1. Introduction
Q fever is a zoonotic infectious disease caused by Coxiella burnetii, a Gram-negative intracellular bacterium that is highly resistant to unfavorable factors in the external environment (1). The infection is challenging to diagnose due to a wide range of symptoms that mimic other illnesses. Additionally, healthcare providers may not routinely test for Q fever, leading to potential underdiagnosis and underreporting (2, 3). The reservoirs of C. burnetii are usually livestock such as goats, sheep, and cattle. Coxiella burnetii is often transmitted to these animals through bites from soft and hard ticks. The common route of transmission to humans is inhalation of dust contaminated with body fluids or birth products of infected animals. Another way of transmission to humans is the consumption of unpasteurized dairy products from infected animals. Due to regular contacts with livestock, farm workers and veterinarians are at the highest risk of contracting the disease (1).
The incubation period lasts an average of 20 days. The acute clinical manifestations are non-specific and include flu-like symptoms. In 60% of cases, the infection can be asymptomatic. In 1-5% of cases, acute Q fever progresses to a chronic infection, which can manifest itself within a few months or several years after the acute infection. Possible signs and symptoms include endocarditis, chronic hepatitis, chronic vascular lesions, osteomyelitis, and osteoarthritis (4). Serologic testing is a routine method of confirming Q fever in both the acute and chronic forms. Acute disease is usually associated with the detection of antibodies to phase II C. burnetii antigens, whereas the detection of IgG against phase I antigens is essential for the diagnosis of chronic Q fever. Polymerase chain reaction (PCR) is another highly informative approach for the diagnosis of acute and chronic C. burnetii infection (1, 2). Doxycycline remains the most effective treatment option for Q fever (2). If left untreated, the mortality rate can reach 1-2% for acute Q fever (2) and as high as 60% for chronic Q fever (5).
Epidemiological surveillance for C. burnetii infection is currently lacking in Kazakhstan, despite evidence from several studies indicating the circulation of the pathogen in southern Kazakhstan, which includes the regions of Turkestan, Zhambyl, Almaty, and Zhetisu (6). Historical data from 1980 reported incidence rates ranging from 1 to 18 cases per 100,000 population in various areas of southern Kazakhstan (7). More recently, a 2020 study documented a seroprevalence of 1.3% (11/910) among residents of the Zhambyl region (8). In the Turkestan region, 22% of livestock were found to be seropositive for antibodies to C. burnetii, and 14.8% of ticks tested positive for C. burnetii DNA, suggesting that the disease may be endemic in certain areas of southern Kazakhstan (9). As Q fever is an occupational disease that affects farm workers, it is rarely diagnosed in children. Therefore, the full extent of the impact of Q fever on the health of children remains undetermined (10). The aim of this study was to retrospectively analyze the medical records of an infant patient with serological findings indicative of Q fever.
2. Methods and Study Design
We retrospectively analyzed medical records and conducted serologic testing in a child who had initially been diagnosed with acute respiratory viral infection and bronchopneumonia of unknown etiology. The patient's parents gave their consent for the material to be published. This study was also reviewed and approved by the Ethics Committee of the National Center for Biotechnology (approval no. 1 issued on 31 January, 2023).
An acute phase serum sample and a convalescent phase serum sample of the patient were collected on the 8th day of the illness and 17 weeks after the onset of the disease, respectively, and shipped on frozen gel packs to the Central Reference Laboratory in Almaty, Kazakhstan, for further analysis. Serologic analysis for the presence of IgG antibodies against C. burnetii antigens was first performed using an ID Screen® Q Fever Indirect Multi-species enzyme-linked immunosorbent assay (ELISA) kit (IDVet) aimed at detecting both phase I and phase II antibodies according to the manufacturer’s instructions. As recommended by the manufacturer, a serum dilution of 1:50 was used. The optical densities (ODs) were measured by BioTek (BioTek Instruments) at 450 nm. The percentage of serum positivity (S/P %) was calculated as follows: S/P % = (OD tested sample − OD negative control) / (OD positive control − OD negative control) × 100. Samples with an S/P value < 40% were considered negative, those between 40 and 50% inconclusive, those between 50 and 80% positive, and those with S/P > 80% strongly positive. The positive samples were further analyzed for the presence of antibodies against C. burnetii phase I and phase II antigens using an Anti-Coxiella burnetii Phase I IgG ELISA kit (Q-Fever) (Abcam, sensitivity is > 90% according to the manufacturer) and an Anti-Coxiella burnetii Phase II IgG ELISA kit (Q-Fever) (Abcam, sensitivity is > 90% according to the manufacturer), respectively. A dilution protocol of 1:100 was used according to the manufacturer’s instructions. Samples were classified as positive if the OD value was more than 10% above the cut-off value and as negative if the OD value was less than 10% below the cut-off value. The seropositive sample was also analyzed for C. burnetii DNA by PCR using an AmpliSense®Coxiella burnetii-FL (AmpliSense) kit according to the manufacturer’s instructions. DNA was extracted using a QIAamp DNA Mini Kit (Qiagen).
2.1. Case Presentation
On December 14, 2022, a 10-month-old boy from the village of Keregetas, Tolebi district, Turkestan region, Kazakhstan, fell ill with a persistent fever of 38.5 - 39.0°C, accompanied by a non-productive cough, general weakness, and refusal to eat. Antipyretics had no effect, and his condition progressively worsened. On day 4 of his illness, he was hospitalized with a presumptive diagnosis of acute respiratory viral infection. On examination, he appeared pale, was short of breath, and had a dry cough. The throat was moderately hyperemic. The patient had a fever of 38.5°C and a tachycardia of 124/minute. The child’s weight was 9 kg. He was fully conscious. Enlargement of the spleen was noted.
On day 8 of illness, laboratory examination revealed reduced hemoglobin, normal leukocyte count, relative neutropenia, and relative lymphocytosis (Table 1). Tests for other infectious diseases (e.g., COVID-19, tuberculosis, brucellosis, yersiniosis, rickettsiosis, Lyme disease, human immunodeficiency virus (HIV), syphilis) were negative. There were no significant changes in the urinalysis. The chest X-ray showed signs of bronchopneumonia. The patient had no history of tick bites or travel. The physicians diagnosed an acute respiratory viral infection with bronchopneumonia of unknown etiology. The patient received empirical antibacterial therapy with intramuscular cefazolin for 5 days, in accordance with local guidelines for managing fever of unknown origin in children. Additional treatment included inhaled bronchodilators (ipratropium bromide/fenoterol hydrobromide) for 4 days and intravenous prednisolone in combination with euphylline for 3 days (Table 1). The patient responded well to treatment and was discharged from the hospital on day 9 of the illness with improvement.
| Marker (Reference Range) | Day of Illness | |||||
|---|---|---|---|---|---|---|
| 5th | 6th | 7th | 8th | 9th | 10th | |
| Blood analysis results | ||||||
| Leukocyte count (4.5 - 9.5 × 109/L) | 9.3 /L | - | - | 5.7 /L | - | - |
| Neutrophil (50 - 70); (%) | 60.3 | - | - | 11 | - | - |
| Lymphocyte (18 - 40); (%) | 30.3 | - | - | 76 | - | - |
| Monocytes (2 - 8) ;(%) | 8.3 | - | - | 10 | - | - |
| Eosinophils (0 - 5); (%) | 0.3 | - | - | 0 | - | - |
| Basophils (0.5 - 1); (%) | 1 | - | - | 1 | - | - |
| Platelets (125 - 350×109/L) | 187 /L | - | - | 217 /L | - | - |
| Erythrocytes (3.8 - 5.8×1012/L) | 4.1 /L | - | - | 4.3 L | - | - |
| Hemoglobin (115 - 150 g/L) | 93 g/L | - | - | 97 g/L | - | - |
| Erythrocyte sedimentation rate (15 - 25 mm/h) | 2 | - | - | - | - | - |
| Urine analysis results | ||||||
| Proteins (≤ 150 mg/d) | 0 mg/d | |||||
| Bilirubin (0 umol/L or negative) | - | 0 | - | - | - | - |
| Glucose (0 mmol/L) or negative | - | 0 | - | - | - | - |
| Ketone bodies (0 mmol/L or negative) | - | 0 | - | - | - | - |
| White blood cells (≤ 2 - 5 WBCs/hpf) | - | 2.2 | - | - | - | - |
| Nitrites (negative) | - | 0 | - | - | - | - |
| Specific gravity (1.005 - 1.025) | - | 1.020 | - | - | - | - |
| рН (5.5 to 6.5) | - | 5.5 | - | - | - | - |
| Urobilinogen (0 umol/L) | - | 0 | - | - | - | - |
| Other tests | ||||||
| SARS-CoV-2 PCR | - | Negative | - | - | - | - |
| Microprecipitation reaction with cardiolipin antigen antibodies to Treponema pallidum | - | Negative | - | - | ||
| Stool test for Ascaris lumbricoides | - | Negative | - | - | - | - |
| Stool test for Enterobius vermicularis | - | Negative | - | - | - | - |
| Bacteria culture test | - | no growth of microflora detected | - | - | - | - |
| Treatment | - Antibacterial therapy: Cefazolin intramuscularly (0,45 g twice a day) with novocaine; -Inhalations with Sodium chloride + ipratropium bromide/fenoterol hydrobromide (2 mL 3 times a day); - Treatment of iron deficiency and anemia with Ferrovit C; - Prednisolone (18 mg twice a day) with Euphylline (19 mg twice a day) | - Antibacterial therapy: Cefazolin intramuscularly (0,45 g twice a day) with novocaine; -Inhalations with Sodium chloride + ipratropium bromide/fenoterol hydrobromide (2 mL 3 times a day); - Treatment of iron deficiency and anemia with Ferrovit C; - Prednisolone (18 mg twice a day) with Euphylline (19 mg twice a day) | Antibacterial therapy: Cefazolin intramuscularly (0,45 g twice a day) with novocaine; -Inhalations with Sodium chloride + ipratropium bromide/fenoterol hydrobromide (2 mL 3 times a day); - Treatment of iron deficiency and anemia with Ferrovit C; - Prednisolone (18 mg twice a day) with Euphylline (19 mg twice a day) | Antibacterial therapy: Cefazolin intramuscularly (0,45 g twice a day) with novocaine; -Inhalations with Sodium chloride + ipratropium bromide/fenoterol hydrobromide (2 mL 3 times a day); - Treatment of iron deficiency and anemia with Ferrovit C | Antibacterial therapy: Cefazolin intramuscularly (0,45 g twice a day) with novocaine | |
| Outcome | Hospitalization | Chest X-ray results revealed signs of right-sided bronchopneumonia | Discharge from the hospital with an improvement | |||
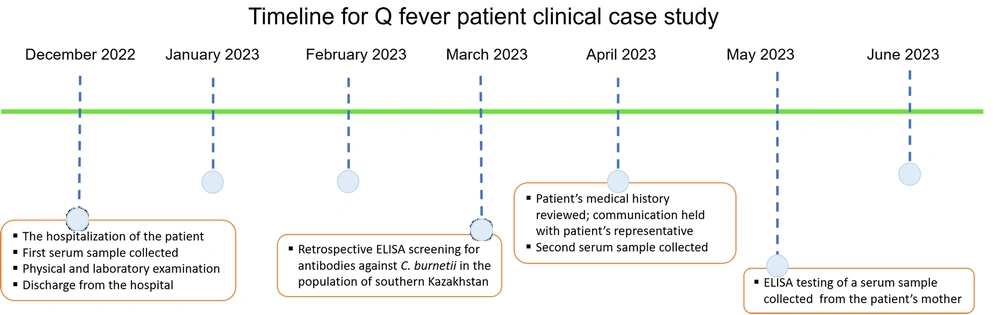
A project was initiated to study the prevalence of Q fever in the southern region of Kazakhstan, and biomaterial was collected from patients with manifestations of acute or chronic Q fever (Figure 1). The result of serologic analysis of an acute and a convalescent serum sample collected from the patient, performed with an ID Screen® Q Fever Indirect Multi-species kit, showed positive results for IgG antibodies against C. burnetii (S/P = 63.4% and S/P = 86.1%, respectively). Further testing of the acute phase sample demonstrated positive results for IgG phase I C. burnetii antibodies at a dilution of 1:100 and negative results for IgG phase II C. burnetii antibodies at a dilution of 1:100. A serum sample from the convalescent phase showed negative results for both IgG phase II and phase I C. burnetii antibodies. The PCR analysis of the serum samples for C. burnetii DNA was negative.
In May 2023, we collected an additional epidemiologic history. The patient's mother reported that she had kept a goat and had fed her son unpasteurized goat’s milk for several months. In addition, antibodies against C. burnetii (S/P = 86.1%) were detected in a serum sample obtained from the patient’s mother in March 2023 using an ELISA test performed with an ID Screen® Q Fever Indirect Multi-species kit. Due to the young age of the child, which ruled out a previous infection with C. burnetii, the pronounced clinical picture, the epidemiological factors (consumption of unpasteurized milk in the past), and serological data, the child was retrospectively diagnosed with chronic Q fever.
3. Discussion
The recognized standard for confirmation of acute Q fever by serology is a fourfold increase in IgG antibodies in serum against phase II of C. burnetii (11). Due to the requirement for detecting this rise in titer, ELISA tests are infrequently employed for diagnosis, and the indirect fluorescent antibody test (IFA) remains the most prevalent method for assessing anti-C. burnetii IgG titers. However, the IFA method lacks standardization across various laboratories and cannot be automated. From this point of view, the ELISA stands out as a more appealing option for the diagnosis of Q fever. Several studies have assessed the diagnostic value of the ELISA method for the diagnosis of Q fever. A study by Wegdam-Blans et al. demonstrated a very high sensitivity of ELISA for the detection of low titers (1:1,024) of IgG antibodies against C. burnetii phase I (12). Similar findings were reported by van der Hoek et al. (13). A recent study by Ledda et al. showed that the ELISA test is a valid support for clinical diagnosis and improves the surveillance of patients at risk of contracting Q fever (14).
In our study, the diagnosis of Q fever in the patient was based on consistent results of serologic analysis performed using ELISA kits from two manufacturers. However, while phase II IgG antibodies are commonly predominant during the primary infection and remain detectable up to 15 days after the onset of clinical symptoms, exhibiting higher titers compared to phase I IgG antibodies (11), our study revealed elevated phase I IgG antibodies in the acute phase serum, alongside negative results for phase II IgG antibodies. The reasons for this are unclear. One can speculate that the serologic response in infants differs from that described in adult patients. A study by Wielders et al. showed that there are large differences between individuals at the onset of the phase I and phase II IgG antibody response (15). Another consideration is the potential detection of maternal antibodies in the infant, which could be supported by the presence of antibodies to C. burnetii in a serum sample received from the patient’s mother. However, the clinical presentation, which is consistent with the symptoms of Q fever, makes this hypothesis less likely.
The typical clinical picture of acute Q fever in children resembles common childhood ailments such as influenza-like symptoms, pneumonia, or respiratory tract infections. Fatigue, cough, headache, and fever are frequently observed in children (16). Typically, pneumonia in Q fever infection leads to a dry to productive cough, pleuritic chest pain, and focal or bilateral lung involvement (17). Similar findings were observed in our patient. Laboratory abnormalities in support of acute Q fever are nonspecific and may include mild transaminase elevations, thrombocytopenia, and either leukopenia or leukocytosis (18). In this study, the patient exhibited reduced hemoglobin, normal leucocyte count, relative neutropenia, and relative lymphocytosis.
Although treatment with doxycycline is preferred in acute pediatric patients, trimethoprim/sulfamethoxazole may be given as an alternative in children under 8 years of age with a benign course. Although cephalosporins have some broad-spectrum activity against various bacteria, they are not the primary choice for the treatment of Q fever. In our case, however, the patient responded well to the treatment with cefazolin and was discharged from the hospital with a marked improvement in his condition.
This case report has some serious limitations. For the serological tests, we used ELISA instead of IFA because of its availability. This limited our ability to perform an in-depth serologic study to determine antibody titers. A fourfold increase in IgG titers against C. burnetii antigens could significantly support the diagnosis of acute infection. Additionally, dynamic follow-up was complicated by the patient’s distant residence. Furthermore, we faced a limitation in testing the goat from the patient's household since it had been sold prior to the commencement of the study.
3.1. Conclusions
In Kazakhstan, medical personnel have a low suspicion of Q fever in patients, primarily due to low awareness and the non-specific symptoms of the infection. In this study, we retrospectively diagnosed acute Q fever in a child who developed bronchopneumonia. The results of the study emphasize the urgent need for epidemiological surveillance of Q fever in the southern region of Kazakhstan and the improvement of serological diagnostic methods in the country. As this is the first documented case of pediatric Q fever in southern Kazakhstan, the study also aims to demonstrate the importance of recognizing Q fever as a possible cause of illness in children in the studied region.