1. Background
In 2020, the COVID-19 pandemic had a widespread impact and presented unprecedented challenges for many business sectors, becoming the primary cause of absenteeism and failure to return to previous jobs across various occupations. Many factors can contribute to extended absences from work and delays in returning to work (RTW) after this illness (1).
According to the latest recommendations from the Centers for Disease Control and Prevention (CDC), the duration of sickness absence after COVID-19 was at least 10 days and up to 20 days after the onset of symptoms, depending on the severity of the disease (2).
A prospective cohort study showed that 30% of individuals who recovered from COVID-19 reported long-term symptoms and reduced health-related quality of life (3). A decrease in physical fitness and performance levels can persist for up to two years after infection (4). Certain co-morbidities and risk factors, such as age, obesity, high blood pressure, and diabetes, may increase the risk of more severe disease (5).
Fraser and Gaspar found that the duration of absenteeism was higher among the elderly, with the fear of contracting COVID-19 being the most common reason for absence from work, followed by other factors such as the infection itself (6). Preventive measures at both the individual and systemic levels, including hand hygiene, workplace hygiene, and wearing a mask, were associated with significant improvements in psychological symptoms such as stress, anxiety, fear, and insomnia after RTW (7).
Leggat-Barr et al. found that the Standard Mortality Ratio (SMR) in Native Americans was highly correlated with frontline workers’ status, as most of these workers came from deprived populations and were employed in jobs that involved close contact with others, often without appropriate protective measures or the possibility of remote work. These jobs were typically low-paying and required face-to-face interaction with others (8). Another study showed that the death rate due to the coronavirus was highest among taxi drivers. However, after adjusting for other confounding factors, the researchers concluded that working in frontline infectious disease jobs did not lead to an increase in deaths caused by COVID-19 (9). In a cohort study in Australia, up to one-third of COVID-19 survivors did not return to their previous job due to a new disability (10).
2. Objectives
We could not find a study on the factors affecting RTW for people affected by COVID-19 in Iran. Therefore, this study was conducted to assess the factors affecting RTW in employees after being infected by COVID-19 in Iran.
3. Methods
This was a cross-sectional study conducted on individuals aged 20 to 60 years who were admitted to hospitals in Yazd province, Iran, with a definite or probable diagnosis of COVID-19 from September 2020 to March 2021. In this study, individuals with a positive result for Polymerase Chain Reaction (PCR) testing for COVID-19 were considered as definite cases. Those with at least one of the following conditions were considered as probable cases: 1) Radiological manifestations strongly suggestive of COVID-19, including one- or two-sided multi-lobular infiltration or ground-glass lesions on a CT scan; 2) pneumonia with an inappropriate clinical response to usual treatments and rapid deterioration of the patient's clinical condition.
Initially, patient information was extracted from the database of the health deputy of the medical university. A total of 1,040 individuals were identified. Individuals who were simultaneously hospitalized or on sick leave due to other reasons were excluded from the study. Data were collected via a questionnaire through a phone interview by census. The interviews were conducted by two occupational medicine specialists, who were trained in a session. The Kappa coefficient between the specialists was 0.8. Among the 1,040 individuals, 355 agreed to participate in the study and answered the questions (response rate: 34%). Of the responders, 33 did not meet the inclusion criteria, and ultimately, 320 individuals were assessed.
The questionnaire consisted of four parts: The first part collected demographic information, including age, marital status, weight, height, and educational qualification. The second part focused on job information, including:
- Employment status, job title, and work experience
- Type of respiratory exposure (dusts, metal fumes, solvents, acids and alkalis, and pesticides)
- Intensity of exposure based on the occupational history reported by the patient and the opinion of the occupational medicine specialist (very low, low, moderate, and high)
- Intensity of physical activity at work (sedentary, light, medium, heavy, and very heavy)
- Type of shift work (fixed morning, fixed evening, fixed night, rotating day and night, and split)
The intensity of physical activity at work was categorized as follows: Sedentary (energy requirement less than 2 Met); light (energy requirement: 2 - 3 Met); moderate (energy requirement: 4 - 5 Met); heavy (energy requirement: 6 - 8 Met); and very heavy (energy requirement more than 8 Met) (11).
The third part of the questionnaire included information about the recent COVID-19 infection, such as disease manifestations, type of treatment, number of days spent in the hospital, use of medicine at home, and the individual’s underlying disease status.
The final part of the questionnaire was dedicated to information about RTW, including the duration of medical absenteeism, the reason for the absence, work-related mitigations taken in the workplace after the pandemic [e.g., physical distancing, personal protective equipment (PPE) use, and hygienic measures such as hand washing], exacerbation of symptoms due to occupational exposures, and physical activities in the workplace.
Two methods were used to classify jobs:
1. The standard classification of occupations in Iran (based on the International Standard Classification of Occupations, 2008), which divides occupations into 10 groups: "Managers, professionals, technicians and associate professionals, clerical support workers, service and sales workers, skilled agricultural, forestry and fishery workers, crafts-related trades workers, plant and machine operators and assemblers, elementary occupations, and armed forces occupations" (12).
2. In the second method, physical, biological, and chemical exposures were used to classify jobs into the following categories: Salesperson, office workers/teachers/guards, drivers, healthcare workers, industry and construction workers, farmers and ranchers, military workers, and food handlers.
Participants were also divided into two groups based on the duration of absenteeism: Fewer than 21 days and 21 days or longer. According to the RTW guidelines after COVID-19 in our country, a 21-day interval before RTW was accepted as the standard. Thus, a duration longer than 21 days was considered delayed RTW. We did not assess the sustainability of RTW.
Data were analyzed using SPSS (ver. 25) with the Kolmogorov-Smirnov test, Kruskal-Wallis test, Mann-Whitney U test, chi-square test, Spearman's correlation test, and univariate and multivariate logistic regression.
The study was approved by the ethics committee of Shahid Sadoughi University of Medical Sciences (Ethics code: IR.SSU.REC.1399.265).
4. Results
Among the 320 employees participating in the study, 295 were men (92%) and 25 were women (8%). Additionally, 92% of the participants were married. Among all participants, 3% were illiterate. The educational levels of the others were as follows: Twenty-three percent had less than a high school diploma, 28% were high school graduates, and 10%, 24%, 8%, and 3% held associate, bachelor’s, master’s, and doctorate degrees, respectively. Table 1 shows the demographic information and the characteristics of the participants' jobs. The mean work hours per week and per day were 49.55 ± 12.54 hours and 8.88 ± 4.17 hours, respectively.
| Variables | Values |
|---|---|
| Age (y) | 39.77 ± 8.36 (40) |
| Number of dependents | 2.61 ± 1.40 (3) |
| BMI (kg/m2) | 28.14 ± 5.01 (27.68) |
| Work experience (y) | 15.82 ± 9.06 (15) |
| Employment status | |
| Official | 45 (14.1) |
| Temporary contract | 22 (6.9) |
| Permanent contract | 97 (30.3) |
| Self-employed | 142 (44.4) |
| Others | 14 (4.4) |
| Work shift | |
| Fixed morning | 184 (57.5) |
| Cycling | 60 (18.7) |
| Fixed evening | 43 (13.1) |
| Fixed night | 0 (0) |
| Split | 15 (4.7) |
| Not identified | 18 (5.6) |
| Intensity of physical activity | |
| Sedentary | 70 (21.9) |
| Light | 69 (21.6) |
| Moderate | 122 (38.1) |
| Heavy and very heavy | 59 (18.4) |
| Respiratory exposure at work | |
| Yes | 137 (42.8) |
| No | 183 (57.2) |
| Intensity of respiratoryexposure | |
| Very low | 22 (6.9) |
| Low | 58 (18.1) |
| Moderate | 38 (11.9) |
| High | 14 (4.4) |
Abbreviation: BMI, Body Mass Index.
a Values are expressed as mean ± SD (median) or No. (%).
The average duration of hospitalization and drug use after discharge for the participants was 8.34 ± 7.26 days and 16 ± 15 days, respectively. A total of 36% of participants had underlying diseases, including diabetes (14%), hypertension (7%), asthma (5%), immune deficiency (1%), chronic respiratory diseases (4%), chronic renal disease (3%), cardiovascular disease (3%), rheumatologic disease (2%), chronic liver disease (1%), neurologic disease (1%), and other diseases (6%).
After RTW, about 72% of individuals reported at least one of the following symptoms: Fatigue, shortness of breath, joint pain, cough, depression, anxiety, and sleep disorders. Among these, 44% experienced symptom exacerbation with physical activity, and 26% experienced exacerbation with respiratory exposures in the workplace.
Among all participants, 239 (75%) experienced at least one complication in one organ. Muscular weakness was the most common after-COVID complication, followed by respiratory and psychological complaints. Table 2 shows the frequency of different symptoms after RTW.
At the time of completing the questionnaire, 10 individuals (3%) had not returned to work. The reasons for not returning were complications of the disease (7 individuals), fear of transmitting the disease to others (2 individuals), and fear of reinfection (1 individual). The duration of sick leave before RTW, since the onset of the disease, was 31.67 ± 33.47 days. The most common cause of delay in RTW was the physician's recommendation (2%), followed by personal belief of inability to work (44%), disease complications (30%), employer’s decision (7%), fear of transmitting the disease to others (2%), and fear of reinfection (1%).
| Symptoms | Total | Week 1 | Week 2 | Week 3 | Week 4 | Weeks 4 - 8 | After Week 8 |
|---|---|---|---|---|---|---|---|
| Fatigue | 197 (63.5) | 18 (5.8) | 37 (11.9) | 35 (11.2) | 39 (12.5) | 17 (5.4) | 50 (16.1) |
| Shortness of breath | 134 (43.2) | 16 (5.1) | 22 (7.0) | 18 (5.8) | 24 (7.7) | 12 (3.8) | 42 (13.5) |
| Cough | 55 (17.7) | 12 (3.8) | 10 (3.2) | 4 (1.3) | 7 (2.2) | 3 (0.9) | 16 (5.1) |
| Memory and concentration deficit | 68 (21.9) | 1 (0.3) | 13 (4.1) | 4 (1.3) | 9 (2.9) | 2 (0.6) | 33 (10.6) |
| Depression and Anxiety | 66 (21.2) | 8 (2.5) | 11 (3.5) | 10 (3.2) | 8 (2.5) | 5 (1.6) | 30 (9.6) |
| Sleep disorders | 68 (21.9) | 6 (1.9) | 19 (6.1) | 9 (2.9) | 7 (2.2) | 2 (0.6) | 22 (7.0) |
a Values are expressed as No. (%).
The duration of absenteeism after COVID-19 infection was significantly higher in workers who had lower respiratory tract involvement during the disease (P = 0.014), a longer duration of hospitalization and drug use (P < 0.001), or who suffered from after-COVID complications (P < 0.001).
The average duration of hospitalization was significantly higher in individuals who had severe respiratory exposures in the work environment compared to those without exposure (P < 0.05). It was significantly associated with BMI, marital status, diabetes, age, and work experience; however, no correlation was found between the duration of hospitalization and other occupational or personal factors (Table 3).
| Variables | Duration of Hospitalization (Day) | Duration of Absenteeism (Day) |
|---|---|---|
| Type of employment | ||
| Self-employed (n = 142) | 7.04 ± 5.97 | 40.88 ± 35.82 |
| Others (n = 176) | 7.43 ± 9.85 | 28.83 ± 19.28 b |
| Work shift | ||
| No (n = 184) | 7.03 ± 7.42 | 32.56 ± 22.25 |
| Yes (n = 136) | 7.57 ± 9.46 | 36.15 ± 34.66 |
| Respiratory exposure in the workplace | ||
| No (n = 184) | 7.22 ± 9.44 | 29.83 ± 23.29 |
| Yes (n = 136) | 7.31 ± 6.59 | 37.64 ± 31.29 c |
| Physical activity in the workplace | ||
| Moderate to very heavy (n = 180) | 7.34 ± 8.46 | 36.97 ± 33.68 |
| Sedentary and light (n = 140) | 7.16 ± 8.21 | 30.28 ± 18.78 |
| Observing hygienic issues in the workplace | ||
| No (n = 75) | 7.82 ± 0.75 | 44.86 ± 45.71 |
| Yes (n = 245) | 7.11 ± 8.52 | 31.16 ± 20.66 d |
| Gender | ||
| Male (n = 295) | 7.57 ± 8.58 | 35.09 ± 29.13 |
| Female (n = 25) | 3.80 ± 3.58 b | 21.69 ± 12.14 c |
| Marital status | ||
| Single (n = 24) | 4.66 ± 3.23 | 25.65 ± 19.27 |
| Married (n = 296) | 7.47 ± 8.59 d | 34.75 ± 28.90 d |
| Diabetes | ||
| No (n = 276) | 6.96 ± 8.22 | 32.47 ± 27.36 |
| Yes (n = 44) | 9.18 ± 8.90 c | 43.79 ± 32.60 b |
| Respiratory complications | ||
| No (n = 256) | 6 ± 4.32 | 29.80 ± 22.69 |
| Yes (n = 62) | 12.45 ± 15.80 b | 52.63 ± 40.85 b |
| Psychologic complications | ||
| No (n = 282) | 7.16 ± 8.68 | 32.73 ± 28.24 |
| Yes (n = 36) | 8.05 ± 4.86 b | 45 ± 27.54 b |
| Muscular weakness | ||
| No (n = 258) | 6.18 ± 4.39 | 31.20 ± 24.52 |
| Yes (n = 60) | 11.90 ± 16.21 b | 46.56 ± 39.04 b |
a Values are expressed as mean ± SD.
b P < 0.001.
c P < 0.01.
d P < 0.05.
There was a significant relationship between the duration of absenteeism and the severity of respiratory exposures (P < 0.01), the degree of symptom exacerbation with heavy activity (P < 0.001), and the degree of symptom exacerbation with respiratory agents in the workplace (P < 0.01). However, no relationship was found between the duration of absenteeism and the level of education, intensity of physical activity, or the type of shift work.
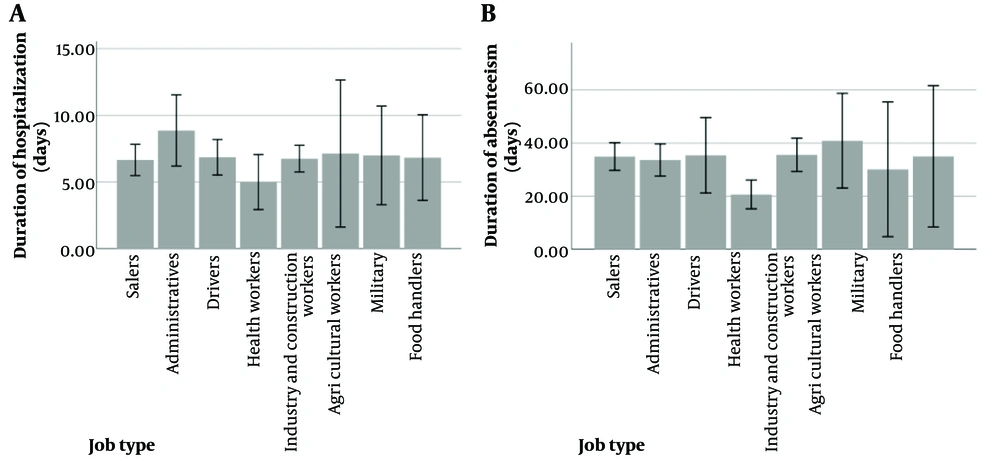
The duration of absenteeism was shortest among healthcare workers (P < 0.05), but job title did not significantly affect the duration of hospitalization (P > 0.05). Figure 1 compares the duration of absenteeism and hospitalization across different job titles.
Table 4 shows the odds ratio for sick leave of 21 days or longer, considering various factors related to the workplace and the worker.
| Independent Variables | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | P-Value | Odds Ratio (95% CI) | P-Value | |
| Age | 1.04 (1.01 - 1.07) | 0.005 | 1.01 (0.93 - 1.03) | 0.370 |
| Gender (Ref: Female) | 2.42 (1.02 - 5.71) | 0.044 | 1.09 (0.33 - 2.47) | 0.858 |
| Marital status (Ref: Single) | 3.62 (1.48 - 8.82) | 0.005 | 1.50 (0.73 - 6.21) | 0.457 |
| Number of dependents | 1.38 (1.16 - 1.65) | < 0.001 | 1.18(0.89 - 1.55) | 0.230 |
| BMI | 1.06 (1.00 - 1.11) | 0.031 | 1.01 (0.95 - 1.06) | 0.776 |
| Work experience | 1.05 (1.02 - 1.08) | < 0.001 | 1.04 (0.99 - 1.09) | 0.064 |
| Type of employment (Ref: Self-employed) | 0.52 (0.323 - 0.844) | 0.008 | 0.56 (1.03 - 0.30) | 0.061 |
| Workplace respiratory exposure | 1.71 (1.02 - 2.86) | 0.042 | 1.08 (0.57 - 2.02) | 0.804 |
| Lower respiratory symptoms (Ref: No symptom) | 1.74 (1.07 - 2.83) | 0.024 | 1.17 (0.65 - 2.12) | 0.597 |
| Duration of hospitalization | 1.12 (1.05 - 1.19) | < 0.001 | 1.03 (0.96 - 1.09) | 0.337 |
| Duration of drug consumption | 1.06 (1.04 - 1.10) | < 0.001 | 1.06 (1.03 - 1.10) | < 0.001 |
| Suffering from diabetes (Ref: No diabetes) | 3.49 (1.50 - 8.14) | 0.004 | 2.71 (0.99 - 7.40) | 0.051 |
| Muscular weakness (Ref: No weakness) | 3.49 (1.29 - 5.07) | 0.007 | 2.19 (0.96 - 5) | 0.062 |
| Respiratory complications (Ref: No complication) | 6.41 (2.65 - 15.43) | < 0.001 | 3.34 (1.27 - 8.77) | 0.014 |
| Psychological complications (Ref: No complication) | 4.89 (1.67 - 14.28) | 0.004 | 3.62 (1.06 - 12.34) | 0.040 |
Abbreviation: BMI, Body Mass Index.
5. Discussion
This study investigated the factors affecting RTW among workers hospitalized due to COVID-19. The results indicated that certain personal and occupational factors influenced RTW. After adjusting for confounding factors, the most significant risk factors affecting RTW were the severity of the disease, as measured by the number of days of medication use for COVID-19 infection, and the presence of pulmonary and psychological complications. These findings are consistent with the results of the study conducted by Jacobsen et al. (13).
In the current study, no significant relationship was found between occupational factors and the average number of hospitalization days as an indicator of disease severity. This study was limited to hospitalized cases, excluding mild cases that did not require hospitalization and cases that resulted in death. Additionally, individuals hospitalized in the ICU were not analyzed separately, while many previous studies have focused on mortality and hospitalization as indicators of COVID-19 severity. Mutambudzi et al. investigated the relationship between socioeconomic risk factors related to work, health, and lifestyle and the hospitalization rate and mortality due to COVID-19 among 120 075 participants in the UK. They concluded that healthcare workers had the highest risk of severe COVID-19 (14). Another study found that healthcare and transportation workers had the highest mortality rates among various occupational subgroups (15).
In the present study, healthcare workers had fewer days of absenteeism compared to other occupations. This difference was likely due to their younger age and earlier treatment. The results of previous studies in this field have been varied and sometimes contradictory. Some studies indicated that individuals with direct patient contact had longer absenteeism due to COVID-19. This variation may be linked to the timing of the studies, which were conducted early in the pandemic (16).
Another study showed that working in frontline jobs related to combating COVID-19 did not lead to increased mortality or absenteeism (9). The differences in findings may also be attributed to local and cultural factors, as well as potential immunity established in healthcare workers due to early vaccination, compared to workers in other sectors. Furthermore, the commitment to RTW in healthcare workers, driven by the high societal demand for healthcare services, may have contributed to their faster return to work. As observed in the present study, self-employed individuals returned to work later, with a significant difference compared to other types of employment.
Observance of hygiene practices by individuals and coworkers, along with the provision of health measures in the work environment by employers, are important factors that reduce anxiety and facilitate RTW (7). This is consistent with the results of the current study, which compared the adherence to hygiene practices and work-related mitigation factors across different occupations. The least adherence was observed among farmers, livestock breeders, and construction workers (75%), while the highest adherence was observed in healthcare workers (100%).
Age, obesity, and diabetes are well-known underlying conditions that increase the risk of more severe COVID-19 (17), and this was also demonstrated in the present study through the increased duration of hospitalization and absence from work.
We found no association between RTW after COVID-19 hospitalization and other personal or occupational factors such as gender, number of dependents, marital status, shift work, shift type, respiratory exposure, or physical activity. Several confounding factors may influence these relationships, as demonstrated in previous studies (18, 19). Mental health issues, such as anxiety, depression, or fear-avoidance, can also affect RTW. Moreover, individuals with depression are less likely to return to their pre-injury levels of daily life activities and instrumental tasks (20). It has also been found that COVID-19 can cause mental health complications in sufferers. For instance, one in five people with severe COVID-19 continued to experience mood symptoms such as depression, anxiety, or post-traumatic stress disorder (PTSD) six months after the end of the physical illness (10). In the present study, 11% of participants reported mental health complications caused by COVID-19 at the time of the interview, and 21% reported depression and anxiety at least one week after RTW, which significantly delayed their return to work.
There was a direct and significant relationship between the duration of hospitalization and the development of mental complications caused by COVID-19. This suggests that psychological factors are as important as physical complications, or even more important, in the RTW process. In other words, focusing on severe cases of COVID-19, providing early intervention to reduce psychological complications, and ensuring the observance of hygiene measures in the workplace can help reduce absenteeism after COVID-19.
There were several limitations in this study: Data were collected through interviews, which may not have been objective, and thus, results could have been influenced by recall bias. Additionally, we could not investigate individuals who did not participate in the study. Some important factors that could affect the time to RTW, such as the mode of commuting to work, income levels, the possibility of remote work, varying workplace absence policies, and social and familial support, were not assessed in the present study. Moreover, the number of women in the study was small and insufficient for statistical comparison between genders.
5.1. Conclusions
In this study, the most important and direct risk factors for delayed RTW were the severity of the disease, in terms of the duration of medication use, and the development of pulmonary and psychological complications after the illness.