1. Background
The Joint United Nations Programme on HIV/AIDS (UNAIDS) has proposed the goal of “Global elimination of acquired immune deficiency syndrome (AIDS) by 2030.” However, the latest data suggests that in 2022, there were 39 million people living with HIV (PLWH) worldwide, with 1.3 million new infections and 630,000 AIDS-related deaths (1). These statistics indicate that the world is struggling to achieve this goal. Acquired immune deficiency syndrome remains one of the main public health problems in China (2). Although the prevalence of AIDS is low, it remains a significant risk, particularly for a country like China with its very large population. China still reported a large number of deaths from HIV/AIDS each year, making it the most reported infectious disease in terms of deaths (3-5). The prevention and control of AIDS in China face severe challenges. Guangxi is one of the regions with the most severe AIDS epidemic in China. From 2010 to 2020, approximately 10,000 new cases were reported, with 5,000 deaths, and the mortality rate of PLWH under treatment was 2.19 per 100 person-years in 2020 (6). Baise is a multiethnic city with an underdeveloped economy and health facilities in Guangxi.
In 1996, highly active antiretroviral therapy (HAART) was introduced, greatly reducing the morbidity and mortality of AIDS (7). In 2015, WHO recommended that all HIV-infected patients should undergo antiretroviral therapy (ART) regardless of CD4+ T cell count (8). This strategy, called “Test and Treat,” meant that treatment would be initiated immediately after an HIV diagnosis. In June 2016, China began implementing the “Test and Treat” strategy. Antiviral treatment for all HIV-infected people is beneficial for expanding treatment coverage. Studies have shown that early initiation of ART and effective ART reduced PLWH mortality, narrowed the life expectancy gap between PLWH and the general population, and even allowed PLWH to reach the life expectancy of the average person (9-11).
2. Objectives
The main purpose of this study was to comprehensively analyze the specific circumstances of PLWH deaths in Baise from 2017 to 2022. This included assessing the all-cause and AIDS-related mortality rates among all PLWH populations, as well as examining changing trends and the proportion of specific causes of death. Furthermore, it analyzed the factors that influence mortality. Currently, many studies focus on the death situation and influencing factors of PLWH receiving treatment (12-14). However, there are still untreated PLWH in various regions. Analyzing all patients is conducive to a more comprehensive understanding of the actual situation and the effectiveness of interventions. The results of this analysis can help assess the effectiveness of the “Test and Treat” strategy and provide references for improving measures to control AIDS epidemics.
3. Methods
3.1. Data Collection
The data for this study was derived from the China Information System for Disease Prevention Control—AIDS Information System (AIDSIS). Newly identified HIV-infected individuals must be initially registered in AIDSIS. Infected individuals are required to undergo regular follow-ups, with detailed information from each follow-up recorded in AIDSIS. The study subjects included all eligible PLWH obtained from the AIDSIS database. The selection criteria included individuals registered in the system from January 1, 2017, to June 30, 2022, who were aged 15 and above and residing in the Baise City area.
3.2. Study Design
A retrospective cohort study was conducted to collect demographic information, including the results of the first CD4 cell test, history of tuberculosis infection, antiviral treatment, date of death, and cause of death.
3.2.1. Definitions
Years of survival after infection, the observation starting point was the date of HIV diagnosis, and the observation endpoint was either the date of death for deceased individuals or the date of the last follow-up for those lost to follow-up, with the cutoff date being June 30, 2022. The time difference between the observation starting point and the observation endpoint was calculated as the number of years of survival with infection.
AIDS-related deaths is registered in the information system under several categories: AIDS-related tumors (e.g., Kaposi's Sarcoma, Hodgkin's Lymphoma, Invasive Cervical Cancer, Burkitt's Lymphoma, non-Hodgkin's lymphoma), AIDS-related opportunistic infections (e.g., pneumocystis pneumonia, candidiasis, cryptococcosis, toxoplasmic encephalitis, chronic cryptosporidiosis, cytomegalovirus infection, tuberculosis), and AIDS-related specific diseases and syndromes (e.g., HIV-associated dementia, progressive multifocal leukoencephalopathy, wasting syndrome, acute HIV infection syndrome, HIV-associated nephropathy).
Non-AIDS-related deaths, the causes of death registered in the information system include respiratory diseases, cardio-cerebrovascular diseases, digestive diseases, endocrine, nutritional, and metabolic diseases, malignant tumors other than AIDS-related tumors, and other diseases unrelated to AIDS, such as drug overdose, suicide, drug toxicity, and injury.
Unknown causes of death, those whose cause of death was not specified or did not fall within the above categories were classified as having an "unknown cause of death."
Late discoverers, the newly discovered infected individuals with AIDS were those who had progressed to AIDS within 1 year or had a baseline CD4 count of less than 200 cells/μL.
3.3. Statistical Analysis
The data was exported from the China AIDS integrated prevention and control information system and organized using Excel 2022.
The analysis described the characteristics of PLWH monitored by Baise City from 2017 to the first half of 2022, as well as the overall situation of PLWH deaths during this period. This was used to calculate the composition of the causes of death, the proportion of deaths each year (number of deaths from different causes/total number of deaths), and the mortality rate (number of deaths/years of observation).
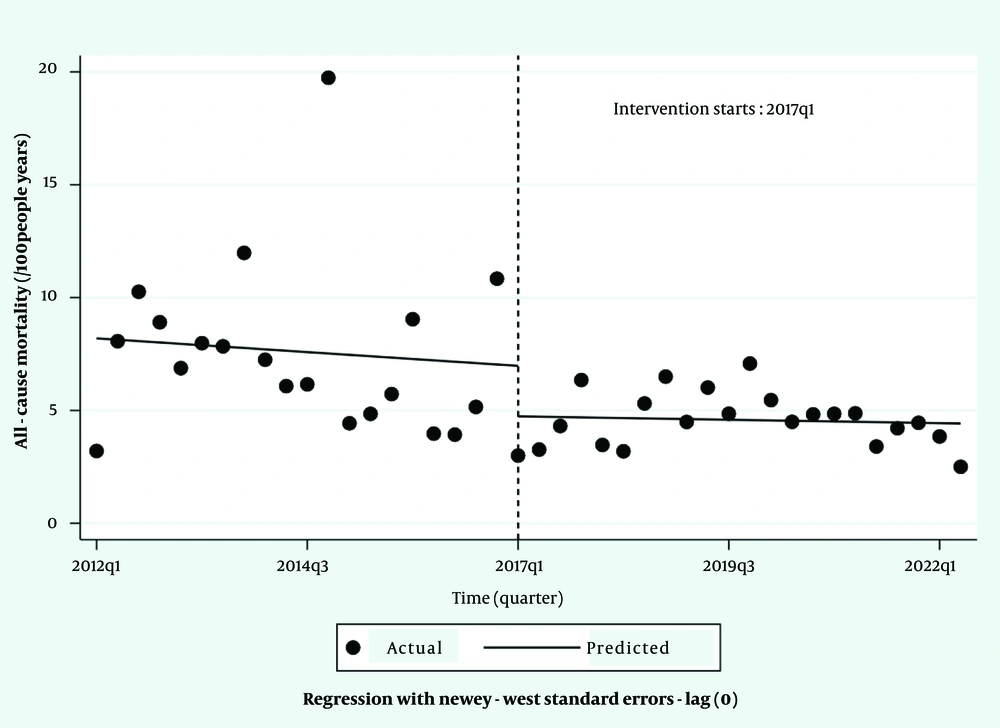
The interrupted time series analysis (ITSA) with a segmented log-linear model was used to analyze the difference in the all-cause mortality rate of PLWH before and after the implementation of the “Test and Treat” strategy. Interrupted time series analysis evaluates the effectiveness of intervention measures by testing the change in slope before and after intervention and the immediate level change at intervention points for outcome variables in time series (15). Quarterly all-cause mortality rates were collected from 2012 to the first half of 2022 and standardized by age and gender composition in 2021. Considering that China began implementing this strategy in June 2016, with some time needed for preparation and adaptation by health departments, the first quarter of 2017 was chosen as the intervention point to avoid lagging effects. This series of statistical processing used STATA 17.0.
We calculated the mortality rate within 1 year after diagnosis for different feature groups, plotted a cumulative risk curve using Kaplan-Meier, and compared the mortality risk within 1 year after diagnosis for different feature groups using the Log-Rank test. Participants’ demographic information, baseline CD4 cell count, history of TB infection, antiviral treatment, and other factors were included in the Cox proportional hazards regression model to explore the factors affecting all-cause mortality and AIDS-related mortality. The time of survival (or follow-up) after the diagnosis was used as the time variable. Univariate analysis was performed first, followed by multivariate analysis, and the adjusted hazard ratio (aHR) of risk factors and its 95% confidence interval (CI) were calculated. The above statistical analysis was performed using SPSS 26.0. A P-value < 0.05 was considered statistically significant.
4. Results
4.1. Characteristics of People Living with HIV
As shown in Table 1, during the observation period, there were 8,922 PLWH cases in Baise City, including 5,623 males (63%) and 3,299 females (37%). The median age of the total PLWH at diagnosis was 43 years (IQR: 11). Over one-third of the population was over 50 years old. Of the PLWH, 94.9% were infected through sexual transmission, 36.6% had a baseline CD4 count of less than 200 cells/µL, 9.8% did not receive antiviral treatment, and 76.4% continued treatment for more than six months.
Among the 1,265 all-cause deaths, the majority were men, predominantly from the peasant and Zhuang ethnic groups. Of all the deaths, 215 (17%) had a history of tuberculosis infection, 638 (50.4%) had a baseline CD4 count of less than 200 cells/µL, and only 149 (11.8%) had a baseline CD4 count of more than 500 cells/µL. Additionally, 476 (37.6%) of the deaths were without ART, and 572 (45.2%) had been treated for more than six months. The median survival time for all-cause mortality was 2.28 years (IQR: 6.40).
There were 438 reported AIDS-related deaths, 76.9% of which were male. The proportion of people under 50 years old and those over 50 years old was nearly equal. PLWH with a baseline CD4 count of less than 200 cells/µL accounted for the largest proportion (69.9%), and only 32 people (7.3%) had a baseline CD4 count of more than 500 cells/µL. Of these deaths, 128 (29.2%) were without ART, and 212 (48.4%) had been treated for more than six months. The median survival time after diagnosis was 1.56 years (IQR: 5.63).
| Variables | Total (N = 8922) | All-Cause Deaths (N = 1265) | AIDS-Related Deaths (N = 438) |
|---|---|---|---|
| Gender | |||
| Male | 5623 (63.0) | 958 (75.7) | 337 (76.9) |
| Female | 3299(37.0) | 307 (24.3) | 101 (23.1) |
| Age of diagnosis (y) | |||
| 15 - 50 | 5777 (64.8) | 629 (49.7) | 208 (47.5) |
| ≥ 50 | 3145 (35.2) | 636 (50.3) | 230 (52.5) |
| Ethnic group | |||
| Han | 1466 (16.4) | 202 (16.0) | 50 (11.4) |
| Zhuang | 7054 (79.1) | 1 012 (80.0) | 372 (84.9) |
| Other minorities | 402 (4.5) | 51 (4.0) | 16 (3.7) |
| Occupation | |||
| Housekeeping/unemployed | 903 (10.1) | 118 (9.3) | 28 (6.4) |
| Peasant | 6252 (70.1) | 897 (70.9) | 341 (77.9) |
| Worker/waitress | 780 (8.7) | 92 (7.3) | 22 (5.0) |
| Other | 987 (11.1) | 158 (12.5) | 47 (10.7) |
| Marital status | |||
| Single | 1710 (19.2) | 221 (17.5) | 78 (17.8) |
| Married | 5670 (63.6) | 775 (61.3) | 271 (61.8) |
| Divorced/widowed | 1474 (16.5) | 248 (19.6) | 87 (19.9) |
| Unknown | 68 (0.8) | 21 (1.6) | 2 (0.5) |
| Education | |||
| Primary school | 4058 (45.5) | 699 (55.3) | 251 (57.3) |
| Junior high school | 3482 (39.0) | 422 (33.4) | 144 (32.9) |
| Highschool | 832 (9.3) | 98 (7.7) | 32 (7.3) |
| College or above | 474 (5.3) | 31 (2.5) | 7 (1.6) |
| Unknown | 76 (0.9) | 15 (1.1) | 4 (0.9) |
| State of infection | |||
| HIV | 4538 (50.9) | 400 (31.6) | 29 (6.6) |
| AIDS | 4384 (49.1) | 865 (68.4) | 409 (93.4) |
| Survival time after the diagnosis(y) | |||
| 0 - 0.99 | 1482 (16.6) | 451 (35.7) | 186 (42.5) |
| 1.00 - 1.99 | 1114 (12.5) | 146 (11.5) | 55 (12.6) |
| 2.00 - 4.99 | 2527 (28.3) | 233 (18.4) | 68 (15.5) |
| 5.00 - 9.99 | 2308 (25.9) | 307 (24.3) | 106 (24.2) |
| 10.00 - 19.99 | 1445 (16.2) | 114 (9.0) | 19 (4.3) |
| More than 20 | 46 (0.5) | 14 (1.1) | 4 (0.9) |
| Infection route | |||
| Injection drug | 365 (4.1) | 109 (8.6) | 16 (3.7) |
| Sexual route | 8469 (94.9) | 1138 (90.0) | 417 (95.2) |
| Other route | 37 (0.4) | 10 (0.8) | 3 (0.7) |
| Unknown | 51 (0.6) | 8 (0.6) | 2 (0.4) |
| History of Tuberculosis b | |||
| No | 8017 (89.9) | 1050 (83.0) | 366 (83.6) |
| Yes | 905 (10.1) | 215 (17.0) | 72 (16.4) |
| Baseline CD4 count (cell/µL) | |||
| < 200 | 3267 (36.6) | 638 (50.4) | 306 (69.9) |
| 200 - 349 | 2572 (28.8) | 260 (20.6) | 57 (13.0) |
| 350 - 500 | 1678 (18.8) | 180 (14.2) | 36 (8.2) |
| > 500 | 1302 (14.6) | 149 (11.8) | 32 (7.3) |
| Not measured | 103 (1.2) | 38 (3.0) | 7 (1.6) |
| ART treatment experience | |||
| Untreated | 865 (9.8) | 476 (37.6) | 128 (29.2) |
| < 3 (months) | 396 (4.4) | 112 (8.9) | 56 (12.8) |
| 3 - 6 (months) | 208 (2.3) | 56 (4.4) | 27 (6.2) |
| > 6 (months) | 6816 (76.4) | 572 (45.2) | 212 (48.4) |
| Unknown or transferred | 637 (7.1) | 49 (3.9) | 15 (3.4) |
Abbreviations: AIDS, acquired immune deficiency syndrome; ART, antiretroviral therapy.
a Values are expressed as No (%).
b Tuberculosis cases refer to those diagnosed based on the national diagnostic standards (16), including both clinical diagnoses and confirmed cases.
4.2. The Overall Mortality
As shown in Table 2, the number of HIV/AIDS infections and deaths in Baise City increased each year from 2017 to 2021. The all-cause mortality rate was 4.19 per 100 person-years, while the AIDS-related mortality rate was 1.45 per 100 person-years, and the non-AIDS-related mortality rate was 2.42 per 100 person-years. AIDS-related mortality accounted for between 30.69% and 47.00% over the years, with an overall proportion of 34.62% (438/1, 265). In contrast, the proportion of non-AIDS-related deaths ranged from 45.00% to 63.49%, with an overall proportion of 57.71% (730/1, 265).
Among all-cause deaths, common chronic diseases such as respiratory system diseases, cardiovascular and cerebrovascular diseases, malignant tumors, and endocrine and nutritional metabolic diseases ranked highest, accounting for 12.41% (157 people), 11.30% (143 people), 8.46% (107 people), and 6.56% (83 people), respectively. These causes collectively accounted for 38.73% (490/1, 265) of all deaths.
Among AIDS-related deaths, the main causes of death were acute AIDS infection syndrome, sporobacterium infection, bacterial pneumonia, tuberculosis infection, AIDS-related tumors, wasting syndrome, and other specific diseases and syndromes related to AIDS, accounting for 10.7% (47 people), 9.8% (43 people), 5.9% (26 people), 4.8% (21 people), 6.2% (27 people), 5.5% (24 people), and 35.2% (154 people), respectively.
| Year | The Number of Infected | Person-Year of Observation | All-Cause Mortality | AIDS-Related Mortality | Non-AIDS-related | Death of Unknown Cause | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mortality Rate | n | Proportion (%) | Mortality Rate | n | Proportion (%) | Mortality Rate | n | Proportion (%) | |||
| 2017 | 4 383 | 3 973.98 | 145 | 3.65 | 54 | 37.24 | 1.36 | 80 | 55.17 | 2.01 | 11 | 7.59 |
| 2018 | 5 041 | 4 525.38 | 189 | 4.18 | 58 | 30.69 | 1.28 | 120 | 63.49 | 2.65 | 11 | 5.82 |
| 2019 | 5 919 | 5 249.07 | 274 | 5.22 | 98 | 35.77 | 1.87 | 149 | 54.38 | 2.84 | 27 | 9.85 |
| 2020 | 6 667 | 5 994.12 | 277 | 4.62 | 79 | 28.52 | 1.32 | 173 | 62.45 | 2.89 | 25 | 9.03 |
| 2021 | 7 537 | 6 809.15 | 280 | 4.11 | 102 | 36.43 | 1.50 | 163 | 58.21 | 2.39 | 15 | 5.36 |
| The first half of 2022 | 7 744 | 3 649.83 | 100 | 2.74 | 47 | 47.00 | 1.29 | 45 | 45.00 | 1.23 | 8 | 8.00 |
| Total | 8 922 | 30 201.53 | 1265 | 4.19 | 438 | 34.62 | 1.45 | 730 | 57.71 | 2.42 | 97 | 7.67 |
a Mortality rate is /100 person-years.
4.3. The Comparison of the Mortality Rate Pre- and Post- the Implementation of the “Test and Treat” Strategy
The all-cause mortality rate (standard rate) from 2012 to the first half of 2022 was compiled. The Mann-Kendall test was conducted to analyze the trend of the time series data, revealing a significant correlation between time variables and mortality (P = 0.001). The data passed the Ljung-Box Q test (P = 0.366) and the Breusch-Godfrey (BG) test (P = 0.376), indicating no autocorrelation in the data. The results of the ITSA are shown in Table 3 and Figure 1, which found no difference in all-cause mortality before and after the intervention (β intervention = -2.235, P intervention = 0.220, β post-intervention = -0.459, P post-intervention = 0.725).
| Variables | Coefficient | 95% CI | t | P-Value |
|---|---|---|---|---|
| Pre-intervention | -0.061 | -0.307 - 0.185 | -0.50 | 0.619 |
| Intervention | -2.508 | -6.245 - 1.229 | -1.36 | 0.182 |
| Post-intervention | 0.065 | -0.205 - 0.335 | 0.49 | 0.629 |
| Constant | 8.192 | 5.619 - 10.765 | 6.45 | < 0.001 |
4.4. All-Cause Mortality Within 1 Year of Diagnosis
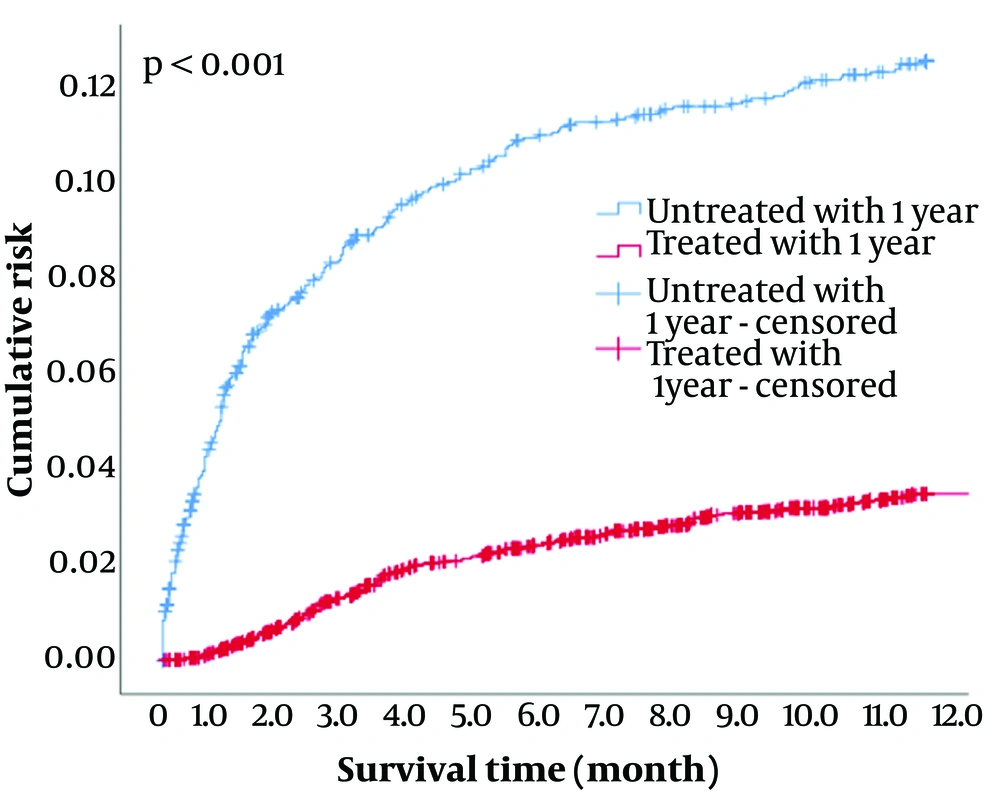
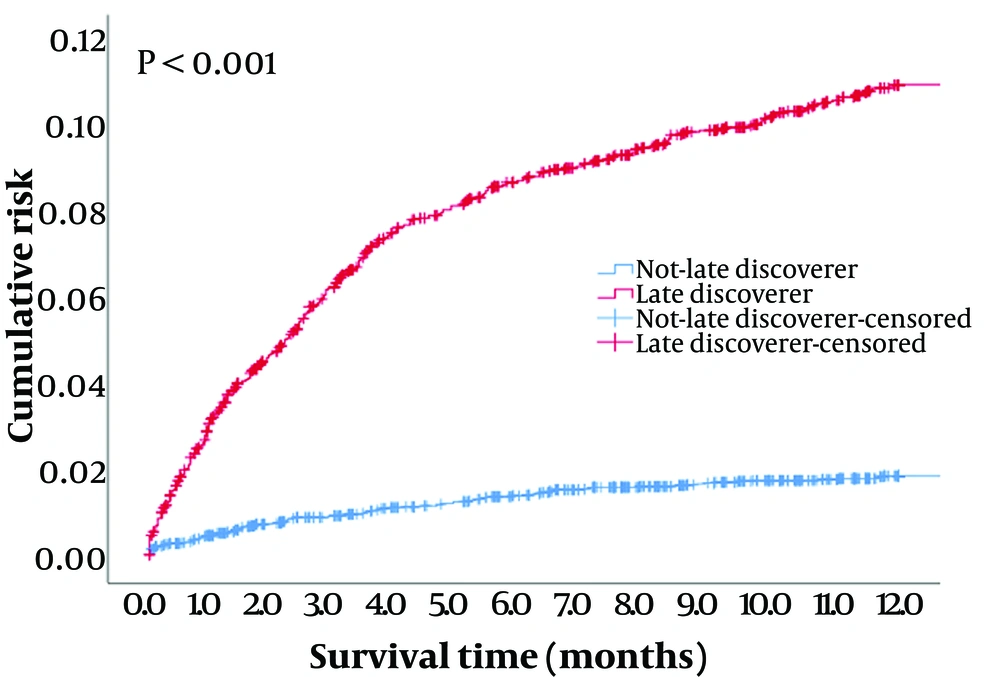
In Table 1, PLWH with a survival time of less than 1 year after diagnosis, i.e., those who died within 1 year after diagnosis, accounted for 35.7% (451 people) of all-cause deaths. The proportion of AIDS-related deaths among all deaths is as high as 42.5%. The all-cause mortality rate for all subjects within 1 year of diagnosis was 5.58/100 person-years (451/8, 113.48). This mortality rate for those who were untreated within 1 year after diagnosis is 13.13/100 person-years (247/1, 881.89), while for those who received treatment within 1 year after diagnosis, this rate is 3.52/100 person-years (198/5, 631.6). The mortality rate for late discoverers and non-late discoverers was 11.63/100 person-years (356/3, 062.33) and 1.88/100 person-years (95/5, 051.15), respectively.
Kaplan-Meier methods were used to establish cumulative death risk curves for PLWH in treated and untreated groups within 1 year after diagnosis. There was a statistically significant difference in the survival curve between treated and untreated patients within 1 year of diagnosis, with untreated patients having a higher risk of death than treated patients (χ2 = 219.174, P < 0.001). The results are shown in Figure 2. By the same method, the cumulative risk of death curves was created for both late and non-late discovery groups of PLWH, with the late discovery PLWH having a higher cumulative risk of death than non-late discovery PLWH (χ2 = 311.338, P < 0.001). The results are shown in Figure 3.
4.5. Influencing Factors of All-Cause Mortality and AIDS-Related Mortality
The characteristic factors in Table 1 were used in the Cox proportional hazards regression model to analyze the influencing factors of all-cause mortality and AIDS-related mortality, respectively. As shown in Table 4, men have a higher risk of death (aHR: 1.85, 95% CI: 1.62 - 2.12) and AIDS-related mortality (aHR: 1.91, 95% CI: 1.51 - 2.41) compared to women. The risk of death for PLWH aged ≥ 50 years was 2.62 times that of those aged 15 - 50 years, and the risk of AIDS-related mortality was 2.08 times that of those aged 15 - 50 years. There was no difference in the overall risk of death between Zhuang and Han PLWH, but the risk of AIDS-related mortality in Zhuang was 1.50 times (aHR:1.50, 95% CI: 1.11 - 2.04) higher than in Han PLWH.
Peasants had a higher risk of all-cause mortality (aHR: 1.32, 95% CI: 1.06 - 1.64) and AIDS-related mortality (aHR: 1.59, 95% CI: 1.04 - 2.44) than housekeeping/housework/unemployed infected persons. The aHR showed that the risk of death and AIDS-related mortality among people with high educational backgrounds was lower. Compared with patients infected through injecting drugs, patients infected through the sexual route had a greater risk of death (aHR: 1.81, 95% CI: 1.41 - 2.34) and specifically AIDS-related mortality (aHR: 3.83, 95% CI: 2.10-7.00).
The overall risk of death for patients with a history of tuberculosis was higher than for those without a history of tuberculosis (aHR: 1.37, 95% CI: 1.18 - 1.60), but there was no difference in the risk of AIDS-related mortality. Compared with patients with a baseline CD4 count < 200 cells/µL, the risk of death and AIDS-related mortality in each group with higher baseline levels was reduced, with patients with CD4 cell counts < 200 having the highest risk.
The study did not find that the risk of all-cause mortality and AIDS-related mortality for PLWH patients treated for < 3 months and < 6 months was different from those without treatment. However, the risk of all-cause mortality and AIDS-related mortality among PLWH undergoing treatment for > 6 months decreased significantly compared to those without treatment, with a reduction of 93% and 92%, respectively.
| Factors | Univariate Analysis of All-Cause Mortality | Multivariate Analysis of All-Cause Mortality a | Univariate Analysis of AIDS-Related Mortality | Multivariate Analysis of AIDS-Related Mortality b | ||||
|---|---|---|---|---|---|---|---|---|
| P | HR | P | aHR (95%CI) | P | HR | P | aHR (95%CI) | |
| Gender c | < 0.001 | 1.95 | < 0.001 | 1.85 (1.62 - 2.12) | < 0.001 | 2.08 | 0.000 | 1.91 (1.51 - 2.41) |
| Age of diagnosis d | < 0.001 | 3.24 | < 0.001 | 2.62 (2.29 - 3.00) | < 0.001 | 3.20 | 0.000 | 2.08 (1.67 - 2.60) |
| Ethnic group | 0.038 | - | 0.011 | - | 0.001 | - | 0.022 | - |
| Han | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 |
| Zhuang | 0.026 | 1.19 | 0.190 | 1.11 (0.95 - 1.30) | < 0.001 | 1.70 | 0.009 | 1.50 (1.11 - 2.04) |
| Other minorities | 0.812 | 0.96 | 0.003 | 1.65 (1.12 - 2.30) | 0.488 | 1.22 | 0.050 | 1.81 (1.00 - 3.26) |
| Occupation | < 0.001 | - | 0.023 | - | < 0.001 | - | 0.051 | - |
| Housekeeping/housework/unemployed | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 |
| Peasant | < 0.001 | 1.83 | 0.014 | 1.32 (1.06 - 1.64) | < 0.001 | 2.66 | 0.033 | 1.59 (1.04 - 2.44) |
| Worker/waitress | 0.821 | 1.03 | 0.345 | 1.15 (0.86 - 1.53) | 0.977 | 0.99 | 0.937 | 1.02 (0.58 - 1.82) |
| Other | 0.005 | 1.41 | 0.715 | 1.05 (0.81 -1.36) | 0.025 | 1.71 | 0.286 | 1.31 (0.80 - 2.17) |
| Marital status | < 0.001 | - | 0.345 | - | 0.001 | - | 0.408 | - |
| Single (never married) | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 |
| Married | 0.033 | 1.18 | 0.551 | 1.05 (0.90 - 1.25) | 0.354 | 1.13 | 0.433 | 0.90 (0.68 - 1.18) |
| Divorced/widowed | < 0.001 | 1.74 | 0.100 | 1.18 (0.97 - 1.45) | 0.002 | 1.63 | 0.863 | 1.03 (0.74 - 1.44) |
| Unknown | 0.479 | 0.85 | 0.975 | 1.01 (0.61 - 1.68) | 0.070 | 0.27 | 0.217 | 0.39 (0.09 - 1.75) |
| Education background | < 0.001 | - | < 0.001 | - | < 0.001 | - | 0.006 | - |
| Literacy, primary school | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 |
| Junior high school education | < 0.001 | 0.56 | < 0.001 | 0.75 (0.66 - 0.85) | < 0.001 | 0.55 | 0.015 | 0.76 (0.61 - 0.95) |
| Highschool/technical secondary school degree | < 0.001 | 0.51 | 0.001 | 0.68 (0.55 - 0.86) | < 0.001 | 0.49 | 0.029 | 0.65 (0.44 - 0.96) |
| College degree or above | < 0.001 | 0.33 | < 0.001 | 0.46 (0.31 - 0.68) | < 0.001 | 0.21 | 0.005 | 0.31 (0.14 - 0.71) |
| Unknown | < 0.001 | 0.26 | 0.003 | 0.37 (0.19 - 0.71) | 0.007 | 0.25 | 0.343 | 0.54 (1.15 - 1.95) |
| State of infection e | < 0.001 | 2.10 | < 0.001 | 1.37 (1.16 - 1.62) | < 0.001 | 14.08 | 0.000 | 9.67 (6.35 - 14.71) |
| Transmission route | 0.004 | - | < 0.001 | - | < 0.001 | - | 0.000 | - |
| Injection drug | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 |
| Sexual route | 0.004 | 1.38 | < 0.001 | 1.81 (1.41 - 2.34) | < 0.001 | 3.24 | 0.000 | 3.83 (2.10 - 7.00) |
| Another route | 0.404 | 1.32 | 0.170 | 1.59 (0.82 - 3.08) | 0.102 | 2.84 | 0.117 | 2.75 (0.78 - 9.78) |
| Unknown | 0.150 | 0.59 | 0.550 | 1.28 (0.57 - 2.90) | 0.890 | 1.11 | 0.173 | 3.30 (0.60 - 18.38) |
| History of tuberculosis f | < 0.001 | 1.60 | < 0.001 | 1.37 (1.18 - 1.60) | < 0.001 | 1.59 | 0.377 | 1.12 (0.87 - 1.45) |
| Baseline CD4 count (cell/µL) | < 0.001 | - | < 0.001 | - | < 0.001 | - | 0.000 | - |
| < 200 | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 |
| 200 - 349 | < 0.001 | 0.42 | < 0.001 | 0.54 (0.45 - 0.64) | < 0.001 | 0.20 | 0.000 | 0.57 (0.42 - 0.78) |
| 350 - 500 | < 0.001 | 0.41 | < 0.001 | 0.38 (0.31 - 0.47) | < 0.001 | 0.18 | 0.000 | 0.38 (0.26 - 0.66) |
| > 500 | < 0.001 | 0.37 | < 0.001 | 0.34 (0.27 - 0.4) | < 0.001 | 0.18 | 0.000 | 0.43 (0.29 - 0.65) |
| Not measured | < 0.001 | 2.38 | 0.952 | 1.01 (0.70 - 1.47) | 0.895 | 0.95 | 0.100 | 2.00 (0.88 - 4.56) |
| ART treatment experience (mon) | < 0.001 | - | < 0.001 | - | < 0.001 | - | 0.000 | - |
| Untreated | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 |
| < 3 | < 0.001 | 1.52 | 0.755 | 0.97 (0.78 - 1.20) | < 0.001 | 2.51 | 0.161 | 1.27 (0.91 - 1.77) |
| 3 - 6 | 0.201 | 1.20 | 0.060 | 0.76 (0.57 - 1.01) | 0.002 | 1.92 | 0.915 | 0.98 (0.64 - 1.50) |
| > 6 | < 0.001 | 0.10 | < 0.001 | 0.07 (0.06 - 0.08) | < 0.001 | 0.14 | 0.000 | 0.08 (0.06 - 0.10) |
| Unknown or transferred | < 0.001 | 0.09 | < 0.001 | 0.07 (0.06 - 0.09) | < 0.001 | 0.10 | 0.000 | 0.07 (0.04 - 0.11) |
a All-cause mortality model: Likelihood ratio test, χ2= 3672.254, P < 0.001, -2 Log Likelihood = 18587.034,C Index = 0.85.
b AIDS-related mortality model: Likelihood ratio test, χ2 = 1515.83, P < 0.001, -2 Log Likelihood = 6259.827, C Index = 0.89. Both models demonstrate good fit.
c Female as the reference group.
d 15 - 50 years old as the reference group.
e HIV as the reference group.
f No history of tuberculosis as the reference group.
5. Discussion
From June 2017 to June 2022, the all-cause mortality rate in Baise was 4.19 per 100 person-years, while AIDS-related mortality was 1.45 per 100 person-years, and non-AIDS-related mortality were 2.42 per 100 person-years. However, national data from the same period showed that the proportion of HIV/AIDS deaths was 4.3% - 4.8%, (17) and the all-cause mortality rate of PLWH in Guizhou province from 2017 to 2018 was 9.09-7.21 per 100 person-years (18). The mortality rate among PLWH in Baise was lower than those in Guizhou province and the national average. The research results did not find a significant change in the all-cause mortality rate of PLWH in Baise City after implementing the “Test and Treat” strategy. These results are similar to the study conducted by Chen et al. in Guangdong, China (19). The implementation of this strategy did not achieve the expected goal of reducing the all-cause mortality rate. This requires the attention of the health sector. The reason may be related to the high proportion of late discovery in this area and the failure to achieve a high proportion of early detection and early treatment. The research findings revealed that among the all-cause mortality and AIDS-related mortality, 50.4% and 69.9% of PLWH respectively had baseline CD4 counts < 200 cells/μL. Additionally, the proportions of AIDS status were found to be 68.4% and 93.4%, respectively. The proportion, effectiveness, and compliance of ART and the demographic characteristics of the local population may have some influence. But these hypotheses need to be explored later.
In recent years, the main causes of death of PLWH in Baise City include non-AIDS-related diseases such as respiratory system, cardiovascular and cerebrovascular diseases, and tumors. The proportion and mortality of non-AIDS-related were higher than those of AIDS-related. Studies have found that (20) in HIV-infected patients, non-HIV-related complications may develop earlier than in the general population of the same age group. HIV infection and its associated immune activation have been identified as an independent risk factor for many non-AIDS-related complications such as common chronic diseases (21). Therefore, for HIV-infected people, we also need to pay attention to the prevention and control of their common chronic diseases. This includes implementing comprehensive care in designated treatment hospitals and jointly diagnosing, treating, and managing multiple disciplines, including infectious diseases, cardiovascular, respiratory, endocrine medicine, and nephrology (21).
This study found that the all-cause mortality rate within 1 year after diagnosis was higher than the overall mortality rate during the observation period. The untreated and late discoverers within 1 year after diagnosis had a mortality rate of more than 10 per 100 person-years, with a higher risk of death. Such patients did not initiate treatment in time or were detected late, leading to rapid disease progression, low immunity, poor body condition, and a high risk of death. Therefore, early testing and treatment of infected people are essential measures to avoid early death after diagnosis. Kityo et al. have reported that the high mortality rate in severely immunocompromised HIV patients shortly after starting ART is related to immune reconstitution inflammatory syndrome (IRIS) that appears with ART (22). Therefore, those initiating ART should be monitored and followed up in the first year, and IRIS should be handled in time.
Our results showed that men had a higher risk of death than women, which is consistent with other studies (13, 23, 24). Some studies have reported that this might be related to the higher incidence of unhealthy behaviors such as smoking, drinking, sexual behavior, and the higher rate of exposure to health-related risk factors (23). Another study from Ethiopia concluded that women can have an early diagnosis of HIV due to better opportunities such as examinations during pregnancy (12), while men may contribute to late HIV diagnosis and poor adherence to ART due to behavioral factors such as substance use (12). A cohort study in China also suggested that poorer ART adherence in men was associated with a higher mortality risk (25). From 1990 to 2016, the AIDS-related mortality rate in men in China increased faster than in women, and the gender gap is gradually widening (26). Therefore, attention should be paid to men, to reduce the exposure to health risk factors and improve treatment compliance.
People living with HIV diagnosed at age > 50 years have a higher risk of death than those aged 15 - 50 years. The proportion of infected people > 50 years old in China increases year by year (17). These individuals are generally older, have a weakened immune system, and belong to a high-risk group for chronic diseases. Therefore, it is crucial to focus on disseminating HIV prevention knowledge and providing treatment support for this population.
Patients with a history of TB had a higher overall risk of death than infected persons without a history of TB. Falvo et al. (27) have suggested that this might be due to the host response to Mycobacterium tuberculosis (MTB), enhancing HIV replication, accelerating the natural progression of HIV, and further suppressing cellular immunity. HIV infection and coinfection with tuberculosis bacilli mutually accelerate disease progression. A study in Guangxi province showed that the risk of death from HIV/MTB coinfection was 1.17 times that of HIV alone and 25.68 times that of MTB alone (28). Antiretroviral therapy and anti-tuberculosis treatment are key interventions to reduce the risk of tuberculosis morbidity and mortality in HIV-positive populations.
Our results demonstrate that the baseline CD4 level of PLWH has an important influence on death, which is consistent with many other studies (13, 29-31). HIV mainly attacks CD4 cells in the human body. When the level of CD4 cells falls below 200 cells/μL, it indicates that the immune function of the infected person is already at a low level. The proportion of baseline CD4 levels below 200 cells/μL in this study was 36.6%, and the late discoverers were high-risk individuals for death. Therefore, to reduce the proportion of late discoverers, it is necessary to strengthen testing procedures and improve the testing rate, which is also the most challenging part of the WHO 90 - 90 - 90 target. Therefore, it is necessary to carry out the testing procedures in various ways, such as expanding community testing service points and independent testing, such as purchasing testing tools online.
This study analyzed the effect of ART duration on the mortality risk of PLWH. The results showed that the risk of all-cause mortality and AIDS-related mortality for PLWH with treatment durations shorter than 3 months and 6 months were not significantly different from those without a treatment history. However, the risk of death for patients with treatment durations longer than 6 months was significantly reduced (aHR all-cause mortality = 0.07, aHR AIDS-related mortality = 0.08).
Most previous studies have analyzed the effect of antiviral treatment on death (30-32), but this study conducted a detailed analysis of the duration of treatment. It found that brief treatment had little impact on improving survival rates, while continuous treatment for more than 6 months significantly improved survival rates. In industrialized countries, HIV/AIDS mortality with successful ART is similar to that of the general population, and mortality among PLWH is comparable to those with diabetes and other chronic diseases (33).
To maximize the benefits of ART, it is necessary to strengthen ART adherence education and management for PLWH, and to select drugs with minimal side effects and simplified treatment regimens. Additionally, timely management of co-infections and maintaining continuous treatment for patients with HIV and other infections are crucial to effectively reduce the death rate.
5.1. Limitations
The data used in this study is from the China AIDS information system (AIDSIS), primarily focusing on the epidemic situation database and the antiviral treatment database. The data includes reports on the epidemic situation and information registered and entered by treatment and follow-up units in 12 counties and districts of Baise City. Although the data has been audited at multiple levels, there are still a few omissions or contradictions, which may impact the quality of the data. However, the data has undergone logical and matching checks, making most of it reliable and complete. Due to incomplete treatment information for PLWH, the analysis of treatment information is not comprehensive enough.
5.2. Conclusions
In recent years, the all-cause mortality rate of PLWH in Baise City was 4.19/100 person-years, while the AIDS-related mortality rate was 1.45/100 person-years, and the non-AIDS-related mortality rate was 2.42/100 person-years. The anticipated changes in PLWH mortality in Baise City after the implementation of the “Test and Treat” strategy have not yet been observed. Among the deceased, the share of non-AIDS-related mortality is higher, and the risk of death within 1 year of diagnosis is higher for untreated PLWH and late discoverers. The health department should enhance PLWH testing, improve treatment adherence, encourage PLWH to continue long-term ART, and provide comprehensive care for the prevention and control of AIDS, tuberculosis, and common chronic diseases among PLWH.