1. Background
The Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) rank among the most severe infectious diseases of the late 20th century (1). Since it was first identified in 1981, AIDS has emerged as a significant global health issue of remarkable scale and an unparalleled crisis. Four decades after its identification, the virus has spread nearly worldwide, profoundly influencing modern medical practices, public health initiatives, and various facets of society. Worldwide, more than 35 million individuals were living with HIV/AIDS, and approximately 1.6 million died from complications related to the disease (2). The statistics of the global HIV and AIDS epidemic presented by the World Health Organization (WHO) and Joint United Nations Programme on HIV/AIDS (UNAIDS) in 2019 estimated that 38.4 million people worldwide were living with HIV/AIDS, and in 2021, 650,000 people died as a result of HIV/AIDS-related causes (3). Moreover, in 2019, an estimated 1.5 million people were infected by HIV (4).
With the advancement of antiretroviral therapy (ART), HIV infection is now considered a chronic condition, allowing individuals living with HIV (PLHIV) to enjoy an increased life expectancy (5). The enhanced survival of PLHIV due to ART has led to unforeseen consequences, including a wide array of health issues. One such consequence is the increased prevalence of ocular complications, which has become a significant concern for this population (6). Ophthalmic diseases impact 70% - 80% of people living with HIV (7). The HIV-related ophthalmic diseases encompass a diverse array of conditions, ranging from disorders affecting the eyelids and surrounding structures to those impacting the posterior segment of the eye, including the optic nerve and visual pathways. The initial report on ocular manifestations of AIDS was published by Holland et al. (8). In 1982, additional research demonstrated various AIDS-related conditions affecting the eye and the surrounding orbit (9-11).
The possible eye-related effects of untreated HIV infection can cause visual impairment and may eventually result in blindness. A previous study indicated that as many as 2% of PLHIV experience vision loss (12) and encounter difficulties related to visual impairment, which include significant financial and psychosocial challenges (13). Therefore, screening for eye complications should be integrated into the standard follow-up care for PLHIV. Additionally, the clinical characteristics of these ocular manifestations vary by country, particularly between high-income and low- to middle-income nations (14). Several studies have highlighted the significant role of CD4 count in the development of ocular manifestations in HIV-positive patients. According to a systematic review by Doe and Smith, patients with lower CD4 counts are at a higher risk of developing severe ocular conditions, including retinopathy and uveitis (15, 16).
2. Objectives
Consequently, this study aimed to evaluate ocular manifestations in PLHIV and their relationship with CD4 count.
3. Methods
3.1. Setting and Design
This cross-sectional study was conducted at the Behavioral Health Counseling Center affiliated with Hamadan University of Medical Sciences (UMSHA), the only referral center in Hamadan city. A total of 114 PLHIV were enrolled through convenience sampling. The data were collected between January 1 and December 30, 2020. Despite delays in processing and publication that were beyond our control, the findings remain pertinent to current HIV-related ocular issues.
3.2. Data Collection
3.2.1. Inclusion Criteria
Adults aged 18 and older, diagnosed with HIV infection, and receiving care at the Behavioral Diseases Counseling Center in Hamadan, Iran, were included in the study.
3.2.2. Exclusion Criteria
The HIV/AIDS patients who did not consent to participate and cooperate in the study were excluded.
3.2.3. Sampling Method
Convenience sampling was used to enroll participants who met the inclusion criteria. To minimize selection bias, all participants were selected from the city's only behavioral counseling referral center, ensuring a consistent demographic. However, the use of convenience sampling may limit the generalizability of the findings. To reduce measurement bias, all ocular assessments were conducted by a single trained ophthalmologist using standardized procedures.
3.2.4. Sample Size Estimation
The sample size of 114 participants was chosen based on an expected ocular manifestation prevalence of 50%, with a margin of error of 5% and a 95% confidence level. This size is adequate to detect statistically significant associations between ocular manifestations and CD4 counts. Data extracted retrospectively included age, gender, education, job, weight, addiction, duration of infection, duration of treatment, CD4 count, viral load, prison history, transmission, comorbidity, and ART status. A thorough eye examination of both eyes was conducted, encompassing the assessment of corrected visual acuity (VA) using a Snellen chart, an anterior segment evaluation with a slit lamp, measurement of intraocular pressure (IOP) via Goldmann applanation tonometry, and a dilated fundus examination.
3.3. Statistical Methods
Data analysis was performed using descriptive statistics, which included mean ± standard deviation (SD), median, frequencies, and percentages as appropriate. Chi-square tests and Fisher’s exact tests were used to analyze categorical variables, while continuous variables were assessed using t-tests. A result was deemed statistically significant if the P-value was less than 0.05. All analyses were conducted using Stata software (version 14.1) from StataCorp, College Station, TX, USA.
4. Results
This study was conducted on 114 PLHIV, comprising 75 males (65.8%). The average age was 39.64 ± 12.15 years for men and 39.48 ± 12.09 years for women. Patients were in the age range of 2 to 65 years. According to Table 1, the mean duration of HIV infection was 79.07 ± 58.92 months, the mean duration of treatment was 52.43 ± 36.69 months, the mean CD4 count was 527.62 ± 405.02 cells/µL, and the mean viral load was 14,908 ± 70,857.83. Since the CD4 and duration of infection variables have a non-normal distribution, the Mann-Whitney test was used to compare CD4 for the group with or without ocular manifestations (Table 1).
| Variables and Subgroups | Values |
|---|---|
| Age (y) | 39.58 ± 12.10 |
| Gender | |
| Male | 75 (65.8) |
| Female | 39 (34.20) |
| Education | |
| Illiterate | 15 (13.2) |
| Elementary | 30 (26.3) |
| Guidance | 38 (33.3) |
| High school | 23 (20.2) |
| College | 8 (7) |
| Job | |
| Employee | 6 (5.3) |
| Worker | 3 (2.6) |
| Housewife | 12 (10.5) |
| Businessman | 28 (24.6) |
| Unemployed | 43 (37.7) |
| Other | 22 (19.3) |
| Weight (kg) | 65.33 ±17.34 |
| Duration of HIV infection (mo) | 79.07 ± 58.92 |
| Duration of HIV treatment (mo) | 52.43 ± 36.69 |
| CD4+ count (cell/µL) | 527.62 ± 405.02 |
| Viral load (IU/mL) | 14908 ± 70857.83 |
| Comorbidity | |
| HBV | 10 (8.8) |
| HCV | 47 (41.2) |
| Diabetes | 4 (3.5) |
| Blood pressure | 6 (5.3) |
| Heart disease | 3 (2.6) |
| Other | 8 (7) |
| Ocular manifestation (according to the region involved) | |
| Eyelid manifestations | 43 (37.7) |
| Conjunctival manifestations | 39 (34.2) |
| Corneal manifestations | 19 (16.7) |
| Retinal manifestations | 20 (17.5) |
Abbreviation: HIV, human immunodeficiency virus.
a Values are expressed as mean ± SD or No. (%).
Of the 114 patients studied, 60 patients (52.6%) had a history of addiction, 40 patients (35%) had a history of imprisonment, 18 patients (15.8%) had high-risk sexual behaviors, 14 patients (12.3%) had shared injections, 1 patient (0.9%) had tattoos, 6 patients (5.26%) had transmission from an infected mother, and 44 patients (38.59%) had multiple exposures as the way they contracted the disease. Ten patients (8.8%) had hepatitis B, 47 patients (41.2%) had hepatitis C, 4 patients (3.5%) had diabetes, 6 patients (5.3%) had high blood pressure, 3 patients (2.6%) had heart disease, and 8 patients (7%) had other diseases.
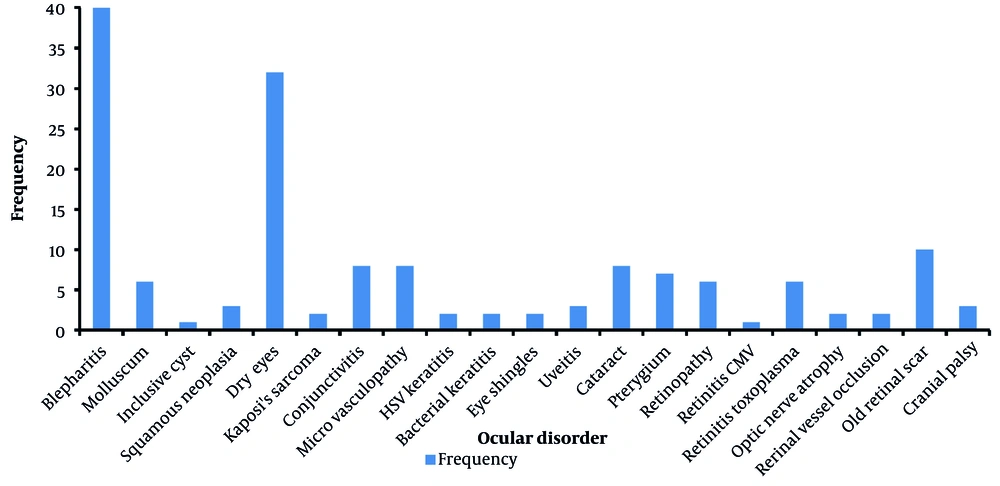
Sixty-six patients (57.89%) had ocular manifestations. Separately, 37.7% of patients had eyelid manifestations, 34.2% had conjunctival effusions, 16.7% had corneal manifestations, and 17.5% had retinal manifestations (Table 1). The most common ocular manifestations in patients were blepharitis (35.1%) and dry eye (28.1%) (Table 2 and Figure 1). A statistically significant relationship existed between patients with retinal manifestations and CD4 count (P-value: 0.001) (Table 3).
| Ocular Disorder | Frequency (%) |
|---|---|
| Blepharitis | 40 (35.1) |
| Mollusca | 6 (5.3) |
| Inclusive cyst | 1 (0.9) |
| Squamous neoplasia | 3 (2.6) |
| Dry eyes | 32 (28.1) |
| Kaposi's sarcoma | 2 (1.8) |
| Conjunctivitis | 8 (7) |
| Micro vasculopathy | 8 (7) |
| HSV keratitis | 2 (1.8) |
| Bacterial keratitis | 2 (1.8) |
| Eye shingles | 2 (1.8) |
| Uveitis | 3 (2.6) |
| Cataract | 8 (7) |
| Pterygium | 7 (6.1) |
| Retinopathy | 6 (5.3) |
| Retinitis CMV | 1 (0.9) |
| Retinitis toxoplasma | 6 (5.3) |
| Optic nerve atrophy | 2 (1.8) |
| Retinal vessel occlusion | 2 (1.8) |
| Old retinal scar | 10 (8.8) |
| Cranial palsy | 3 (2.6) |
| Variables | CD4 Count | Frequency | Mean ± SD | P-Value | |||
|---|---|---|---|---|---|---|---|
| > 500 | 200 - 499 | < 200 | Unknown | ||||
| Eyelid manifestations | 18 (41.9) | 18 (41.9) | 7 (16.3) | 0 | 43 | 490.12 ± 299.30 | 0.09 |
| Conjunctival manifestations | 17 (43.6) | 16 (41) | 6 (15.4) | 0 | 39 | 501.62 ± 314.45 | 0.18 |
| Corneal manifestations | 8 (42.1) | 8 (42.1) | 2 (10.5) | 1 (5.3) | 19 | 492.39 ± 274.12 | 0.12 |
| Retinal manifestations | 4 (20) | 10 (50) | 4 (20) | 2 (10) | 20 - 18 | 380.89 ± 237.05 | 0.003 |
Table 1 displays the baseline characteristics of the PLHIV. The results showed that 47 patients had hepatitis C simultaneously with HIV, which is more than other diseases (Table 1). Retinopathy manifestations were more prevalent in patients with CD4 counts above 200, which aligns with findings from previous studies. This could be due to the relative preservation of immune function in patients with higher CD4 counts, which may result in a delayed onset or milder ocular manifestations compared to those with lower counts (Table 3). The number of CD4 cells is directly proportional to the strength of the immune system (Table 4). A decrease in CD4 cell count has led to an increase in the manifestations of retinal diseases among patients living with HIV. In patients who did not receive ART, retinal manifestations were more prevalent (P-value: 0.01) (Table 5).
| Variables | < 200 | 200 - 499 | > 500 | Unknown |
|---|---|---|---|---|
| Eyelid manifestations | 7 (16.3) | 18 (41.9) | 18 (41.9) | - |
| Conjunctival manifestations | 6 (15.4) | 16 (41) | 17 (43.6) | - |
| Corneal manifestations | 2 (10.5) | 8 (42.1) | 8 (42.1) | 1 (5.3) |
| Retinal manifestations | 4 (20) | 10 (50) | 4 (20) | 2 (10) |
a Values are expressed as No. (%).
| Variables | With ART | Without ART | P-Value |
|---|---|---|---|
| Eyelid manifestations | 43 (40.2) | 0 (0) | 0.003 |
| Conjunctival manifestations | 38 (35.5) | 1 (14.3) | 0.1 |
| Corneal manifestations | 18 (16.8) | 1 (14.3) | 0.8 |
| Retinal manifestations | 17 (15.9) | 3 (42.9) | 0.01 |
Abbreviations: ART, antiretroviral therapy.
a Values are presented as No. (%).
5. Discussion
In this study, out of 114 PLHIV, most of the study patients were unemployed, and only a small percentage had a college education. Ninety-six patients (84.2%) lived in the city, and 18 (15.8%) lived in the village. Sixty-six patients had ocular manifestations, most frequently related to eyelid manifestations. Out of 43 patients with eyelid manifestations, 66.7% had a history of addiction, which was statistically significant (P-value: 0.003). In this study, 57.89% of the patients had ocular manifestations, and in a study by Sudharshan et al. in India, 65.5% had ocular manifestations (17). The results of this study are consistent with our study. In 2013, conjunctivitis and blepharitis were reported as the most common ocular manifestations in HIV patients (18), consistent with our study. In 2015, Nishijima et al. reported that HIV retinopathy was the most common ocular manifestation of PLHIV (19), which was inconsistent with our study. In a study conducted by Pedro-Egbe et al. among 411 PLHIV, the number of women compared to men was 2:1. In contrast, in our research, the number of men was greater than women, which was inconsistent with our study. Ocular manifestations were seen in 37.1% of the patients, less than in our study (57.89%) (20). In other studies, conjunctival microvasculopathy was identified as the most prevalent ocular manifestation among patients; however, in our research, blepharitis and dry eye were found to be the most common. Similar to our findings, most patients in our study had CD4 counts exceeding 200 cells/µL. The overall prevalence of ocular manifestations in our study was greater than that reported in the other study. While retinal manifestations were the most common in those studies, they ranked as the least frequent in our research, following corneal manifestations (20).
The findings of this study align with the research conducted by Saadouli et al., which involved 98 PLHIV participants, with 36 of them presenting ocular manifestations. In their study, the number of male patients was double that of females. Dry eye was identified as the most prevalent ocular manifestation. Additionally, in most patients with ocular manifestations, the CD4 count was below 200 cells/µL, which contrasts with the results of our study (10). This high CD4 count in the patients of our study is probably due to regular visits and receiving ART.
In the Tanzanian study involving 296 PLHIV, 124 exhibited ocular manifestations, with optic atrophy being the most common. The prevalence of these ocular complications was notably higher among patients who were not receiving Highly Active Antiretroviral Therapy (HAART) and those with a CD4 count of less than 200 cells/μL. The weakening of the immune system may increase ocular manifestations in PLHIV (21). CD4 is an effective indicator for assessing a patient's immune and clinical condition, as well as their risk of developing opportunistic infections (22). If the viral load increases in patients who do not use ART or are resistant to a drug, it can accelerate the destruction of CD4 T cells, weaken the immune system, and increase susceptibility to infections and ocular manifestations (23).
In Ghana, a study involving 100 PLHIV found that the prevalence of ocular manifestations was 48%. These complications were more commonly observed in patients with CD4 counts below 200 cells/μL. Most ocular manifestations were related to retinal microvasculopathy in patients. Decreases in CD4+ counts can increase ocular complications in PLHIV (24). In our study, almost all patients received ART, and their CD4 count is above 200 cells/μL, but the prevalence of ocular manifestations is 57.89%. It should be evaluated that in addition to receiving ART and CD4 count, what other factors influence the emergence of these manifestations?
In other studies (25) conducted in Iran, the prevalence of ocular manifestations was reported as 10.6%, which is lower than the prevalence in our study. Factors such as coinfection diseases, education, occupation, and personal health can influence the prevalence of these manifestations. In our study, most patients had no college education and were unemployed. Also, a statistically significant relationship existed between patients with addiction and eyelid and conjunctival manifestations. Table 6 compares the results of other studies with our study.
This study had several limitations, including its cross-sectional design, which limits the ability to establish causality. Additionally, the study was conducted at a single health center, which may not reflect the broader HIV-positive population. Finally, the reliance on medical records may have led to incomplete or inaccurate data. The findings of this study may not be fully generalizable to HIV-positive populations in other regions due to demographic and healthcare access differences. Further studies in diverse settings are needed to validate these findings.
5.1. Conclusions
In the present study, most PLHIV regularly visited health centers and were under regular treatment with ART. Based on the present study's results, the retinal manifestation rate was significantly higher only in patients who did not receive ART. Additionally, their CD4 count was significantly lower than that of patients without ocular manifestations, highlighting the important role of treatment and immune system status in eye manifestations in these patients.