1. Background
The coronavirus (COVID-19) pandemic has caused global uncertainty, according to Wenling et al. (1). During the pandemic period, 6,934,072 fatal cases were reported worldwide (2). The COVID-19 treatment risk group included individuals over 60 years of age, pregnant women, and those with comorbidities (3).
During pregnancy, physiological changes occur in the immune, respiratory, and cardiovascular systems. Additionally, the course of SARS-CoV-2 infection during pregnancy has its own peculiarities (4, 5).
Recent studies indicate an increased risk of spontaneous abortion, spontaneous preterm labor, and severe maternal and neonatal complications caused by COVID-19 (6). Different studies reported an association between pregnancy and an increased risk of admission to intensive care and the need for mechanical ventilation compared to non-pregnant women (7-9).
The meta-analysis we reviewed shows a high incidence of caesarean sections and preterm labor. At the same time, a low breastfeeding rate has been reported, which is not fully explained by the severity of maternal disease or fetal risk (4, 10). Perinatal outcomes with fatal cases have been observed in pregnant women with comorbid pathologies infected with COVID-19. During the pandemic, a positive PCR test for SARS-CoV-2 determined the timing and mode of delivery, rather than maternal and fetal status (4, 10).
2. Objectives
The many unexplored issues and challenges in the perinatal period during the pandemic have prompted further investigation into this topic. The aim of our study is to investigate the impact of COVID-19 infection on perinatal maternal and neonatal outcomes.
3. Methods
The study is historical cohort study, non-interventional, analytical, clinical. We conducted a retrospective analysis of 410 histories of pregnant women admitted to hospitals for 2020 - 2022 years in the City Infectious Disease Centre and the City Infectious Disease Hospital of Shymkent City.
The study participants ranged in age from 18 to 49 years. Women aged 26 to 35 years accounted for 54.4% (223), late reproductive age was 2.4% (10). All participants were PCR assay positive. 293 (71.4%) pregnant women had contact with COVID-19 patients, 28.6% (85) had no contact.
3.1. Inclusion Criteria
Pregnant women with a confirmed case of COVID-19, pregnant women without COVID-19, newborns from mothers with a confirmed case of COVID-19, and newborns from mothers without COVID-19, receiving treatment in hospitals and perinatal centers in 2020 - 2021, regardless of race or nationality.
3.2. Exclusion Criteria
Absence of pregnancy and women of non-reproductive age were excluded from the study. To identify complications in pregnant women with COVID-19, we analyzed the medical histories of pregnant women, dividing them into two groups:
- Main group: Pregnant women with moderate, severe, and extremely severe COVID-19 infection (n = 183).
- Control group: Pregnant women without COVID-19 infection (n = 145).
To determine the perinatal outcomes in women with COVID-19, we analyzed the discharge records of 194 newborns born at the City Perinatal Center in Shymkent according to the following parameters: Weight, height, prematurity, Apgar score, and outcome (discharged home/transferred to the neonatal department).
The subjects were divided into two groups:
- Main group (n = 105): Newborns from mothers with confirmed PCR for SARS-CoV-2.
- Control group (n = 86): Newborns from mothers without COVID-19 infection.
Statistical analysis was performed using IBM SPSS Statistics 26.0 software. Since all data showed non-normal distributions, median confidence intervals and interquartile ranges were used. Categorical variables are presented as absolute numbers, percentages, and frequencies. A P-value of < 0.05 was considered statistically significant. Nominal variables were analyzed using the Mann-Whitney U test, Pearson's chi-square test, and Fisher's exact test.
3.3. Ethics
The research work was approved by the Ethical Committee of JSC "South Kazakhstan Medical Academy" on 21.11.2020, with the conclusion of the ethical committee outlined in protocol No. 1 dated 16.03.2021. All volunteers were included in the study after providing informed consent (11).
4. Results
Among the study population, 12.2% (50) of women were in the first trimester, 29.7% (122) in the second trimester, and 58.1% (238) in the third trimester. Additionally, 18.5% (76) of the women were first-time mothers, while 81.5% (335) were repeat mothers. The predominant age group was 26 to 35 years, comprising 54.4% (223) of the women, followed by the 41 - 50 years age group, which accounted for 2.4% (10) of the pregnant women. The age group of 26 to 30 years was most common in the first and second trimesters, with 36.0% and 28.7%, respectively. Among the women in the third trimester, 30.7% were aged between 31 - 35 years.
Regarding COVID-19 severity, 3.2% (13) had mild symptoms, 40.2% (165) had moderate symptoms, 51.0% (209) were in severe condition, and 5.6% (23) had extremely severe conditions. Analysis of COVID-19 severity by trimester of pregnancy showed statistical significance (P < 0.05).
Table 1 shows that the median birth weights of newborns in the main and control groups were 3220 g and 3330 gr, respectively (P = 0.182). The median birth height was 49 cm in the main group and 52 cm in the control group.
There were 48 (21.0%) babies in the main group and 18 (10.5%) in the control group. Weight above 2500 g was recorded in 79% (182) of newborns in the main group. When comparing the birth weight between the groups, no statistically significant difference was found (P = 0.051). The birth of babies weighing more than 2500 g was 2.26 times more common in the control group than in the main group (95% CI: 0.984 - 5.228). A birth height of less than 48 cm was recorded in 1.7% (3) of cases in the control group and 13.8% (32) of newborns in the main group (P = 0.002). Growth greater than 48 cm was recorded in 86.2% (198) of neonates in the main group and 98.3% (84) in the control group.
When analyzing perinatal outcomes, it was noted that the condition of newborns at birth, as assessed on the Apgar Scale, was 5 - 8 points in the main group and 8 points in 75% of the control group (Table 1) (P < 0.001).
Comparative Characteristics of Weight, Height, Apgar Score of Newborns
Table 2 shows the results of the neonatal maturity assessment. There were 8.2 times more preterm newborns in the main group (91, 39.4%) compared to the control group (10, 5.8%) (P < 0.001). The odds of preterm birth in the control group were 10.5 times higher than in the main group, with the odds difference being statistically significant (95% CI: 3.937 - 28.234).
In the main group, 48.1% (110) of newborns were discharged home in satisfactory condition, while in the control group, 95.3% (164) were discharged in satisfactory condition. In the neonatal pathology department, 51.9% (120) of the main group and 4.7% (8) of the control group were admitted. The odds of being admitted to the neonatal pathology department were 22.1 times lower in the control group compared to the main group. The difference in odds was statistically significant (OR = 0.045; 95% CI: 0.015 - 0.132).
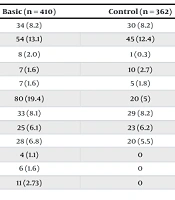
Table 3 shows that antenatal fetal death occurred in 8 cases in the main group and 1 case in the control group (P = 0.04). Preterm labor occurred in 19.4% of women (80) in the main group and 5% (20) in the control group (P = 0.001). A total of 33 (8.1%) cases of cervical rupture were recorded in the main group, and 29 (8.2%) in the control group. In the main group, 6.1% (25) of patients underwent manual separation of the afterbirth, while 6.2% (23) of patients in the control group underwent the same procedure. Labor was complicated by hemorrhage in 28 women (6.8%) in the main group and 20 (5.5%) in the control group. HELLP syndrome was registered in only 4 patients (1.1%) in the main group. DIC (6, 1.6%) and TELA (11, 2.73%) were registered only in the main group. No statistically significant difference was found when comparing the main and control groups (P > 0.05).
| Complication of Pregnancy | Basic (n = 410) | Control (n = 362) | P-Value |
|---|---|---|---|
| Threatening fetal condition | 34 (8.2) | 30 (8.2) | 0.868 |
| Pre-eclampsia | 54 (13.1) | 45 (12.4) | 0.594 |
| Antenatal foetal death | 8 (2.0) | 1 (0.3) | 0.04 b |
| Gestational hypertension | 7 (1.6) | 10 (2.7) | 0.810 |
| UNDAP | 7 (1.6) | 5 (1.8) | 0.112 |
| Preterm labor | 80 (19.4) | 20 (5) | 0.001 b |
| Complication of labor cervical rupture | 33 (8.1) | 29 (8.2) | 0.743 |
| Manual extraction and separation of the afterbirth | 25 (6.1) | 23 (6.2) | 0.374 |
| Bleeding | 28 (6.8) | 20 (5.5) | 0.457 |
| HELPP syndrome | 4 (1.1) | 0 | 0.810 |
| Complication of postpartum period DIC syndrome | 6 (1.6) | 0 | 0.112 |
| TELA | 11 (2.73) | 0 | 0.632 |
Complications of Pregnancy, Labor and Postnatal Period in Women with and Without COVID-19 a
5. Discussion
Women of all age groups participated in our study. The majority of the sample was in the third trimester (238, 58.1%), which is consistent with the literature (12). According to scientists, the severe course of coronavirus infection is more commonly observed in women who have had multiple pregnancies (12). In our sample, 81.5% (335) were repeat mothers, of whom 64% (255) had a severe course. Moore reported that 15% experienced a severe course of infection, 5% had a critical course, and 80% had a mild to moderately severe course, which aligns with the figures reported by the World Health Organization (13). In our study, mild COVID-19 accounted for a smaller proportion of the sample (13, 3.2%), which was associated with receiving treatment at home or in outpatient settings. A total of 51.0% (209) were in severe condition. Consequently, there were more pregnant women with severe COVID-19 in Shymkent city compared to the general population. The later the gestational age or trimester, the more severe the condition.
Recent studies suggest an increased risk of spontaneous abortion, spontaneous preterm labor, and severe maternal and neonatal complications caused by COVID-19 (6). According to Di Toro et al., there is an association between pregnancy and an increased risk of admission to intensive care and the need for mechanical ventilation compared to non-pregnant women (14, 15). Our analysis of the study on perinatal outcomes of newborns revealed that women with COVID-19 are significantly more likely to give birth to low-growth, premature infants with lower Apgar scores, who are subsequently more likely to be admitted to the neonatal pathology department than those born to women without COVID-19 infection.
A large systematic review (28 studies involving 790,954 pregnant women, among whom 15,524 were diagnosed with SARS-CoV-2 infection) aimed to investigate the relationship between SARS-CoV-2 infection during pregnancy and the risk of pre-eclampsia (16). It should also be noted that SARS-CoV-2 during pregnancy increases the likelihood of severe pre-eclampsia and HELLP syndrome (16-21). In our study, preeclampsia (13.1% - 54%) and HELLP syndrome (1.1% - 4%) were more frequent in the main group than in the comparison group.
Additionally, frequent complications of COVID-19 in pregnant women included preterm labor (19.4% - 80%) and antenatal fetal death (2.0% - 8%). The result of the meta-analysis showed that the pooled prevalence of preterm delivery, maternal mortality, NICU admission, and neonatal death in the group with COVID-19 infection was significantly higher than those without COVID-19 infection (P < 0.01). A meta-regression was conducted using the income level of countries (22). Similarly, in our study, neonatal death in COVID-19 pregnant women was more frequent than in the control group.
To analyze, CAS/IMD, remdesivir, and IFN alpha 2b reduced the number of cesarean sections but showed no effect on disease progression or other obstetric and COVID-19 related outcomes (23).
5.1. Limitations
One of the primary limitations of our study is its retrospective nature rather than prospective. These limitations should be taken into account when interpreting the findings of this study. Additionally, the study was monocentric.
5.2. Advantages
The advantage of this study is the relatively large number of patients included.
5.3. Conclusions
Thus, the analysis of perinatal outcomes of newborns revealed that women with COVID-19 coronavirus infection are significantly more likely to give birth to low-growth, premature babies with lower Apgar scores, who are subsequently more likely to be admitted to the neonatal pathology department compared to those born to women without coronavirus infection. The characteristic complications of COVID-19 in pregnant women included preterm labor and antenatal fetal death. Healthcare providers should carefully manage the perinatal period during a COVID-19 outbreak, using the latest information to protect and promote maternal and newborn health. Further research is needed to elucidate the early and long-term effects of the COVID-19 pandemic on maternal and neonatal morbidity and mortality.