1. Background
Measles, a highly contagious viral illness attributed to the Paramyxoviridae family, continues to be a leading cause of vaccine-preventable mortality worldwide, particularly in regions characterized by suboptimal immunization coverage (1). Prior to the introduction of vaccination, measles was responsible for cyclical epidemics occurring every 2 - 5 years, resulting in millions of fatalities annually (2). Although global vaccination initiatives have led to a 73% reduction in measles-related deaths since 2000, resurgence remains prevalent in areas with deficiencies in herd immunity, a situation exacerbated by vaccine hesitancy, logistical challenges, and declining seroprevalence (3).
In Iran, the measles vaccination program commenced in 1968, transitioning from an initial single-dose regimen administered at 9 months to a two-dose measles, mumps, and rubella (MMR) schedule at 9 and 15 months of age by 1988 (4, 5). In terms of national vaccination coverage, rates exceed 90%; however, localized outbreaks persist, particularly in southern provinces such as Hormozgan, where logistical challenges and transient populations impede consistent immunization efforts (6, 7). Notably, between 2004 and 2008, more than 4,300 suspected measles cases were reported nationwide, with southern regions, including Bandar Abbas, experiencing recurrent outbreaks attributed to declining herd immunity and the introduction of imported genotypes (8, 9).
The durability of vaccine-induced immunity is a significant concern. Research indicates that measles IgG antibodies may decrease over time, putting older children and adolescents at risk of infection despite being fully vaccinated (10). For example, Nokhodian et al. found that only 65.8% of Iranian students aged 7 - 18 years were seropositive, highlighting the potential for immunity gaps as children grow older (11). Furthermore, emerging evidence points to the impact of measles virus genotypes on antibody neutralization efficacy. The WHO recognizes eight clades with a total of 24 genotypes based on a C-terminal nucleotide of the N-gene sequence. Viruses with related sequences within a genotype (e.g., B3, H1) are considered as clusters (12). Among all recognized genotypes, D4, H1, and B3 have been detected regularly in different regions of Iran (13). Notably, the B3 genotype shows lower geometric mean titers (GMTs) compared to the D4 and H1 genotypes, which may compromise protection in areas where B3 is prevalent (14).
In Hormozgan province, a populated area with significant migration rates, measles outbreaks reported between 2009 and 2015 raised concerns about suboptimal immunity despite high vaccination coverage (15).
2. Objectives
This study aims to evaluate the measles-specific IgG seroprevalence in children aged 2 to 6 years — an essential period before antibody levels decline — and to assess associations with demographic factors. The findings will inform targeted interventions to maintain herd immunity and reduce the risk of outbreaks in vulnerable regions.
3. Methods
3.1. Study Design and Population
This cross-sectional study was conducted from January 2022 to December 2023 in Bandar Abbas, the capital city of Hormozgan province, southern Iran. The study population included 133 children aged 2 - 6 years who visited public medical centers (e.g., outpatient clinics, vaccination units, or pediatric wards) for routine check-ups, minor illnesses, or immunization. Children were excluded if they had a history of measles infection in the past six months, congenital immunodeficiency (other than those reported by parents during interviews), or if parental consent was not obtained. Participants were consecutively enrolled during their visits to ensure a representative sample of the pediatric population accessing healthcare services.
3.2. Data Collection
Trained healthcare staff conducted face-to-face interviews with parents/guardians using a standardized checklist. The checklist questionnaire captured:
(1) Demographics: Age (recorded in months and later categorized into < 5 years vs. ≥ 5 years), gender, and place of residence (urban/rural). All eligible samples were from Iranian individuals.
(2) Household characteristics: Number of family members and children under six years old.
(3) Nutritional history: Feeding practices during infancy, categorized as exclusive breastfeeding (≥ 6 months), formula-only, or mixed feeding (breast milk supplemented with formula).
(4) Immunization status: Verification of two-dose MMR vaccination via health records.
3.3. Laboratory Procedures
Venous blood samples (3 - 5 mL) were collected from each child and centrifuged at 3,000 rpm for 10 minutes to separate the serum. Sera were stored at -20°C until analysis. Measles-specific IgG antibodies were quantified using a commercial indirect ELISA kit (Euroimmun, Lübeck, Germany; Cat. No. EI 2662-9601 G) following the manufacturer’s protocol. The BP800 ELISA Reader (Biohit, Finland) measured optical density at 450 nm. Results were interpreted as follows:
(1) Negative: < 0.8 IU/mL (susceptible to measles)
(2) Borderline: 0.8 - 1.1 IU/mL (equivocal; retested for confirmation)
(3) Positive: > 1.1 IU/mL (immune)
The assay’s inter-and-intra-assay coefficients of variation were < 10%, ensuring reproducibility.
3.4. Statistical Analysis
Data were analyzed using SPSS v26 (IBM Corp., USA). Descriptive statistics summarized categorical variables as frequencies (%) and continuous variables as mean ± SD. The chi-square test (or Fisher’s exact test for small cell counts) was used to evaluate associations between IgG seropositivity (positive vs. negative/borderline) and demographic factors. Age was dichotomized (< 5 vs. ≥ 5 years) to assess trends in antibody persistence. A P-value < 0.05 indicated statistical significance.
3.5. Ethical Considerations
Ethical approval was obtained from the Hormozgan University of Medical Sciences (IR.HUMS.REC.1397.272). Written informed consent was secured from parents/guardians, emphasizing voluntary participation and the right to withdraw. Data were anonymized using unique identifiers, stored in password-protected files, and accessible only to the research team. No incentives were provided to participants to avoid coercion.
4. Results
A total of 133 children (70 boys and 63 girls) were included in the study. Baseline characteristics are summarized in Table 1. The majority of participants were urban residents. Regarding nutritional status, 68.4% were exclusively breastfed, 11.3% received only formula, and the remaining children were fed with both breast milk and formula. The mean age of the children was 4.26 ± 1.62 years (median: 4.0 years), and the average household size was 4.15 ± 0.9 members (median: 5.0 members).
| Characteristics | Values |
|---|---|
| Total participants | 133 children |
| Gender (male/female) | 70 (52.6)/63 (47.4) |
| Age | 4.26 ± 1.62 (y) |
| Urban residence | 93 (69.9) |
| Exclusive breastfeeding | 91 (68.4) |
| Formula-fed only | 15 (11.3) |
| Mixed feeding | 27 (20.3) |
| Household size | 4.15 ± 0.9 members |
a Values are expressed as mean ± SD or No. (%).
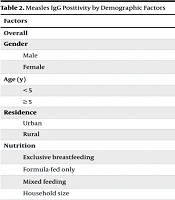
Table 2 presents the prevalence of IgG antibodies against measles based on baseline characteristics. Overall, 94.7% of children tested IgG seropositive for measles. The presence of measles IgG antibodies was not significantly associated with gender (P = 0.072), age (P = 0.653), place of residence (P = 0.109), nutritional method (P = 0.328), or household size (P = 0.390).
a Female IgG+ inferred from total IgG+ count (126/133) and male IgG+ (64/70).
b Exclusive breastfeeding and mixed feeding IgG+ assumed to align with overall prevalence (94.7%) due to non-significant P-value.
5. Discussion
This study found a measles IgG seroprevalence of 94.7% among children aged 2 - 6 years in Hormozgan province. These results align with previous Iranian studies, which reported post-vaccination immunity rates between 93.7% and 96.8% (5, 10). These findings suggest that the current vaccination program in this region is largely effective in conferring immunity to measles during early childhood. However, the high seroprevalence observed in this age group contrasts with studies in older populations, such as the work by Nokhodian et al., which found only 65.8% seropositivity among Iranian students aged 7 - 18 years (11). This discrepancy highlights the potential for waning immunity as children grow older, a phenomenon documented in other global studies as well (14, 16). For instance, Loo et al. demonstrated that measles seroprevalence declines significantly with age, particularly in individuals vaccinated at younger ages (10). These findings underscore the need to evaluate booster doses or revaccination strategies to maintain long-term immunity, especially in older children and adolescents.
The variability in measles seroprevalence across different regions and age groups may also be influenced by factors such as vaccination timing, socioeconomic conditions, and circulating measles virus genotypes. For example, studies have shown that the age at which the first dose of the measles vaccine is administered can significantly impact the durability of immunity. In Iran, the transition from a single-dose regimen at 9 months to a two-dose schedule at 9 and 15 months has likely contributed to the high seroprevalence observed in younger children (5, 6). However, in regions with delayed or incomplete vaccination coverage, lower seropositivity rates have been reported, emphasizing the need for robust immunization programs (3).
Interestingly, no significant associations were found between measles IgG seropositivity and demographic factors such as gender, age, place of residence, or nutritional status. This finding differs from other studies, such as Sanchez-Aleman et al., which reported higher seroprevalence in girls and smaller households (14). These differences may reflect variations in study populations, vaccination practices, or regional epidemiological factors. For instance, in regions with higher migration rates or lower healthcare access, demographic factors may play a more pronounced role in shaping immunity levels. Additionally, the limited age range of this study (2 - 6 years) may have precluded the detection of age-related trends in seropositivity, which have been observed in studies with broader age ranges (10, 11).
Another critical factor influencing measles immunity is the genetic diversity of circulating measles virus strains. Studies have shown that antibody neutralization efficacy can vary significantly depending on the measles genotype. For example, Fatemi Nasab et al. demonstrated that GMTs against the B3 genotype were notably lower compared to the D4 and H1 genotypes, suggesting that genotype-specific differences may compromise protection in regions where certain strains predominate (9). This highlights the importance of genotype surveillance in understanding regional immunity patterns and guiding vaccination strategies.
Although this study found high seroprevalence, persistent measles outbreaks in southern Iran — particularly in Hormozgan province — suggest additional contributing factors. Addressing gaps in vaccination coverage, monitoring immunity waning in older children, and improving surveillance of measles genotypes are critical steps for effective measles control. These could include gaps in vaccination coverage, particularly among transient or marginalized populations, as well as the potential for imported cases from neighboring regions with lower immunization rates (6, 7). Additionally, the role of maternal antibodies in conferring temporary immunity to infants, which may interfere with early vaccination, warrants further investigation (1).
5.1. Conclusions
In conclusion, this study demonstrates a high level of measles IgG seropositivity (94.7%) among children aged 2 - 6 years in Hormozgan province, reflecting the success of the current vaccination program in this region. However, the findings also highlight the need for continued vigilance, particularly in light of evidence suggesting waning immunity in older age groups and the potential impact of measles virus genotypes on antibody efficacy. Nationwide studies are essential to assess regional disparities in immunity and to identify populations at risk of measles outbreaks. Sustained monitoring, genotype surveillance, and the potential introduction of booster doses may be necessary to maintain herd immunity and achieve measles elimination in Iran.
5.2. Limitations
Several limitations should be considered when interpreting the results of this study:
(1) Geographical limitation: The study was conducted only in Hormozgan province, which limits the applicability of the findings to other regions of Iran or globally.
(2) Age restriction: The focus was solely on children aged 2 - 6 years, preventing analysis of immunity trends across broader age groups.
(3) Sample size: With only 133 participants, the study may lack the statistical power to detect subtle differences in immunity.
(4) Cross-sectional design: This design prevents the assessment of long-term immunity trends or changes in antibody levels over time.
(5) Lack of genotype analysis: The study did not investigate the role of different measles virus genotypes in immunity variation.
(6) Potential bias: Participants were recruited from medical centers, which could introduce selection bias and limit the generalizability of the findings.
5.3. Recommendations
Based on the findings and limitations of this study, the following recommendations are suggested:
(1) Expand research scope: Conduct studies across multiple provinces to evaluate regional variations in measles immunity.
(2) Broaden age range: Include older children, adolescents, and adults to assess immunity waning over time.
(3) Increase sample size: Use a larger participant pool to improve statistical reliability and detect demographic variations.
(4) Implement longitudinal studies: Monitor antibody levels over time to assess long-term vaccine effectiveness.
(5) Investigate measles genotypes: Analyze how different measles virus strains influence immunity and vaccine efficacy.
(6) Minimize selection bias: Use community-based sampling rather than medical center recruitment for a more representative study population.
(7) Address social determinants: Examine socioeconomic and healthcare access factors affecting vaccination coverage.
(8) Enhance public health strategies: Use findings to guide targeted vaccination campaigns in areas with lower immunity.