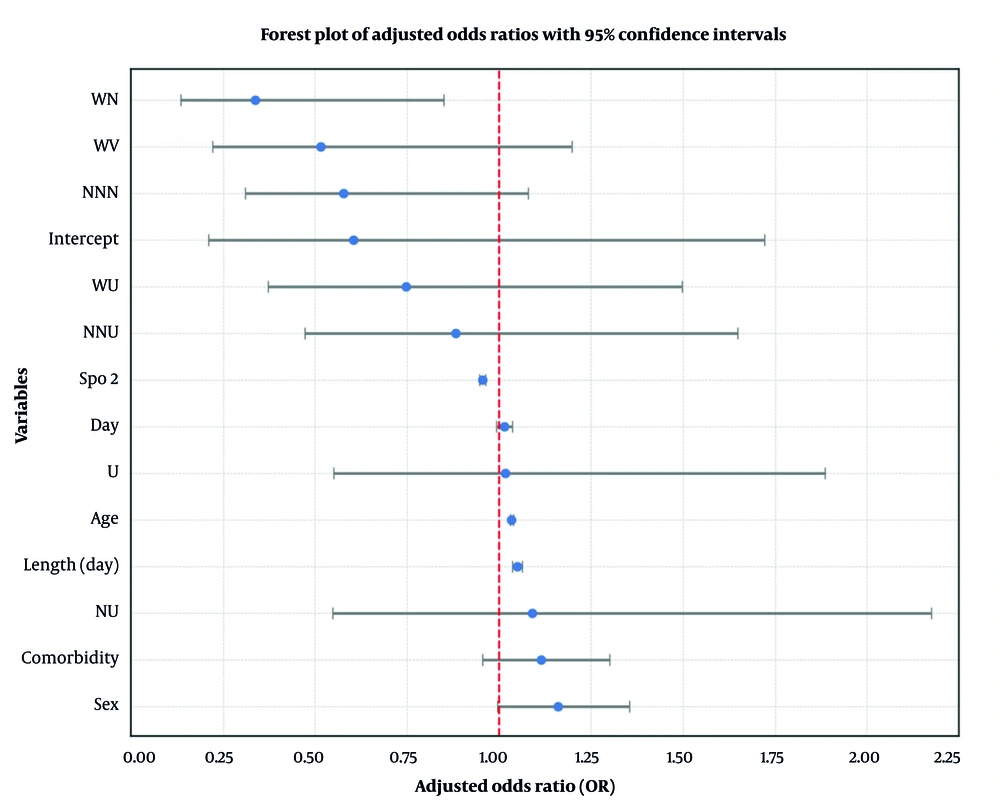
To compare the effectiveness of different vaccines, individuals who were not vaccinated were used as the baseline group. The risk of death from COVID-19 was then measured in relation to this group. The study found no significant difference in the likelihood of death between unvaccinated patients and those who had received a single dose of a non-vector-based vaccine (P = 0.835). Furthermore, the VVU group did not have a higher risk of death than the unvaccinated group (P = 0.059).
Receiving two doses of a vector-based vaccine and one dose of a non-vector-based vaccine (VVN) can protect against death from COVID-19, reducing the chances of dying by one-third compared to those who are not vaccinated (P = 0.002). The NNU group did not show any significant difference in death rates compared to the non-vaccinated group. Those who received three doses of vector-based (VVV) or three doses of non-vector-based (NNN) vaccines had a 50% reduction in the chances of dying compared to those who were not vaccinated. Having at least one underlying disease increases the chances of dying by 1.17 times (P = 0.048).
Tables 6 and 7 provide details of the coefficients of logistic regression, while Figure 1 illustrates the effectiveness of all types of vaccines.
| Variables | Β | P-Value a | Exp (β) | 95% CI for EXP (β) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Sex | -2.38 | < 0.001 | 0.09 | 0.08 | 0.10 |
| Age | -4.57 | < 0.001 | 0.01 | 0.01 | 0.01 |
| Day b | -2.41 | < 0.001 | 0.09 | 0.08 | 0.10 |
| SpO2 | 3.56 | < 0.001 | 35.16 | 17.85 | 69.34 |
| Length (d)c | -2.54 | < 0.001 | 0.08 | 0.07 | 0.09 |
| U | -2.25 | < 0.001 | 0.10 | 0.10 | 0.12 |
| NU | -2.26 | < 0.001 | 0.10 | 0.10 | 0.11 |
| VVU | -2.25 | < 0.001 | 0.10 | 0.10 | 0.11 |
| VVN | -2.24 | < 0.001 | 0.11 | 0.10 | 0.11 |
| NNU | -2.27 | < 0.001 | 0.10 | 0.10 | 0.11 |
| VVV | -2.25 | < 0.001 | 0.11 | 0.10 | 0.11 |
| NNN | -2.20 | < 0.001 | 0.11 | 0.10 | 0.12 |
| Comorbidity | -2.42 | < 0.001 | 0.09 | 0.08 | 0.10 |
Abbreviations: SpO2, oxygen saturation; U, unvaccinated; NU, non vector based, unvaccinated; VVU, vector based, vector based, unvaccinated; VVN, vector based, vector based, non vector based; NNU, nonvector based, nonvector based, unvaccinated; VVV, vector based, vector based, vector based; NNN, nonvector based, nonvector based, nonvector based.
a A P-value < 0.05 is considered statistically significant.
b The number of days of referral after the onset of symptoms.
c Length of hospitalization.
| Variables | Β | P-Value | Exp (β) | 95% CI for EXP (β) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Intercept | -0.50 | 0.34 | 0.60 | 0.21 | 1.72 |
| Sex | 0.15 | 0.06 | 1.16 | 1.00 | 1.35 |
| Age | 0.03 | < 0.001 a | 1.03 | 1.03 | 1.04 |
| Day b | 0.01 | 0.19 | 1.01 | 0.99 | 1.04 |
| SpO2 | -0.05 | < 0.001 a | 0.96 | 0.95 | 0.96 |
| Length (d)c | 0.05 | < 0.001 a | 1.05 | 1.04 | 1.06 |
| U | 0.02 | 0.95 | 1.02 | 0.55 | 1.89 |
| NU | 0.09 | 0.80 | 1.09 | 0.55 | 2.17 |
| VVU | -0.29 | 0.41 | 0.75 | 0.37 | 1.50 |
| VVN | -1.09 | 0.02 a | 0.34 | 0.13 | 0.85 |
| NNU | -0.13 | 0.69 | 0.88 | 0.47 | 1.65 |
| VVV | -0.66 | 0.12 | 0.52 | 0.22 | 1.20 |
| NNN | -0.55 | 0.09 | 0.58 | 0.31 | 1.08 |
| Comorbidity | 0.11 | 0.16 | 1.12 | 0.96 | 1.30 |
Abbreviations: SpO2, oxygen saturation; U, unvaccinated; NU, non vector based, unvaccinated; VVU, vector based, vector based, unvaccinated; VVN, vector based, vector based, non vector based; NNU, nonvector based, nonvector based, unvaccinated; VVV, vector based, vector based, vector based; NNN, nonvector based, nonvector based, nonvector based.
a A P-value < 0.05 is considered statistically significant.
b The number of days of referral after the onset of symptoms.
c Length of hospitalization.
5. Discussion
The SARS-CoV-2 pandemic has greatly affected global health and economies. The emergence of the new Omicron variant poses challenges for public health systems worldwide (24). The primary objective of this study was to examine the impact of COVID-19 vaccination on the mortality rates of hospitalized patients infected with the Omicron strain. Even as three years have elapsed since the onset of the COVID-19 pandemic and extensive vaccination campaigns have been carried out, assessing the efficacy of various vaccine formulations remains pivotal, not only for the current pandemic but also for potential future outbreaks of similar diseases.
In our investigation, we meticulously considered several confounding variables, including age, gender, blood oxygen levels (SpO2), and the duration of hospitalization. To comprehensively account for the diversity of vaccines administered, we categorized them into two groups: Vector-based and non-vector-based. Additionally, we introduced a vaccine type variable, which was a function of both the number of vaccine doses received and the specific vaccine type, into our logistic model.
Our findings align with prior research, such as the meta-analysis conducted by Romero Starke et al., which highlighted the undeniable association between age and COVID-19 mortality. In this study, age emerged as a statistically significant factor (P < 0.001), with each year of increasing age correlating with a 3% higher likelihood of mortality among hospitalized COVID-19 patients (25). Our study investigated the relationship between COVID-19 mortality, age, and vaccine administration, unlike Romero Starke et al.’s (25) meta-analysis, which did not consider the vaccine variable. We found a significant association between age and COVID-19 mortality (P < 0.001).
Similarly, the study by Pan et al., which centered on 124 hospitalized COVID-19 patients, emphasized the significance of SpO2 alongside variables like age, high blood pressure, and diabetes (26). Our research corroborated these findings, revealing that for every incremental unit increase in SpO2, the survival rate surged by a substantial 74% (P < 0.001).
However, our study introduced a novel perspective by examining the influence of hospitalization duration. Contrary to expectations, we observed that each additional day spent in the hospital amplified the chance of death by 5%. This may be attributed to sicker patients being more prone to extended hospital stays and consequently facing an elevated risk of contracting hospital-acquired infections (P < 0.001). Intriguingly, a study by da Costa Sousa et al. contradicted our findings, suggesting that longer hospital stays might actually diminish the likelihood of death (27).
Based on the data analysis, there was no notable discrepancy in the mortality rates of men and women who contracted COVID-19 (P = 0.06). Furthermore, the duration of hospital stays after the onset of symptoms did not have a significant effect on the probability of death (P = 0.13). When scrutinizing the impact of vaccine dosing, our research revealed that receiving a single vaccine dose did not yield a statistically significant reduction in COVID-19-related deaths (P = 0.85). Furthermore, due to the initial predominance of non-vector vaccines in Iran, we were unable to compare the outcomes of a single dose of a non-vector vaccine with that of a single dose of a vector-based vaccine.
The study conducted by Corchado-Garcia et al. in 2021 revealed interesting findings about the effectiveness of the vector-based vaccine Ad26.COV2.S (28). While their research focused on the risk of infection, our study went further by analyzing mortality outcomes. Despite these findings, our study detected no significant difference in the death rates between those who received two doses of vector-based vaccines, those who received two doses of non-vector-based vaccines, and the unvaccinated (P = 0.059 and P = 0.229, respectively). However, the unvaccinated group showed a slight trend toward significance when it came to those who had received two vaccine doses (Table 6).
A study conducted by Sirison et al. in 2023, examining the cost-effectiveness of booster doses during the Omicron variant epidemic, yielded noteworthy insights. Their research explored three scenarios: No booster, a vector-based booster dose, and an mRNA booster dose, and revealed a threefold reduction in mortality rates in scenarios involving viral vector and mRNA boosters compared to the non-booster scenario (29). In our study, the ratios of death for individuals who received two doses of vector-based vaccines and a vector-based booster, as well as those who received two doses of non-vector-based vaccines and a non-vector-based booster, were found to be significantly reduced (P = 0.013 and P < 0.001, respectively) compared to the unvaccinated.
Lastly, we delved into the impact of comorbidities on the mortality of COVID-19 patients, considering numerous studies on the subject. Our investigation assessed vaccine efficacy while controlling for the presence of at least one underlying condition, and it was revealed that having at least one comorbidity increased the risk of death by approximately 16% in COVID-19 patients (Table 6). In the study by Adab et al., diabetes emerged as the most prevalent comorbidity among COVID-19 patients, followed closely by hypertension, with corresponding mortality rates of 17.1% and 7.8% (30).
Our study highlights the significance of classifying vaccines by their production platforms in assessing their efficacy, despite the numerous challenges presented by different COVID-19 virus variants. Our findings suggest the need for booster shots and bring attention to the constraints related to vaccine diversity in Iran, which limited our analysis of a wider range of vaccine types.
5.1. Conclusions
In conclusion, our study examined how COVID-19 vaccination, patient demographics, comorbidities, and hospitalization outcomes are interconnected in the context of the Omicron strain. It is evident from our findings that age remains a critical factor, with each additional year significantly elevating the risk of COVID-19-related mortality among hospitalized patients. Likewise, maintaining higher SpO2 emerged as a robust indicator of improved survival. Furthermore, the duration of hospitalization, a less explored parameter, revealed an unexpected trend, suggesting that longer hospital stays might contribute to a heightened risk of mortality, potentially due to the susceptibility of sicker patients to hospital-acquired infections.
In the realm of vaccines, our study underscores the vital importance of booster doses in reducing COVID-19 mortality rates, especially in the context of the Omicron variant. Notably, our research discerned substantial reductions in mortality risk for individuals receiving certain vaccine formulations and boosters. However, the diversity of vaccine types introduced challenges in assessing their efficacy comprehensively. Additionally, our investigation found that comorbidities, particularly diabetes and hypertension, significantly increased the risk of death among COVID-19 patients, highlighting the critical need for tailored medical care for individuals with underlying health conditions.
In light of these findings, we emphasize the importance of continued research into the nuanced dynamics of COVID-19 vaccination, age-related risks, hospitalization effects, and the impact of comorbidities. Such insights are invaluable not only for managing the ongoing pandemic but also for shaping future strategies to combat emerging infectious diseases. Furthermore, our study underscores the value of standardized vaccine categorization based on production platforms to facilitate more precise assessments of vaccine effectiveness.
In conclusion, our research contributes to the evolving body of knowledge surrounding COVID-19 and provides essential insights that can inform public health strategies, vaccination campaigns, and clinical care protocols as we navigate the complex landscape of infectious disease management.