1. Background
Tuberculosis (TB) is a human disease which is still a major cause of morbidity and mortality throughout the world, especially in Asia and Africa, and has remained a public health problem (1). It is the second leading cause of death in the world after HIV, according to the World Health Organization (WHO) estimates, in 2010 there were 8.8 million new cases of TB and 1.5 million deaths (2). While the incidence rate of TB in Iran is 28 per 100 000, its prevalence in Zahedan (Center of Sistan and Baluchistan province) has been higher than other regions of the country (3). More than one-third of the world’s population is infected with Mycobacterium tuberculosis, of which only 10% develop clinical disease; the remaining individuals are able to restrict and eliminate the infection by generating an appropriate immune response (4). Increasing evidence indicates that host genetic factors are important risk factors for development of TB and contribute to variations in the host response against M. tuberculosis (4, 5). Multiple genes may be involved in the development of susceptibility or immunity to TB. A variety of cytokines takes part in protective host response in human TB and also serves to localize the bacteria.
The CXCL10 gene localizes on chromosome 4 at band q21 (6). CXCL10 (IP10) is a small chemokine secreted by several cell types in response to interferon-γ (IFN-γ). These cell types include monocytes, endothelial cells and fibroblasts. It is a 10-kDa protein and is functionally categorized as an inflammatory chemokine. CXCL10 exerts its biological effects by binding to CXCR3 and regulates immune responses by activation of leukocytes such as T cells, eosinophils, monocytes, and natural killer (NK) cells. Several roles, such as chemoattraction of monocytes/macrophages, T cells, NK cells, and dendritic cells, promotion of T cell adhesion to endothelial cells, antitumor activity, and angiogenesis have been attributed to CXCL10. The role of CXCL10 has been discovered in various infectious diseases. It has been proposed that impaired CXCL10 production leads to susceptibility to infection (6).
Several genes contributing to TB susceptibility have been identified (1, 7). In our previous study, we found that single nucleotide polymorphism (SNP) in the IFN-γ gene was associated with susceptibility to TB (5). There is little information regarding the possible association between CXCL10 polymorphism and TB (8).
2. Objectives
The present study aimed to evaluate the association between CXCL-10 (-135 G/A) variant and pulmonary TB (PTB) in a sample of an Iranian population.
3. Patients and Methods
From September 2010 to June 2012, 150 patients with PTB, referred to the Research Center for Infectious Diseases and Tropical Medicine, Bou-Ali Hospital, Zahedan, Iran, and 150 population-based healthy subjects with no clinical symptoms or family histories of TB belonging to same ethnicity as patients were enrolled in this case control study.
Diagnosis of TB was based on clinical symptoms, radiological evidence, sputum acid fast bacillus (AFB) smear positivity, culture, and response to antituberculosis chemotherapy, as described previously (9). The local Ethics Committee of Zahedan University of Medical Sciences approved the study; all the individuals included in the study were informed about the study and written consents were obtained from them.
Two milliliters of venous blood was drawn from each subject. Blood samples were collected in EDTA-coated vials and stored at -20°C until DNA extraction. Genomic DNA was extracted using salting out method, as described previously (10).
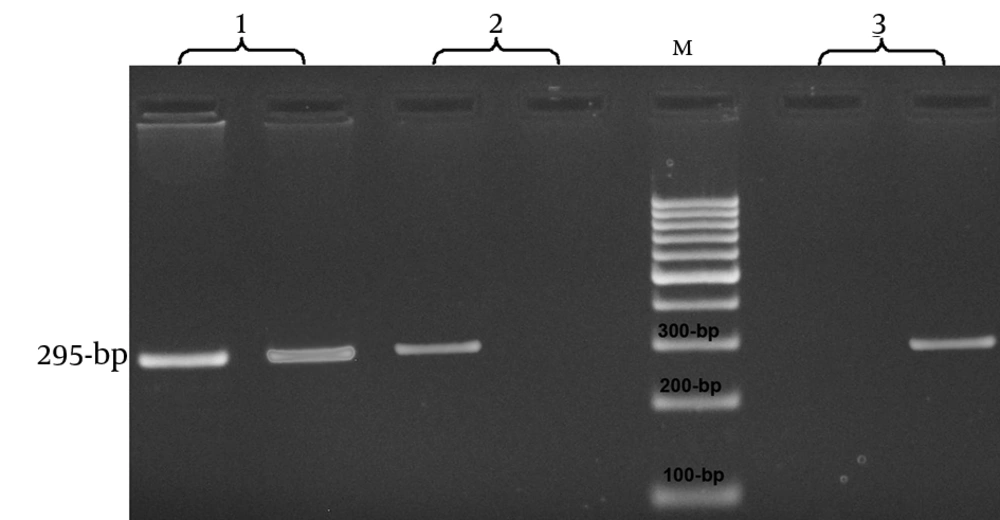
CXCL10 genomic sequence (NC-000004.11) was obtained from the National Center for Biotechnology Information (NCBI) (http://www.ncbi.nlm.nih.gov). The polymorphism was searched and primers for amplification refractory mutational system-polymerase chain reaction (ARMS-PCR) were designed (F: TTCCTTACCTTGAATGCCACTT, R (G Allele): GGAGGCTACAATAAATAATACCTTCG, R (A Allele): GGAGGCTACAATAAATAATACCTTCA). The product size was 295 base pair (bp). PCR was performed using a commercially available PCR premix (AccuPower PCR Pre-Mix, BIONEER, Daejeon, South Korea) according to the manufacturer’s recommended protocol. For the reaction mixture, 1 μL of the template DNA (~ 100 ng/μL), 1 μL of each primer (10 μM), and 15 μL DNase-free water were added to a 0.2-mL PCR tube containing AccuPower PCR Pre-Mix. The PCR cycling condition for detection of -135 G/A polymorphism of CXCL10 was as follows: five minutes at 95°C, followed by 30 cycles of 30 seconds at 95°C, 30 seconds at 62°C, and 17 seconds at 72°C, with a final extension of five minutes at 72°C. The PCR products were visualized and analyzed by electrophoresis in 2% agarose gel. A 100-bp DNA ladder marker was used as the molecular size standards (Figure 1). We regenotyped approximately 10% of the samples to verify the initial results, which confirmed the previous results by 100%.
3.1. Statistical Analysis
Statistical analysis of the data was performed using the SPSS 18.0 software. Demographics and biochemical parameters between the groups were analyzed by independent sample t-test for continuous data, and χ2 test was used to compare allele and genotype distribution in patients with TB and healthy controls. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated with logistic regression analyses.
4. Results
This study included 150 patients with PTB (55 males and 95 females) and 150 healthy controls (62 males and 88 females) belonging to same ethnicities. The mean age of patients with PTB and controls was 49.97 ± 20.98 and 44.87 ± 15.47, respectively. Table 1 summarizes the genotype and allele frequencies of the examined polymorphism in promoter region of the CXCL10 gene. There were significant differences in the genotype and allele frequencies of the CXCL10 gene -135 G/A polymorphism between the groups (χ2 = 27.36, P < 0.0001). As shown in Table 1, GA and AA genotypes were protective against TB (OR = 0.19, 95% CI = 0.10-0.36, P < 0.001 for GA vs. GG; OR = 0.12, 95% CI = 0.04-0.43, P = 0.001 for AA vs. GG; and OR = 0.18, 95% CI = 0.10-0.35, P < 0.001 for AG + AA vs. GG, respectively). Furthermore, A allele decreased the risk of TB (OR = 0.55, 95% CI = 0.39-0.77, P < 0.001) in comparison with G allele. We calculated the Hardy-Weinberg equilibrium (HWE) in cases and controls. We found that neither cases nor controls were in HWE (P < 0.05).
| Polymorphism | PTB | Normal | OR (95% CI) c | P Value |
|---|---|---|---|---|
| Genotype | ||||
| GG | 54 (36) | 16 (10) | 1.00 | - |
| GA | 91 (61) | 124 (83) | 0.19 (0.10-0.36) | < 0.001 |
| AA | 5 (3) | 10 (7) | 0.12 (0.04-0.43) | < 0.001 |
| GA + AA | 96 (64) | 134 (90) | 0.18 (0.10-0.35) | < 0.001 |
| Alleles | ||||
| G | 199 (66.3) | 156 (52) | 1.00 | - |
| A | 101 (33.7) | 144 (48) | 0.55 (0.39-0.77) | < 0.001 |
aAbbreviations: CI, confidence interval; OR, odds ratio; PTB, pulmonary tuberculosis.
bData are presented as No. (%).
cAdjusted for sex and age.
5. Discussion
Our findings revealed the protective role of CXCL10 -135 G/A polymorphism against PTB in our population. The frequencies of -135AG and AA genotypes as well as -135 A allele were significantly higher in normal subjects than ones with PTB. In agreement with our study, Tang et al. (8) showed that the minor allele of -135 G/A was a protective allele for TB in a Chinese population, but -1447 A/G and -872 G/A did not show any association with TB. They found that 14-bp adjacent to this SNP was a binding site for the nuclear factor (NF) κB. They postulated that this SNP (-135 G/A) may also affect the transactivation effect of NF-κB on the CXCL10 expression. Deng et al. (11) in a study on Han Chinese hepatitis B virus (HBV) carriers identified that the -201 G/A polymorphism in CXCL10 was associated with susceptibility to disease progression in male HBV carriers. They observed that the disease-susceptible genotypes, -201 GA and -201 AA, had higher CXCL10 transcription levels in IFN-g-stimulated peripheral blood mononuclear cells, compared with the -201 GG genotype. They revealed that the -201 GA polymorphism alters the binding affinity of the nuclear protein and regulates the CXCL10 expression. In a study on patients with invasive aspergillosis after allogeneic stem cell transplantation, Mezger et al. (12) found that three SNPs in CXCL10 (rs1554013, rs3921, and rs425767415) were associated with the occurrence of invasive aspergillosis. Nakata et al. (13) in a cohort study on 652 patients who underwent unrelated human leukocyte antigen (HLA)-matched bone marrow transplantation for hematologic malignancies, examined the impact of an SNP (rs3921) in the CXCL10 gene on the transplant outcomes. They showed that the recipient CG or GG genotype was associated with a significantly better five-year overall survival rate as well as lower transplant-related mortality rate than the recipient CC genotype. The recipient CG or GG genotype also predicted a reduced incidence of death due to organ failure. They declared that CXCL10 genotyping could be useful in prognoses and creating therapeutic strategies for improving the final outcomes of patients who undergo allogeneic marrow transplantation.
Function of the immune system against TB is homing, recruitment, migration and activation of leucocytes to sites of inflammation, besides restriction of M. tuberculosis to the site of infection by “granuloma formation”, which is regulated by TNFα and chemokines such as CCL2, CCL3, CCL5, CXCL8, CXCL9 and CXCL10 (14). CXCL10 is a chemokine, detected within tuberculous granuloma. CXCL10 attracts activated T cells and monocytes to the inflammatory area, promotes T helper (Th)-1 responses, and has antimicrobial functions (15). In addition to its chemotactic properties for immune cells, including monocytes/macrophages, CXCL10 is also involved in stimulation of NK cells and migration of T cells, following M. tuberculosis infection (16). Ruhwald et al. (17) found that IP-10 is expressed in very high amounts in patients with active TB, but not in unexposed controls. Liu et al. (6) demonstrated that alterations in CXCL10 expression levels were associated with inflammatory diseases including infectious diseases, immune dysfunction, and tumor development. Strong evidence has supported a critical role for genetic factors in susceptibility and resistance to TB, involving multiple genes of the innate immune system (16). Polymorphisms in cytokine genes are known to influence cytokine levels and may be associated with outcomes of infections (18). Indeed, polymorphism in -135 G/A CXCL10 can have a protective role against PTB. It is supposed that this polymorphism can influence the expression of the gene (8, 11).
One limitation of our study was the relatively-small sample sizes. There was no clear explanation for deviation from HWE in our population. It might be due to genetic drift as well as consanguineous marriages, which are still very common in Sistan and Baluchestan province. The -135 G/A regulatory polymorphism in the CXCL10 gene promoter could be a part of the genetic variation underlying the individuals' protections against TB in a sample of the Iranian population, which remains to be fully cleared.