1. Background
COVID-19 has affected approximately 515 million people globally resulting in nearly 6 million deaths according to recent data (1). Although children's underdeveloped immune systems were initially expected to result in higher infection rates (2), the incidence of COVID-19 remains comparatively low in this age group, with only about 1% of confirmed or suspected cases reported in children under ten years old (3-5).
Among pediatric patients neonates are particularly susceptible to COVID-19, often presenting with atypical and subtle symptoms (5-7). Studies suggest that infants under 30 days old are more likely to experience severe symptoms, increasing their risk for intensive care unit (ICU) admission (2). Although COVID-19 presentations in neonates can range from asymptomatic to respiratory distress, mild nonspecific symptoms like poor feeding and diarrhea are more common (3, 8). These mild cases are frequently misdiagnosed or undetected (3), potentially contributing to viral transmission through asymptomatic or mildly symptomatic neonates. Consequently, thorough evaluation and exclusion of COVID-19 in neonates with ambiguous symptoms are essential.
Neonatal sepsis is another condition characterized by nonspecific clinical features (9) and is a significant cause of morbidity and mortality in infants under 28 days old (10). Commonly presenting with symptoms such as poor feeding and lethargy. Respiratory symptoms are also common in sepsis, often associated with pneumonia (10) leading to a clinical overlap with COVID-19 presentations in neonates.
While COVID-19 can precipitate sepsis, most sepsis cases in neonates are due to bacteremia (11) which may necessitate different bedside management strategies. Therefore, COVID-19 testing is crucial for any neonate with suspected sepsis or with clinical or paraclinical findings lacking an identifiable cause (9). There is a pressing need for evidence to support a more precise, timely, and differential diagnosis of COVID-19 in neonates. This study aims to identify and compare the clinical and paraclinical manifestations of COVID-19 and sepsis in neonates with confirmed diagnoses.
Despite significant advancements in COVID-19 research within adult and pediatric populations, neonates remain underrepresented in the current literature. Given the overlapping clinical presentations of COVID-19 and sepsis in neonates, distinguishing between these conditions is critical for accurate diagnosis and effective treatment.
2. Objectives
This study addresses this gap by providing a comparative analysis focused explicitly on neonates, offering insights that can aid in clinical differentiation. Understanding these distinctions is essential for guiding management decisions and supporting healthcare providers in tailoring interventions for this vulnerable population.
3. Methods
3.1. Study Setting and Sampling
This prospective observational study was conducted in the Department of Pediatrics at Namazi and Hafez hospitals from February 20, 2020, to December 20, 2020. Written informed consent was obtained from parents or guardians before enrollment, along with detailed written and verbal information, regarding potential risks and benefits. Parents received a research fact sheet that emphasizing voluntary participation, assuring them that there were no penalties for nonparticipation, and informing them of their right to withdraw their infant from the study at any time without providing a reason. Confidentiality of all participant data was strictly maintained.
During the study period, neonates admitted with respiratory problems or presenting with symptoms such as poor feeding, lethargy, restlessness, and diminished reflexes underwent comprehensive screening, including complete blood count (CBC), C-reactive protein (CRP), blood culture, and COVID-19 polymerase chain reaction (PCR) testing. Complete blood count and CRP results were obtained promptly, COVID-19 PCR results were available within 24 hours, and blood culture results were available within 72 to 120 hours. Sepsis patients were defined as those with confirmed sepsis based on positive blood culture results, while COVID-19 cases were confirmed via PCR testing. Neonates with a confirmed diagnosis of either sepsis or COVID-19 were categorized into two groups: The sepsis group and the COVID-19 group.
Inclusion criteria included an age of less than 28 days and a confirmed diagnosis of COVID-19 by PCR or sepsis by a positive blood culture. Exclusion criteria were incomplete data and the absence of a confirmed diagnosis of either COVID-19 or sepsis.
3.2. Clinical and Paraclinical Data Collection
Data were extracted from hospital records and included various clinical and laboratory indicators. Observed clinical indicators encompassed signs and symptoms such as poor feeding (defined as lack of interest or ability to feed and feeding less than usual) and lethargy or restlessness (drowsiness, sleepiness, poor response to stimuli, irritability, or excessive crying). Laboratory findings included blood culture, urine culture, cerebrospinal fluid (CSF) analysis, CBC, and CRP. Radiological assessments were performed to identify any signs of pulmonary involvement. The outcome of each case, specifically mortality or discharge, was recorded.
3.3. Data and Statistical Analysis
All data were recorded and analyzed using statistical package for the social sciences (SPSS) version 23 for Windows. Categorical variables were compared using the chi-square test or Fisher’s exact test, as appropriate. For continuous variables, Student’s t-test was used for normally distributed data, and the Wilcoxon signed-rank test was applied to data with a skewed distribution. A P-value of < 0.05 was considered statistically significant.
4. Results
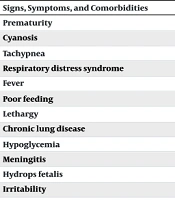
In this prospective observational study, 48 neonates meeting the inclusion criteria were enrolled, with no exclusions due to complete data availability. Each group included 24 neonates. Poor feeding and lethargy were significantly more frequent in neonates with sepsis than in those with COVID-19 (P = 0.01 and P = 0.03, respectively). Specifically, poor feeding was observed in 13 (54.16%) sepsis cases versus 5 (20.83%) COVID-19 cases, and lethargy was present in 8 (33.33%) sepsis cases versus 2 (8.33%) COVID-19 cases (Table 1).
| Signs, Symptoms, and Comorbidities | COVID-19 Group 24 | Sepsis Group 24 | P-Value |
|---|---|---|---|
| Prematurity | 6 (25) | 7 (29.16) | 0.74 |
| Cyanosis | 4 (16.67) | 1 (4.16) | 0.15 |
| Tachypnea | 4 (16.67) | 1 (4.16) | 0.15 |
| Respiratory distress syndrome | 3 (12.5) | 0 | |
| Fever | 5 (20.83) | 7 (29.16) | 0.50 |
| Poor feeding | 5 (20.83) | 13 (54.16) | 0.01 |
| Lethargy | 2 (8.33) | 8 (33.33) | 0.03 |
| Chronic lung disease | 2 (8.33) | 0 | - |
| Hypoglycemia | 1 (4.16) | 0 | - |
| Meningitis | 1 (4.16) | 0 | - |
| Hydrops fetalis | 1 (4.16) | 0 | - |
| Irritability | 1 (4.16) | 1 (4.16) | 1 |
Comparison of Various Signs, Symptoms, and Comorbidities Among COVID-19 and Sepsis Patients a
In the COVID-19 group, two patients developed sepsis during hospitalization, as confirmed by positive blood cultures. In contrast, all neonates in the sepsis group had positive blood cultures, with late-onset sepsis (> 72 hours of age) being predominant. Early-onset sepsis (< 72 hours of life) was identified in four cases within the sepsis group but not in the COVID-19 group. Klebsiella pneumoniae was isolated in COVID-19 patients who developed secondary sepsis. In contrast, the sepsis group exhibited a variety of organisms, including Acinetobacter, Alpha-hemolytic Streptococcus, Escherichia coli, Enterobacter, Enterococcus, K.pneumoniae, methicillin-resistant coagulase-negative staphylococci, non-fermentative bacilli, Pseudomonas, Serratia, Staphylococcusepidermidis, Streptococcus, and vancomycin-resistant Enterococcus.
All urine cultures in the COVID-19 group were sterile, while in the sepsis group, 4 (16.6%) urine cultures yielded growth of E. coli, Enterococcus, and yeast (P = 0.29). Cerebrospinal fluid analysis showed no significant difference between the groups (COVID-19: 72.73% vs. sepsis: 83.3%; P = 0.46).
Neonates with sepsis had significantly lower platelet counts (COVID-19: 296.73 ± 160.15 × 10³/mm³ vs. sepsis: 199.08 ± 184.61 × 10³/mm³; P = 0.03) and higher CRP levels (COVID-19: 29.14 ± 52.72 mg/dL vs. sepsis: 96.83 ± 53.55 mg/dL; P < 0.001) compared to COVID-19 neonates. There were no significant differences between the groups in total white blood cell count (COVID-19: 10.19 ± 4.26 × 10³/mm³ vs. sepsis: 13.48 ± 8.94 × 10³/mm³; P = 0.33), neutrophil percentage (COVID-19: 42.25 ± 19.20% vs. sepsis: 49.54 ± 20.27%; P = 0.42), lymphocyte percentage (COVID-19: 47.18 ± 19.20% vs. sepsis: 42.15 ± 19.10%; P = 0.46), and hemoglobin levels (COVID-19: 12.81 ± 2.66 mg/dL vs. sepsis: 12.32 ± 2.91 mg/dL; P = 0.56).
Although chest X-rays indicated higher pulmonary involvement among COVID-19 neonates [16/22 (72.7%)] compared to sepsis neonates [13/23 (56.5%)], this difference was not statistically significant (P = 0.35).
Neonatal mortality was higher in the COVID-19 group compared to the sepsis group, though this difference did not reach statistical significance (COVID-19: 6 (25%) vs. sepsis: 1 (4.2%); P = 0.09).
5. Discussion
This study enrolled neonates diagnosed with either COVID-19 or sepsis, all of whom required hospital admission. Several distinctions between COVID-19 and sepsis in neonates were identified. Notably, poor feeding and lethargy were significantly more prevalent among neonates with sepsis, whereas conditions such as respiratory distress syndrome, chronic lung disease, and hypoglycemia were observed exclusively in COVID-19 cases. The CSF analysis mainly yielded normal results in both groups. Additional differences included lower platelet counts and higher CRP levels in sepsis patients. Both groups demonstrated comparable pulmonary involvement in radiological findings, while mortality was significantly higher in COVID-19 cases.
In alignment with other studies, COVID-19 symptoms in neonates, such as fever, poor feeding, and tachypnea, tend to be milder (8, 12, 13). Several hypotheses have been proposed to explain this age-related pattern of COVID-19 infection. One hypothesis suggests that the immature angiotensin-converting enzyme 2 (ACE2) receptor, integral to SARS-CoV-2 pathogenesis, binds less effectively to the virus in neonates than in adults (4). Another hypothesis posits that, despite their underdeveloped immune systems, neonates may have higher relative counts of lymphocytes and natural killer cells, both critical in combating COVID-19 (14). However, this does not explain why other respiratory viruses, such as respiratory syncytial virus (RSV) and influenza, often cause more severe diseases in the pediatric population (15). This discrepancy underscores the need for further investigation into the role of the immune system in COVID-19 pathogenesis, including the possibility of a mitigated cytokine storm in children due to less pronounced pro-inflammatory cytokine responses (14, 16-18). This discrepancy underscores the need for further investigation into the role of the immune system in COVID-19 pathogenesis, including the possibility of a mitigated cytokine storm in children due to less pronounced pro-inflammatory cytokine responses (19). Another theory suggests that high viral and bacterial colonization in children may compete with SARS-CoV-2, limiting its colonization and reducing its pathogenesis (20, 21). In summary, the relatively mild COVID-19 symptoms in neonates may result from a combination of immature ACE2 receptor binding, distinct immune responses, lower prevalence of comorbidities, and microbial competition.
Differentiating COVID-19 from sepsis in neonates is essential yet challenging due to similar nonspecific clinical features (22). Asymptomatic COVID-19 neonates can still transmit the virus due to high viral loads (6, 23), underscoring the need for differentiation as treatment approaches differ significantly. Once confirmed by reverse transcription-polymerase chain reaction (RT-PCR) testing, COVID-19 cases require isolation and management based on symptom severity (24), whereas sepsis is diagnosed via blood culture and managed with antibiotics tailored to local bacterial flora (25). Accurate and timely diagnosis is therefore crucial for optimal management of both conditions.
Laboratory findings in neonates with COVID-19 remain variable and sometimes controversial (26, 27). Although our study found slightly elevated white blood cell (WBC) counts in COVID-19 patients, other studies report average counts as well (28). Variations in CRP and platelet counts have also been noted across studies (29). In sepsis, laboratory findings may include leukocytosis or leukopenia and elevated CRP levels (30), reflecting disease progression and severity (31). Furthermore, the accuracy of diagnostic tests for neonates remains a concern, as standard normal ranges for laboratory values may not be well established for this population (32).
Pulmonary involvement and respiratory symptoms can appear in both COVID-19 and sepsis (10, 33), making radiological findings of limited use in distinguishing between the two conditions based on this study’s observations. However, the significantly higher mortality rate observed in COVID-19 neonates highlights the need for early testing in cases presenting with nonspecific symptoms, abnormal laboratory findings, exposure history, or suspicious radiological findings, to prevent missed diagnoses (34).
This study provides valuable insights into the clinical distinctions between COVID-19 and sepsis in neonates, highlighting unique patterns in symptoms, laboratory findings, and outcomes. A significant strength of this study is its focus on directly comparing these two challenging conditions within a neonatal population, offering critical information that may assist clinicians in differential diagnosis and management. Despite the relatively small sample size, the findings remain statistically significant, underscoring the robustness of the observed differences. This suggests that even a modest sample can yield meaningful insights when carefully analyzed, as in this investigation. However, due to the limited sample size, the generalizability of the findings may be constrained, as a larger cohort could provide a more comprehensive understanding of the clinical characteristics of these conditions across diverse settings. Future research should consider multicenter, large-scale studies to validate these findings further and expand on the nuances of COVID-19 and sepsis in neonates.
5.1. Conclusions
In conclusion, this study highlights the clinical distinctions and challenges in differentiating COVID-19 from sepsis in neonates, emphasizing the importance of tailored diagnostic and management strategies. Although the findings provide valuable insights into mortality risks and immune responses, more extensive multicenter studies are essential to strengthen the evidence and guide best practices for managing these conditions in neonatal populations. The study underscores the need for early testing and differentiation between COVID-19 and sepsis, particularly when symptoms overlap. These insights can help clinicians recognize subtle but significant differences in clinical and paraclinical presentations, facilitating timely intervention and management. Given the complexity and ambiguity of neonatal presentations, this study serves as a valuable reference for enhancing diagnostic accuracy and improving outcomes in neonatal care.