1. Introduction
Acute aortic syndromes include a range of severe aortic pathologies and are considered life-threatening conditions (1). Aortic dissections are the most common and lethal among these (1). A specific subtype, acute type A aortic dissection, has a high mortality rate and requires urgent surgical intervention (2). The incidence of acute type A aortic dissections is estimated at 2.5 - 6 per 100,000 patient-years, with the seventh and eighth decades of life being the peak age range for this condition (3). Evidence suggests that age is a significant predictor of aortic dissection, with an increased incidence rate (8.7 per 100,000 patient-years) likely attributed to an aging population (4).
Aortic dissection and pulmonary embolism can rarely present together (5). Pulmonary embolism, the third most common cardiovascular disease after acute coronary syndrome and stroke, is frequently diagnosed in clinical practice (6). Anticoagulation is typically recommended for pulmonary embolism; however, this increases the risk of bleeding in cases of aortic dissection, posing a challenging therapeutic dilemma (6).
The ongoing COVID-19 pandemic has highlighted the complex link between viral respiratory infections and their potential impact on the cardiovascular system (7). The co-occurrence of COVID-19 and cardiovascular complications suggests a significant overlap between viral infection and cardiovascular pathology (8). COVID-19 can affect the myocardium by increasing cardiac biomarkers (9), induce arrhythmias by altering electrical activity in the heart (10), trigger thromboembolic events due to an elevated risk of clot formation (11), and lead to myocarditis as the immune system responds to the infection (12). Additionally, COVID-19 may cause endothelial dysfunction, disrupting normal blood flow and heightening the risk of thrombosis (13). The manifestation of these cardiovascular issues underscores the importance of understanding and managing COVID-19’s effects on cardiovascular health.
This case report presents a rare and complex COVID-19 patient who concurrently developed type A aortic dissection, pulmonary thromboembolism, and deep vein thrombosis. The presence of these three serious conditions in a single patient poses significant challenges in diagnosis, management, and treatment. Optimizing care and patient outcomes requires an understanding of the pathophysiological mechanisms underlying these concurrent complications. This case underscores the necessity for heightened vigilance regarding cardiovascular complications in COVID-19 patients and supports further research into the interplay between viral infections and thromboembolic events.
2. Case Presentation
A 42-year-old man with a past history of opium addiction, abstinent for the past three years, presented to a general hospital in Qom, Iran, on January 24, 2023. Despite a family history of lung disease, the patient had no other identified risk factors or underlying conditions. He arrived at the hospital with complaints of shortness of breath (respiratory rate = 30), severe chest pain (heart rate = 110), and fever. The primary complaint was a severe, stabbing pain in both the anterior and posterior chest, with positional and pleuritic characteristics. The pain, which began three days before admission, was non-radiating, and while it diminished slightly in a fixed position and with shallow breaths, it remained persistent. Fever, chills, and shortness of breath had developed two days prior to admission.
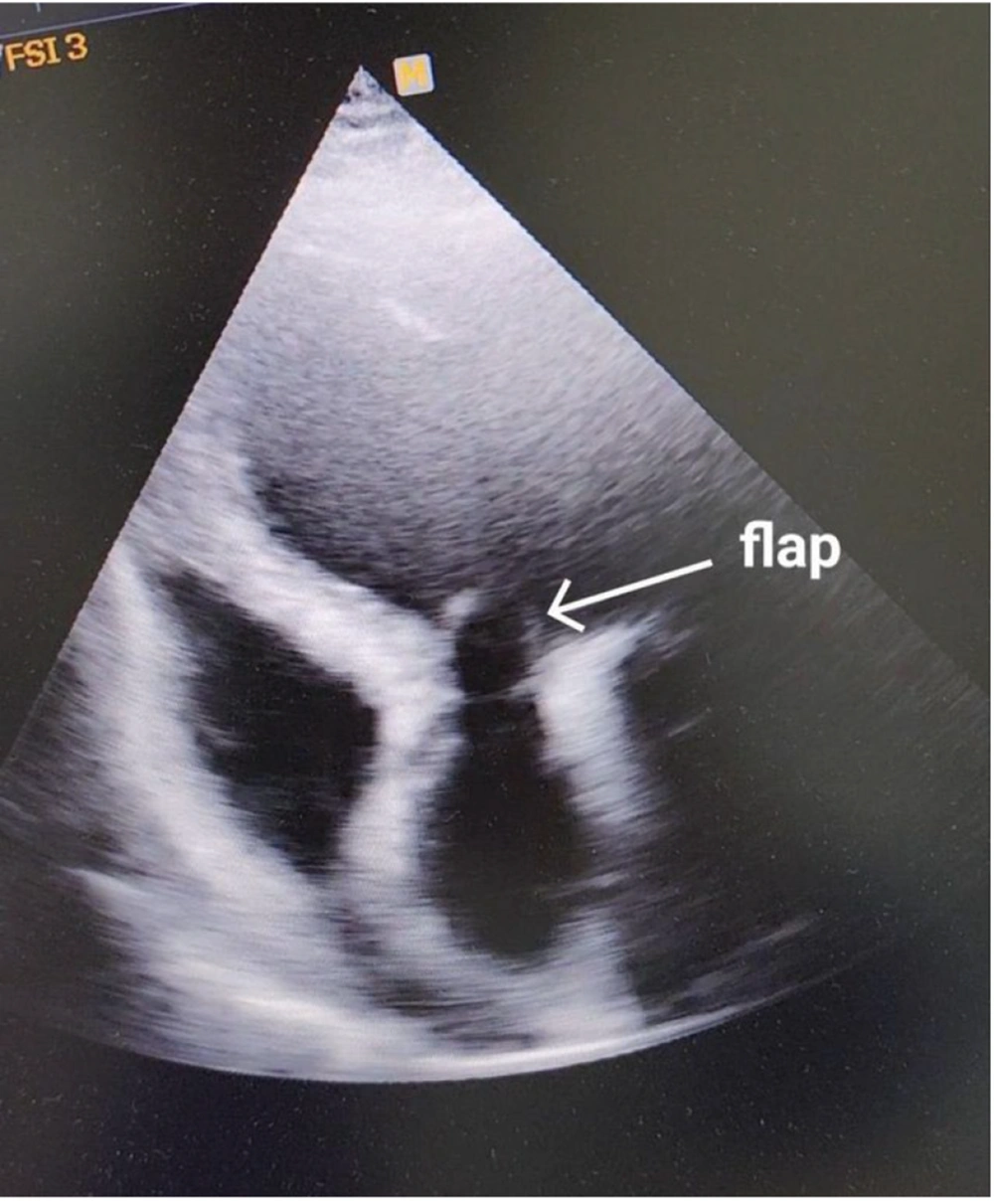
On initial examination, the axillary temperature was 38°C, with sporadic coarse crackles but no discernible heart murmur. No discrepancies were noted in systolic pressure or pulse between the left (135/85 mmHg) and right (140/90 mmHg) arms and legs. A transthoracic echocardiogram was promptly performed. The echocardiogram revealed severe left ventricular (LV) enlargement (LVEDVI = 105 mL/m²), mild LV systolic dysfunction (EF = 45%), and a normal right ventricular (RV) size with moderate dysfunction (TAPSE = 12 mm). The aortic valve was significantly damaged, leading to mild aortic stenosis (PPG = 16 mmHg) and moderate aortic insufficiency, along with mild mitral and tricuspid regurgitation. There was no pericardial effusion, and the ascending aorta was dilated to 60 mm. Additionally, a suspicious density was observed moving into the left ventricle from the aorta during diastole and returning to the aorta during systole (Figure 1).
The patient was admitted to the CCU with two possible diagnoses under consideration: Acute aortic dissection and aortic valve endocarditis.
Tests were conducted for WBC, RBC, hemoglobin, platelets, PTT, INR, blood sugar, blood urea, creatinine, sodium, potassium, troponin, D-dimer, CRP, S.G.O.T. (AST), S.G.P.T. (ALT), and alkaline phosphatase. Elevated D-dimer levels (3847 ng/mL) suggested the presence of an acute aortic dissection and pulmonary thromboembolism. Additional tests indicated elevated urea, creatinine, platelet count, and troponin.
A spiral chest CT without contrast revealed generalized bilateral ground-glass opacities, indicative of COVID-19 infection. After 12 hours of hospitalization, the patient underwent CT angiography of the aorta and pulmonary arteries, as well as an ultrasound of the legs. CT angiography revealed a type A aortic dissection extending from the origin of the aorta to the midpoint of the arch. Additionally, bilateral segmental pulmonary artery thromboembolism was identified (Figure 2).
Both pulmonary thromboembolism and deep vein thrombosis were confirmed. Ultrasound of the leg veins, including the common and external iliac veins, the common and deep femoral veins, the saphenofemoral junction (SFJ) vein, and the peroneal vein, showed increased flow rates in these veins. The superficial femoral, popliteal, and posterior tibial veins demonstrated an increased diameter with echogenic and heterogeneous thrombus in the lumen, which did not compress upon examination.
Due to the aortic dissection and the associated risk of further spread, heparin could not be administered to treat the pulmonary thromboembolism. The patient underwent emergency surgery for a Bentall procedure to replace the aortic valve and repair the aortic dissection. Thirty-six hours after admission, the patient was transferred to Tehran Imam Hospital for surgery. Unfortunately, the patient suffered respiratory and cardiac arrest post-surgery, with bradycardia and arrest occurring two hours after resuscitation attempts.
3. Discussion
In the present study, we described a 42-year-old man with COVID-19, complicated by type A aortic dissection, pulmonary thromboembolism, and bilateral deep vein thrombosis. This case illustrates the severe cardiovascular complications that can arise in COVID-19 patients. The patient presented with overlapping life-threatening conditions, including type A aortic dissection, pulmonary thromboembolism, and COVID-19 pneumonia, each requiring immediate intervention yet posing complex treatment challenges.
The aortic dissection demanded urgent bentall surgery due to the high risk of rupture and mortality. However, anticoagulation therapy for the pulmonary thromboembolism could have exacerbated the dissection, creating a treatment dilemma: Addressing the thromboembolism might worsen the dissection, while failing to do so could lead to fatal hypoxia or circulatory collapse. COVID-19 pneumonia further compromised pulmonary function, heightening the risks of hypoxemia and hypercoagulability, both of which could exacerbate thromboembolic events. COVID-19 likely contributed to vascular inflammation in both the arterial and venous systems, potentially precipitating the rare concurrent presentation of type A aortic dissection and pulmonary thromboembolism (14).
Similar cases have been reported in the literature. Chong et al. documented a case of a 74-year-old male with acute type A aortic dissection and saddle pulmonary embolism, who unfortunately passed away during surgery (5). Rampon et al. also reported a case involving acute type A dissection and pulmonary embolectomy in a 75-year-old male patient. This patient was successfully discharged on postoperative day 10 with a lifelong prescription for warfarin (15).
Tabaghi and Akbarzadeh in Lorestan, Iran, reported a case of a 47-year-old woman with acute type A aortic dissection who had COVID-19; unfortunately, the patient died before reaching the operating room (16). Similarly, a case study in Michigan described a 52-year-old man with acute type A aortic dissection and a positive COVID-19 PCR result, who also succumbed to the condition (17). In Turkey, Akgul et al. presented a case involving a 68-year-old woman with type A aortic dissection and COVID-19; she was successfully discharged 14 days after undergoing cardiopulmonary bypass (18). Another case in Tehran, Iran, documented the death of a 62-year-old woman due to COVID-19-related aortic dissection rupture and tamponade (19). Additionally, Volvovitch et al. reported a 73-year-old patient with acute type A aortic dissection and acute pulmonary embolism affecting both the right and left pulmonary arteries. She tested positive for COVID-19 and underwent successful surgery, including bilateral pulmonary embolectomy and aortic dissection repair, and was discharged without complications on the ninth postoperative day (20).
Most of these cases reported type A aortic dissection in the context of COVID-19, yet the present study highlights an even more complex scenario. This case involved the simultaneous presence of pulmonary thromboembolism, type A aortic dissection, and deep vein thrombosis in a COVID-19 patient, significantly complicating treatment decisions.
The patient faced multiple overlapping life-threatening conditions: Type A aortic dissection, pulmonary thromboembolism, and COVID-19 pneumonia, each requiring urgent intervention but presenting complex challenges for care. Due to the high risk of rupture and mortality, the aortic dissection demanded immediate bentall surgery (21). However, anticoagulation therapy for the pulmonary thromboembolism could worsen the dissection. This presented a therapeutic dilemma: Treating the thromboembolism risked exacerbating the dissection, while withholding treatment risked deadly hypoxia or circulatory collapse. Additionally, COVID-19 pneumonia compromised pulmonary function, increasing the likelihood of hypoxemia and hypercoagulability, which could have further escalated thromboembolic complications.
The patient with COVID-19 presented an extraordinary and complex case of concomitant type A aortic dissection, pulmonary thromboembolism, and deep vein thrombosis. This highlights the critical need for heightened clinical awareness and rapid inter-specialty collaboration to manage these life-threatening conditions effectively. Additionally, it underscores the importance of exploring the pathophysiological connections between COVID-19 and severe vascular diseases to advance targeted pharmacotherapy. Prompt recognition and intervention in such cases are essential for optimizing patient outcomes, emphasizing that rapid assessment and management are paramount in similar clinical settings.