1. Background
A novel coronavirus, identified in December 2019 in Wuhan, China (Hubei province), was officially named SARS-CoV-2 by the World Health Organization (1). The virus has spread worldwide, causing a global pandemic and raising significant concerns regarding its short- and long-term health consequences. SARS-CoV-2 infects cells via the angiotensin-converting enzyme (ACE2) receptor, which is abundantly expressed in alveolar cells, cardiac myocytes, vascular endothelium, and possibly central nervous system tissues (2, 3). The clinical manifestations of COVID-19 vary widely, ranging from mild upper respiratory symptoms to severe pneumonia and acute respiratory distress syndrome (ARDS). Beyond pulmonary injury, SARS-CoV-2 may affect multiple organs, including the brain, via inflammatory and thrombotic mechanisms (4, 5). Neurological manifestations include confusion, memory impairment, anosmia, encephalitis, seizures, and stroke (6-8).
Vertically transmitted COVID-19 from mother to fetus is considered rare; however, maternal infection and the associated immune responses may interfere with fetal brain development (9-11). Previous viral infections in utero, such as influenza and other coronaviruses, have been implicated in neuropsychiatric disorders. However, pinpointing the precise developmental risks associated with maternal SARS-CoV-2 infection has remained challenging (12). Furthermore, stressors associated with the pandemic, such as maternal anxiety, quarantine-related psychosocial factors, and disrupted health services, could impact neonatal outcomes. Observational data suggest that infants born during the pandemic may exhibit lower scores in certain neurodevelopmental domains (e.g., gross motor, fine motor, and social-personal) at 6 months, independent of actual SARS-CoV-2 exposure (13). Other studies have identified associations specifically with the severity of maternal infection, reporting that neonates born to symptomatic mothers tend to have lower Ages and Stages Questionnaire (ASQ)-3 scores (14).
Neonatal sepsis remains a leading cause of morbidity and mortality worldwide, affecting approximately 3 million newborns annually, with a mortality rate ranging from 11% to 19% (15). Despite modern advances, neonatal sepsis can have profound consequences on neurodevelopment, particularly in preterm infants. The mechanisms involved include direct inflammatory injury to the white matter, hypoxic-ischemic insults, and the release of cytokines that disrupt normal brain maturation (16, 17). Late-onset sepsis has been associated with adverse neurodevelopmental outcomes, including cerebral palsy and cognitive deficits (18).
2. Objectives
Given the overlapping concerns of emerging evidence suggesting potential neurodevelopmental challenges in neonates infected with COVID-19 and the established link between neonatal sepsis and neurodevelopmental sequelae, our study aimed to compare the developmental trajectories of infants with COVID-19 to those with sepsis during the first 24 months of life. By selecting these groups, we aimed to elucidate whether COVID-19 poses similar risks as sepsis, thereby enhancing the clinical understanding of the neurodevelopmental impact of these conditions and informing future monitoring and intervention strategies.
3. Methods
3.1. Study Design and Setting
We conducted a prospective cohort study involving infants with confirmed sepsis and SARS-CoV-2 infection in the NICU of the Children’s Medical Center, Tehran University of Medical Sciences, from March 2020 to March 2023. This tertiary center has served as a major referral facility for both sepsis and COVID-19 throughout the pandemic.
3.2. Inclusion Criteria
- COVID-19 group (case): Infants under 3 months of age with polymerase chain reaction (PCR)-confirmed SARS-CoV-2 and clinical signs of infection without positive bacterial or fungal culture. Infants with co-infections (COVID-19 and bacterial or fungal sepsis) were excluded.
- Sepsis group (control): Infants under 3 months of age with sepsis, defined by either a positive blood culture (proven sepsis) or the presence of clinical and laboratory criteria (clinical sepsis) as per NHS guidelines. The NHS guidelines (19) include clinical signs such as respiratory distress, temperature instability, and feeding problems, as well as laboratory findings including elevated C-reactive protein (CRP), abnormal complete blood count (CBC) with neutrophil counts, and/or positive cultures.
- Infants with major congenital anomalies, meningitis, pathologic jaundice, early onset sepsis (EOS), hypoxic-ischemic encephalopathy (HIE), structural brain abnormalities, and inborn errors of metabolism were excluded from both groups.
- Both term and preterm infants were included in the study, provided they met the specified criteria.
- All SARS-CoV-2 PCR-positive and proven sepsis infants were included, regardless of disease severity. The Pishtaz Teb kit (98001) was used for PCR. The BACTEC culture medium was used for blood cultures.
Early onset sepsis refers to infections occurring in neonates within the first 7 days of life.
Pathologic jaundice refers to jaundice that develops on the first day of birth or if the total serum bilirubin level rises by more than 5 mg/dL per day or is higher than 17 mg/dL.
3.3. Follow-up and Neurodevelopmental Assessments
All enrolled infants were followed up, and neurodevelopmental assessments were conducted for 6 to 24 months. The outcomes were evaluated at a single time point (between 6 and 24 months) using the Ages and Stages Questionnaire, Third Edition (ASQ-3). The ASQ-3 is a developmental screening tool used to assess the developmental progress of children from birth. It helps identify children who may need further evaluation or early intervention. The ASQ-3 evaluates five domains through a questionnaire:
1. Communication (cut-off: Approximately 27.93)
2. Gross motor (cut-off: Approximately 30.68)
3. Fine motor (cut-off: Approximately 35.39)
4. Problem-solving (cut-off: Approximately 16.71)
5. Personal-social (cut-off thresholds vary by age; average approximately 32 - 35)
The questionnaire was completed by the parents in the presence and with the guidance of the researcher, question by question. Scores falling below these cut-offs in any domain indicate the need for further intervention and possibly a formal developmental evaluation.
3.4. Data Collection
The investigator-prepared checklist included baseline variables, neurodevelopmental outcomes, and potential confounding factors, collected by trained professionals.
- Baseline variables: Gestational age, birth weight, sex, Apgar scores, and clinical course (including duration of respiratory support, length of NICU stay, and treatments administered).
- Neurodevelopmental outcomes: ASQ-3 scores in each domain.
- Potential confounders: Prematurity (gestational age < 37 weeks), need for mechanical ventilation, birth weight, hospital stay, and presence of hemodynamic instability.
3.5. Statistical Analysis
- Descriptive statistics: Means ± standard deviations (SD) for normally distributed continuous variables, or medians (interquartile ranges) for non-normally distributed continuous variables; frequencies and percentages for categorical variables.
- Comparisons of ASQs: A t-test was used to compare the ASQ scores of infants of the same age (months).
- Covariates: Multivariate analyses were adjusted for known risk factors, including gestational age, birth weight, hospital stay, and respiratory support.
- Significance threshold: P < 0.05.
4. Results
4.1. Demographic Characteristics
This prospective cohort study included 59 infants with confirmed sepsis and 52 infants with COVID-19 admitted to the Children’s Medical Center NICU between March 2020 and March 2023. A total of 111 infants were enrolled. Table 1 summarizes the baseline demographics of the COVID-19 and sepsis groups (categorized as proven sepsis and clinical sepsis). A small subset of participants (n = 9) was preterm (< 37 weeks), with 6 in the COVID-19 group and 3 in the sepsis group.
| Variables | COVID-19 (n = 52) | Proven Sepsis (n = 11) | Clinical Sepsis (n = 48) | P-Value |
|---|---|---|---|---|
| Gestational age (wk) | 37.75 ± 1.63 | 38.00 ± 1.70 | 38.01 ± 1.42 | 0.51 |
| BW (g) | 3195 ± 578 | 3100 ± 338 | 3250 ± 590 | 0.21 |
| Male (%) | 28 (53.8) | 7 (63.6) | 26 (54.2) | 0.83 |
4.2. Neurodevelopmental Outcomes
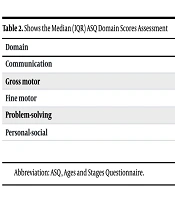
Table 2 illustrates the median ASQ domain scores assessment.
| Domain | COVID-19 | Sepsis | P-Value |
|---|---|---|---|
| Communication | 47.5 (25) | 50 (15) | 0.032 |
| Gross motor | 50 (10) | 60 (10) | 0.020 |
| Fine motor | 50 (15) | 50 (5) | 0.710 |
| Problem-solving | 60 (10) | 50 (25) | 0.190 |
| Personal-social | 60 (10) | 50 (10) | 0.170 |
Abbreviation: ASQ, Ages and Stages Questionnaire.
4.2.1. Communication
Infants in the COVID-19 group exhibited significantly lower median scores than those in the sepsis group (P < 0.05). However, the median scores for both groups remained above the clinical cut-off of 27.93, indicating that, despite the observed between-group differences, all infants scored within the "monitor" or "normal" range.
4.2.2. Gross Motor Skills
The COVID-19 group exhibited significant delays (P < 0.05). The median age for achieving independent sitting and walking was notably delayed in this group (for walking at 18 months in COVID-19 vs. 14 months in sepsis; log-rank P = 0.015).
4.2.3. Fine Motor & Problem-Solving
No statistically significant differences were observed (P > 0.05). Both groups achieved median scores that exceeded the established cut-off points (35.39 for fine motor skills and 16.71 for problem-solving skills).
4.2.4. Personal-Social Skills
There were no significant differences between the groups, and the median scores for both groups were above the domain-specific cut-off points.
Despite the statistical difference in communication and gross motor domain scores, all children in the COVID-19 and sepsis groups remained at or above the ASQ "monitor" threshold. However, the observed gaps between the groups indicated a heightened risk of delay in the COVID-19 cohort.
4.3. Subgroup Analyses: Prematurity, Sex, Prolonged Hospitalization, Birth Weight, and Respiratory Support Requirement
4.3.1. Sex
There was no statistically significant difference in sex distribution between the groups (P = 0.83). ASQ scores did not significantly differ between the two groups based on sex (P = 0.09).
4.3.2. Birth Weight
No significant difference in birth weight was observed between groups (P = 0.21). Additionally, ASQ scores for infants with birth weights less than 2.5 kg showed no significant difference between groups (P = 0.62).
4.3.3. Prematurity
Among 9 preterm infants, those in the COVID-19 group (n = 6) had slightly lower communication scores and showed a trend toward greater deficits in gross motor skills compared to the sepsis group (n = 3), although this difference was not statistically significant (P > 0.05).
4.3.4. Hospital Stay
Among 7 infants requiring >14 days of NICU admission, those in the COVID-19 group (n = 2) had nonsignificantly lower ASQ scores in communication and gross motor domains compared to the sepsis group (n = 5) (P > 0.05).
4.3.5. Respiratory Support
Among 13 infants who required mechanical ventilation, both groups exhibited lower ASQ scores. The COVID-19 group (n = 3) had nonsignificantly lower scores in communication and gross motor areas compared to the sepsis group (n = 10) (P > 0.05).
Due to the limited sample size, the statistical analyses of prematurity, hospital stay, and respiratory support were underpowered. However, trends suggested poorer developmental outcomes in the COVID-19 subgroup, possibly due to more severe pulmonary involvement and systemic inflammation.
5. Discussion
5.1. Linking COVID-19 Exposure to Neurodevelopmental Outcomes
Our findings align with those of several emerging studies reporting subtle but significant differences in neurodevelopment among infants exposed to SARS-CoV-2. Our study revealed deficits in communication and gross motor domains in the COVID-19 group, even after adjusting for birth weight and gestational age. These observations echo those of several recent investigations. Kim et al. found that very-low-birth-weight infants born during the pandemic had lower scores in language and gross motor domains compared to historical (pre-pandemic) controls (20). Shuffery et al. observed that infants born during the COVID-19 pandemic, regardless of maternal infection status, scored lower in gross and fine motor skills than pre-pandemic cohorts (21). Huang et al. noted higher risks of fine motor and communication delays in one-year-olds during the pandemic period, highlighting the possible impact of pandemic-related social restrictions (22).
Our study, however, differs in that we compared COVID-19 PCR-positive infants to a sepsis control group, rather than historical or healthy controls. Sepsis itself predisposes neonates to adverse neurodevelopmental outcomes (15-17). Thus, the observation of more pronounced deficits in COVID-19 infants, even against a high-risk comparator, reinforces the hypothesis that SARS-CoV-2 infection may pose unique or additional risks.
5.2. Mechanisms of Neurodevelopmental Delay
Potential mechanisms linking SARS-CoV-2 exposure to neurodevelopmental delays in infants include:
5.2.1. Direct Viral Invasion or Neurotropism
While vertical transmission of SARS-CoV-2 is rare, some neonates may acquire the virus during the perinatal period. The virus has been associated with neuroinflammation and endothelial damage, leading to microvascular injury in the brain (6, 9, 11).
5.2.2. Maternal Immune Activation
Even in the absence of vertical transmission, maternal inflammatory cytokines can cross the placenta and significantly alter fetal brain development (9, 12, 18).
5.2.3. Postnatal Inflammation
Neonates who experience severe COVID-19 may undergo systemic inflammation, commonly referred to as a cytokine storm, as well as hypoxemia. These conditions can be detrimental to the development of white matter tracts and neuronal architecture (8).
5.2.4. Indirect Effects of the Pandemic
The broader impacts of the pandemic, including lockdowns, reduced caregiving resources, increased parental stress, altered mother-infant bonding, and decreased access to early therapeutic interventions, may also contribute to developmental delays (14, 23, 24).
5.2.5. Sepsis and Similar Pathways of Neurological Injury
The developmental profile of the sepsis group was consistent with the existing literature, indicating that bacterial infections and the associated systemic inflammatory response can disrupt white matter myelination and synaptogenesis (17, 24). However, the COVID-19 group exhibited even lower scores in the communication and gross motor development domains, where infection-driven inflammation and environmental factors (such as isolation practices) may intersect. This follow-up study is particularly important given that other studies have noted that COVID-19 manifestations in infants tend to be milder than in adults (25, 26). Therefore, any infection in an infant, regardless of its severity, is significant. Parents must be aware of the potential long-term outcomes, emphasizing the need for preventive measures, especially during the neonatal period.
5.3. Limitations
This study has several limitations, including its single-center design, which restricts the generalizability of the findings, a relatively small sample size of the subgroups, and limited follow-up time. There is also incomplete data on maternal factors, such as the severity of maternal COVID-19, maternal health, and inflammatory markers. Future research involving larger multicenter cohorts that incorporate detailed inflammatory markers, extended follow-up time, and comprehensive maternal data will be essential to elucidate causal mechanisms and refine clinical guidelines.
5.4. Conclusions
Our prospective cohort study highlights significant neurodevelopmental outcomes among infants with COVID-19 compared with those with sepsis, specifically in the domains of communication and gross motor skills. While most infants in both groups scored within the "monitor" or "normal" ranges, the COVID-19 cohort exhibited notable delays, indicating a heightened risk for long-term developmental challenges. Given the importance of long-term follow-up, the studied cohort will continue to be followed, and the results will be published. These findings suggest that SARS-CoV-2 infection may introduce unique risks that extend beyond those associated with sepsis, potentially linked to direct viral effects and broader environmental disruptions during the pandemic. Future research with larger, multicenter cohorts and comprehensive maternal data is crucial for elucidating the causal mechanisms behind these observed neurodevelopmental delays and for developing targeted preventive strategies during the neonatal period.