1. Introduction
Glomerulonephritis comprises a diverse group of disorders characterized by hematuria, proteinuria, hypertension, and varying degrees of impaired kidney function. It may occur as part of a multisystem disease, as a manifestation of malignancy or monoclonal gammopathy, or as a result of external factors such as infections or medications. Historically, the most common infectious cause of acute glomerulonephritis (AGN) has been group A beta-hemolytic Streptococcus infections. Post-streptococcal glomerulonephritis (PSGN) is the classic example of infection-related glomerulonephritis, primarily affecting children between 5 and 12 years of age. Two streptococcal antigens — nephritis-associated plasmin-like receptor and streptococcal exotoxin B — are recognized as key factors in the development of PSGN. Despite advances in healthcare, PSGN continues to be the most prevalent form of infection-related glomerulonephritis in children (1). The PSGN most frequently presents in children 1 to 2 weeks after a sore throat or 6 weeks after a skin infection (impetigo).
While PSGN represents a renal complication primarily following streptococcal infections of the throat or skin, severe infections in the head and neck region — such as retropharyngeal abscesses — can also pose significant systemic risks and may occasionally be associated with renal involvement. A retropharyngeal abscess is a serious infection involving the deep spaces of the neck, posing a potentially life-threatening condition in children. This anatomical space is situated between the anterior surface of the cervical vertebrae and the posterior wall of the esophagus and contains connective tissue and lymph nodes that receive lymphatic drainage from surrounding structures.
Approximately 50% of retropharyngeal abscess cases occur in children between the ages of 6 and 12 months, and 96% of all cases are reported in children under 6 years of age. This high prevalence in younger children is due to the typical atrophy of the lymph nodes of Rouviere, which drain the retropharyngeal space, after this age. The most commonly implicated pathogens include group A Streptococcus, anaerobic bacteria, and Staphylococcus aureus. Clinically, retropharyngeal abscesses present with symptoms such as fever, dysphagia, odynophagia, trismus, neck stiffness, and poor oral intake (2).
This case highlights the rare coexistence of PSGN with retropharyngeal abscess in an older child, expanding the clinical spectrum of PSGN triggers. It emphasizes the need to consider PSGN in children with acute kidney injury and deep neck infections beyond typical age groups, especially in those with underlying conditions like diabetes, to ensure timely diagnosis and treatment.
2. Case Presentation
A 12-year-old boy with a history of type 1 diabetes mellitus (DM1) presented to the emergency department at Mofid Children’s Hospital with a 3-day history of periorbital and peripheral edema. He denied having experienced similar symptoms in the past and reported symptoms of an upper respiratory infection (URI) occurring one week prior to the onset of edema. On initial evaluation, the patient was alert, developmentally appropriate, and appeared non-toxic. His weight was 42 kg, and vital signs were as follows: Heart rate 100 bpm, oxygen saturation 98% on room air, body temperature 37°C, and blood pressure 130/80 mmHg. Peripheral pulses were full and symmetric. The laboratory results are listed in Table 1. Physical examination revealed significant pitting edema (++), localized to the face and extremities. Neck examination showed bilateral cervical and submandibular lymphadenopathy, with multiple lymph nodes measuring up to 10 mm in diameter. These nodes were round, firm, mobile, and non-tender. Oropharyngeal examination demonstrated uvular deviation to the right and marked postnasal drip (PND). Cardiopulmonary examination revealed normal lung auscultation and a 2/6 systolic murmur on cardiac auscultation. Abdominal examination was notable for a soft and non-tender abdomen, with the spleen tip palpable and the liver non-palpable. No costovertebral angle tenderness was detected. Skin examination showed no rashes or lesions, and neurological and muscle tone assessments were unremarkable.
| Test | Result | Reference Range/Notes |
|---|---|---|
| Hb (g/dL) | 11.5 | - |
| WBC count (µL); % | 8700 | - |
| Neutrophils | 82 | - |
| Lymphocytes | 11.2 | - |
| Platelet count (µL) | 315,000 | - |
| BUN (mg/dL) | 21.7 | - |
| Cr (mg/dL) | 0.8 | - |
| ESR (mm/h) | 68 | Elevated |
| CRP (mg/dL) | 80 | Elevated |
| Alb (g/dL) | 3.7 | Normal |
| LDH | 406IU/L | Mildly elevated |
| Chol (mg/dL) | 125 | - |
| TG (mg/dL) | 65 | - |
| ComplementC3 (mg/dL) | < 20 | ↓ (Normal: 75 - 135) |
| Complement C4 (mg/dL) | 14 | Normal (9 - 36) |
| CH50 (mg/dL) | < 20 | ↓ |
| Urinalysis | ||
| Protein | 4+ | Nephrotic range |
| Blood | ++ | - |
| RBCs (per HPF) | 20 - 25 | - |
| Dysmorphic RBCs | Normal | - |
| Throat culture | Negative | - |
| ASO titer (IU/mL) | 800 | Elevated |
| Anti-dsDNA (IU/mL) | 195 | Positive (> 100) |
| 24-hour urine collection | ||
| Volume (cc) | 3600 | - |
| Protein (mg) | 1764 | Sub nephrotic |
| Creatinine (mg) | 785 | - |
| Blood culture | No growth | - |
| Immunoglobulins | Normal | - |
| Viral markers | Normal | - |
| Electrolytes | Normal | - |
Laboratory Results
Soft tissue ultrasonography revealed multiple enlarged lymph nodes bilaterally, with some showing necrotic changes [maximal short-axis diameter (SAD) = 10 mm]. There is evidence of fat inflammation and a 10 × 14 mm hypoechoic area in the left retropharyngeal region, suggesting a possible abscess. Abdominal sonography demonstrated that the liver has a normal size and a homogeneous echo-pattern. Both kidneys were of normal size, with preserved cortico-medullary echo patterns and differentiation. The spleen exhibited a normal echo pattern but was at the upper limit of normal size. However, abdominal and pelvic CT scans indicated mild splenomegaly (130 mm).
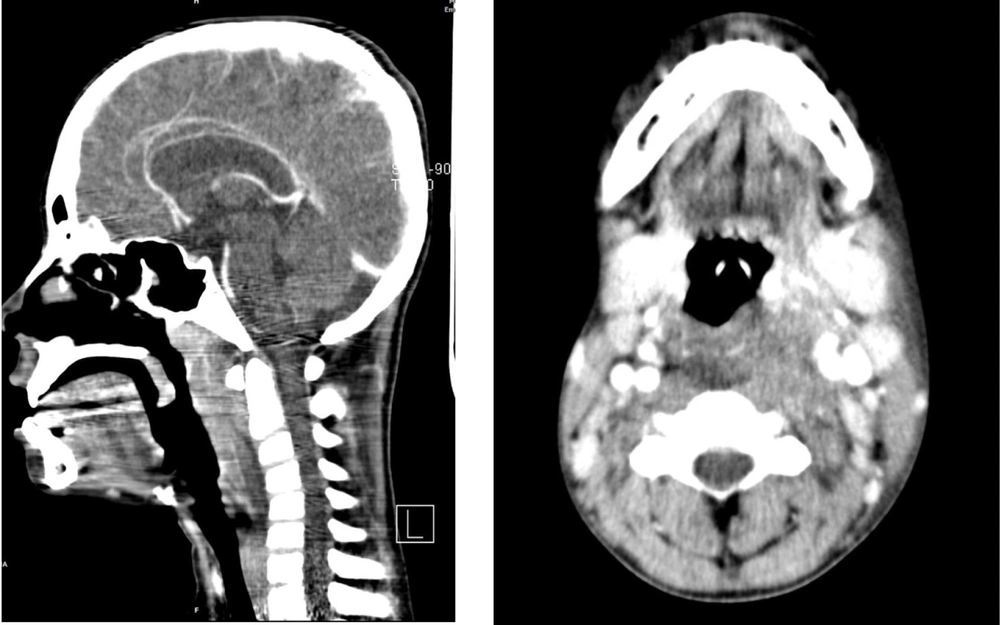
A spiral scan of the neck with IV contrast demonstrated a retropharyngeal abscess with retropharyngeal thickening, measuring approximately 60 × 32 × 12 mm, along with bilateral lymphadenopathy on both sides of the neck. The parapharyngeal, pre- and post-styloid, and mastication areas appear normal. There are no pathologic findings in the oral cavity, sublingual and submandibular spaces, and oropharynx. The palatine and lingual tonsils and soft palate are unremarkable. The epiglottis, vallecula, supraglottis, pyriform sinuses, aryepiglottic folds, larynx, and ventricles are normal. No evidence of lymphadenopathy was detected. However, multiple reactive lymph nodes up to 8 mm in the left anterior chain of cervical lymph nodes were noted in the cervical and submandibular regions.
Based on these evaluations, a preliminary diagnosis of PSGN was established, and supportive care, including benzathine penicillin G (intramuscular), was initiated as a single dose (1200 IU). Considering the patient's systolic blood pressure, which ranged from 130 to 140 mmHg, antihypertensive therapy was started, consisting of 20 mg furosemide every 12 hours (oral) and 25 mg losartan (oral) daily. Following the findings from the ultrasound and CT scan, a retropharyngeal abscess was suspected. After consulting with the infectious disease team, the patient was started on Clindamycin 400 mg every 6 hours (IV) and Ceftriaxone 1.5 g every 12 hours (IV). In light of the observed lymphadenopathy and splenomegaly, a hematology consult was requested, with infectious causes being considered as the likely underlying issue for the lymphadenopathy.
2.1. Soft Tissue Sonography
Multiple enlarged lymph nodes are noted bilaterally, with some exhibiting necrotic changes (MAX SAD = 10 mm). Signs of fat inflammation are present, along with a 10 × 14 mm hypoechoic area in the left retropharyngeal region, suggesting a possible abscess.
2.2. Spiral CT Scan of the Neck with IV Contrast
Findings indicate a retropharyngeal abscess accompanied by retropharyngeal thickening, measuring approximately 60 × 32 × 12 mm. Bilateral lymphadenopathy is evident on both sides of the neck (Figure 1).
3. Discussion
Post-infectious glomerulonephritis (PIGN) is an immune-mediated renal response triggered by group A streptococcal infections, typically occurring 1 - 2 weeks after throat infections and 4 - 6 weeks after skin infections. Severe infections, such as retropharyngeal abscesses presenting concurrently with clinical and serologic evidence of PIGN, have been rarely reported. This case emphasizes the uncommon association of retropharyngeal abscess with simultaneous PSGN, prompting clinicians to consider other potential infections causing glomerulonephritis (3). Acute nephritic syndrome following an infection is classified as PIGN, with PSGN being a subtype that specifically follows Streptococcus pyogenes infection. The diagnostic criteria for PSGN include the sudden onset of hematuria, proteinuria, edema, and hypertension (4), along with serological evidence of streptococcal infection [such as elevated antistreptolysin O (ASO) titers or anti-DNase B titers] and reduced complement C3 levels, which generally return to normal within eight weeks. While most PIGN cases are preceded by pyoderma and occasionally respiratory tract infections, a study by IIyas and Tolaymat noted an epidemiological shift in PSGN, showing decreased incidence, milder severity, and a higher association with pharyngeal infections compared to skin infections (5).
The PSGN is triggered by streptococcal infections and results from either the glomerular deposition of circulating immune complexes (IgG, IgM, C3) or the direct binding of antibodies to antigens expressed within the glomerulus. Long-term renal complications, such as rapidly progressive glomerulonephritis due to crescentic glomerulonephritis, are rare (6). Indications for renal biopsy in children with PSGN include normal C3 levels, negative ASO titers, persistent renal failure, persistently low C3 levels for more than 6 - 8 weeks, and persistent hematuria. In this case, a biopsy was not necessary, as the clinical picture strongly supported PSGN, and no red flags suggesting alternative diagnoses or complications were present. Conventionally, PSGN is considered a non-suppurative complication of group A streptococcal infection (7). The concomitant occurrence of retropharyngeal abscess with PSGN is uncommon. Various causes of AGN in children include infectious (Streptococcus, Staphylococcus, Salmonella typhus, hepatitis B virus, cytomegalovirus, rubella, coxsackievirus, Epstein-Barr virus, and Plasmodium falciparum) and noninfectious causes (vasculitis, Henoch-Schönlein purpura, systemic lupus erythematosus, and polyarteritis nodosa) (8). Given the presence of a retropharyngeal abscess in our patient, along with a negative ANA titer and the absence of clinical signs suggestive of systemic vasculitis or collagen vascular disease, an infectious cause is the most likely explanation.
Retropharyngeal abscess is the second most common deep neck abscess in children after tonsillitis and is typically caused by beta-hemolytic Streptococcus, S. aureus, or, rarely, gram-negative organisms such as Haemophilus parainfluenzae (9).
Retropharyngeal abscesses are uncommon but potentially life-threatening infections that most often affect children under five years old, though they can occasionally occur in adults. Typically, these abscesses develop after a viral upper respiratory tract infection, but they may also arise following oropharyngeal trauma or dental issues. Additionally, risk factors include poor oral hygiene, diabetes, immunocompromised states, and low socioeconomic status.
It is noteworthy that cervical lymphadenopathy in our case could serve as a potential focus for the retropharyngeal abscess. The most common possible causes in our patient are uncontrolled diabetes and inadequate hygiene. However, aspiration of pus or drainage was not performed to identify the organism. Despite extensive searching, 20 to 50% of deep neck infections have no identifiable cause (10). Although a wide range of etiologies can cause PIGN in children, the most common cause remains streptococcal infection of the anterior pharynx in PIGN, which is not common among those over the age of six (4).
In this case, the diagnosis of PIGN — specifically PSGN — was established based on the clinical presentation and supporting laboratory findings, including:
A. Recent infection history: Upper respiratory tract infection one week prior and concurrent retropharyngeal abscess.
B. Nephritic syndrome: Sudden onset of edema, hypertension, hematuria, and proteinuria.
C. Laboratory evidence of streptococcal infection: Elevated ASO titer (800 IU/mL), positive anti-dsDNA in the absence of systemic lupus features.
D. Complement levels: Low serum C3 and CH50 levels (typical of PSGN), with normal C4.
E. Urinalysis: Hematuria with dysmorphic RBCs, proteinuria (4+), and 24-hour protein excretion of 1764 mg.
F. No features suggesting other systemic diseases: Negative ANA, no signs of vasculitis or SLE.
3.1. Conclusions
The PSGN typically occurs 1 - 2 weeks following a throat infection. This case underscores the unusual concurrence of a severe throat infection (retropharyngeal abscess) with AGN. This prompts the physician to look for other infections that may cause acute AGN in children. Although retropharyngeal abscesses typically manifest in children aged under 6 years old, we reported a rare case of retropharyngeal abscess beyond the typical age range.