1. Background
Calcium (Ca) and phosphorus (P) are the principal constituents of bone, and they comprise 65% of its weight. Vitamin D (Vit D) is characterized as a Ca homeostatic agent, known to have pleiotropic actions, and can play roles in decreasing the risk of many chronic illnesses including common cancers, autoimmune, infectious, and cardiovascular disease (1). The clinical syndrome of Vit D deficiency may be a result of deficient production of Vit D in the skin, lack of dietary intake, accelerated losses of Vit D, impaired Vit D activation or resistance to the biologic effects of 1,25(OH)2D (1,25-dihydroxyvitamin D)(2). Accelerated Vit D inactivation metabolites can be observed with drugs that induce hepatic cytochrome P450 mixed function oxidase, such as barbiturates, phenytoin, and rifampin. Impaired 25-hydroxylation, associated with severe liver disease or isoniazid usage, is another infrequent cause of Vit D deficiency (3).
Isoniazid and rifampin, which are the most important drugs in tuberculosis (TB) treatment affected Vit D metabolism and were used together in treatment of TB for many months, therefore Vit D level may change in serums of patients treated with anti-TB therapy. For these reasons Ca levels were studied in Indian patients during 18 months of treatment for TB with rifampin and isoniazid but no significant difference was observed (P > 0.1), which indicated that when rifampin is simultaneously taken with isoniazid it has no significant effect on Ca metabolism over an 18-month treatment period (4). Another study also concluded that the combined effects of isoniazid and rifampin did not cause clinically significant derangement of Vit D metabolism in patients undergoing a nine-month treatment period for TB (5), but none of these studies evaluated parathormone (PTH) or albumin (Alb) levels. On the other hand, it should be emphasized that multiple studies have shown high prevalence of Vit D deficiency in Asian countries. In Iran, results of a population based study to elucidate the prevalence of Vit D deficiency in Tehran on 1210 subjects showed a high rate of Vit D deficiency. Prevalence of severe, moderate and mild Vit D deficiency was 9.5%, 57.6% and 14.2%, respectively (6).
2. Objectives
In a region with a cold weather, high altitude, and low exposure to sunlight (Ardabil), with a high prevalence of Vit D deficiency, all components of Ca regulatory agents in the six-month period of standard anti-TB therapy were studied to determine how these drugs affect the metabolism of Vit D and Ca.
3. Patients and Methods
In the pilot study, eight adult patients whose pulmonary TB had been diagnosed with positive sputum test were selected for the study. All of the clinical states that may change normal bone metabolism state, such as renal insufficiency, HIV, diabetes, and menopause were excluded. For each patient Ca, P, Alb, ALP, Vit D (25 OH), and PTH levels were checked before and after the treatment, monthly until the course termination. Serum Vit D (25 OH) and PTH levels were measured by an electrochemiluminescence kit (Roche Diagnostics, Mannheim, Germany). The plan was approved by the ethics committee. Verbal informed consent was obtained from the patients, and they were free to leave the study at any time without any restrictions, and did not have to pay for the tests. Costs were paid by research deputy of the Ardabil University of Medical Sciences (ARUMS). Wilcoxon signed rank tests were used to compare mean differences and P < 0.05 was the level of significance.
4. Results
Eight patients, five males and three females, were evaluated serially. Serum creatinine and fasting blood glucose levels were in normal ranges in all of them. Means for hemoglobin and erythrocyte sedimentation rate (ESR) were 10.5 mg/dL 33.0 mm/h, respectively. The mean and standard deviation for serum levels of Ca and some other factors were shown in Table 1.
| Before Treatment, mo | After Treatment, mo | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
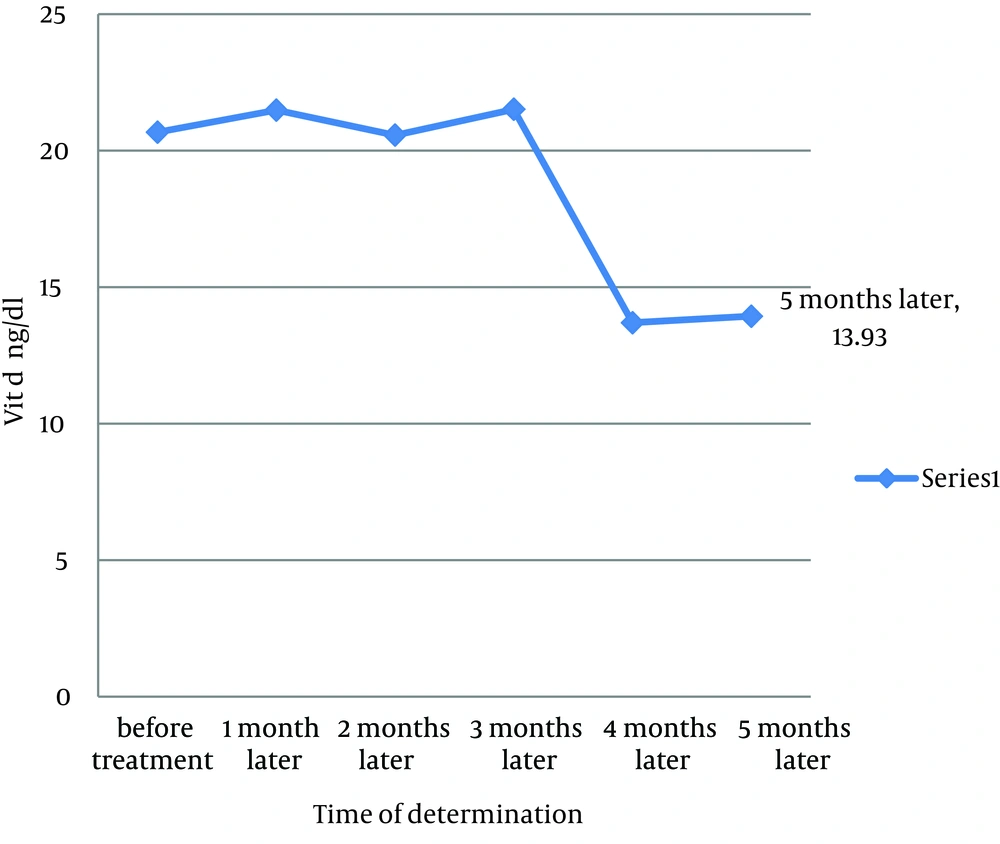
| Vit D, ng/mL | 20.67 ± 13.63 | 21.48 ± 19.4 | 20.56 ± 20.84 | 21.51 ± 21.17 | 13.69 ± 15.57 | 13.93 ± 18.75 |
| Ca, mg/dL | 8.78 ± 0.88 | 8.95 ± 0.56 | 8.73 ± 0.52 | 7.76 ± 0.49 | 8.96 ± 0.61 | 9.17 ± 0.5 |
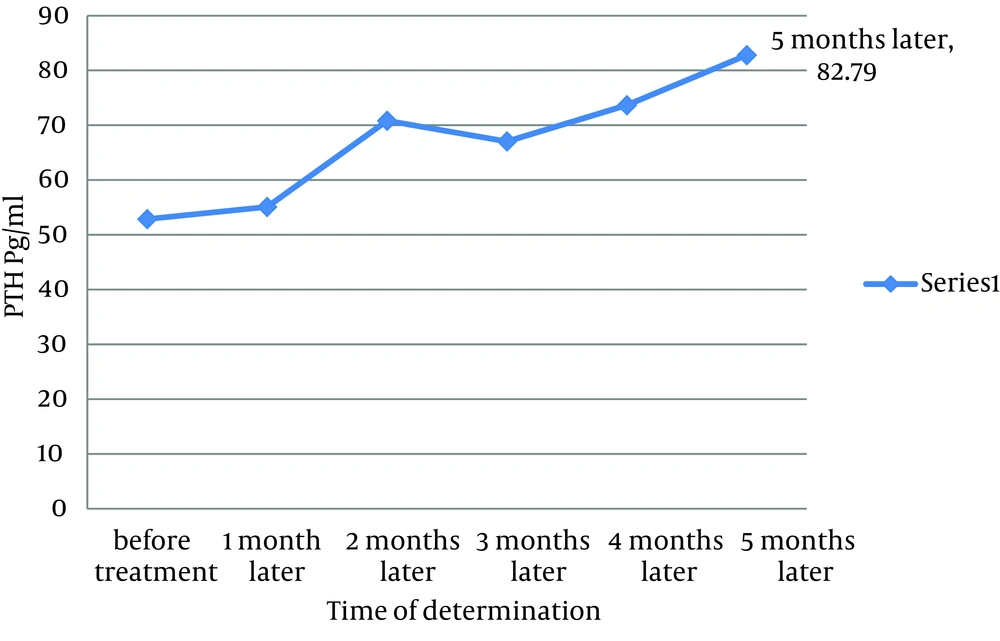
| PTH, pg/mL | 52.87 ± 28.32 | 55.09 ± 18.9 | 70.82 ± 50.49 | 67.04 ± 50.66 | 73.66 ± 48.16 | 82.79 ± 63.07 |
| ALP, IU/L | 257.88 ± 64 | 264.57 ± 67.13 | 267.62 ± 86.17 | 282.75 ± 104.07 | 274 ± 137.27 | 266.86 ± 107.47 |
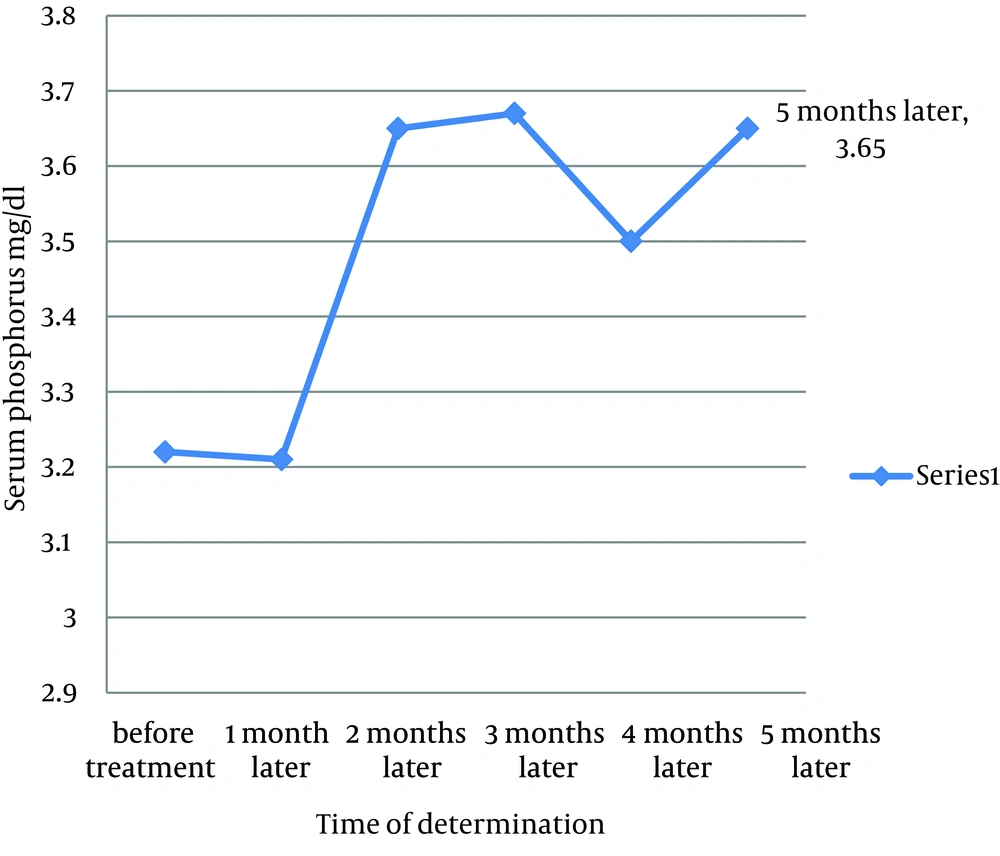
| P, mg/dL | 3.22 ± 0.73 | 3.21 ± 0.24 | 3.65 ± 0.72 | 3.67 ± 1.64 | 3.5 ± 0.6 | 3.65 ± 0.64 |
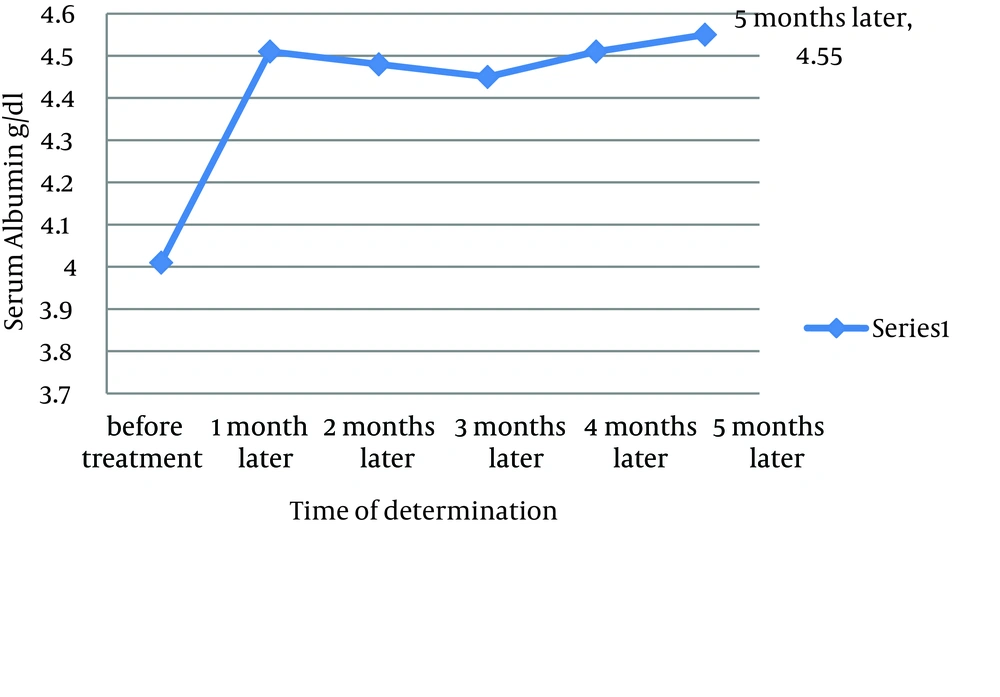
| Alb, g/dL | 4.01 ± 0.73 | 4.51 ± 0.32 | 4.48 ± 0.37 | 4.45 ± 0.33 | 4.51 ± 0.31 | 4.55 ± 0.31 |
aAbbreviations: Alb, albumin; ALP, alkaline phosphatase; Ca, calcium; P, phosphate; PTH, parathyroid hormone.
b Data are presented in Mean ± SD.
Vit D levels decreased significantly in the third month after starting the treatment (P < 0.05); but serum levels of Ca, alkaline phosphates (ALP) and phosphor did not change significantly. On the other hand, serum levels of Alb significantly increased in all five times of checking (P = 0.001). Serum levels of PTH increased, but not significantly, probably because of the wide standard deviation range.
5. Discussion
Rifampin with isoniazid decreased Vit D levels in serum, but serum PTH levels - increased to compensate for serum Ca maintenance. This maintenance of serum Ca levels in approximately constant levels was established at least partly with bone demineralization stimulated with PTH response (Figures 1-4).On the other hand serum Alb levels increased serially in favor of appetite improvement, and appetite improvement per se can compensate Ca and Vit D deficiency to some extent.
Some other studies have mentioned metabolic effects of isoniazid and rifampin in serum Ca levels. In a subject with a surgically proven hyperparathyroidism duo to parathyroid adenoma, anti-TB chemotherapy with rifampin and isoniazid temporarily resolved hypercalcaemia and hypercalciuria. The study demonstrated that anti-TB chemotherapy induces relative Vit D deficiency and resistance to PTH action, thereby masks hyperparathyroidism and hypercalcaemia (7). Sequential development of Vit D metabolites under isoniazid and rifampicin therapy studied by Toppet in a series of 46 children and a statistically significant decrease in 25-OH-D levels could be demonstrated after three months of treatment in one-third of them (13 cases). The study emphasized the need for regular biochemical supervision, even if no sign of rickets were observed in these patients (8). To assess the overall effect of rifampicin and isoniazid on Vit D metabolism, eight patients with TB were studied before, during and after nine months of treatment by Williams S. E. In eight healthy subjects, daily consumption of rifampin, 600 mg, and isoniazid, 300 mg for 14 days, reduced circulating levels of 25-hydroxyvitamin D (25-OHD) and 1 alpha,25-dihydroxyvitamin D (1,25(OH)2D) by 34% (P ˂ 0.01) and 23% (P ˂ 0.05), respectively. This was accompanied by a 57% rise in PTH (P ˂ 0.01), but not by deceleration in serum Ca or phosphate (P) levels (5). In the current study, levels of Vit D decreased and levels of PTH increased in serial measurements. At the same time serum Alb level increased significantly and it seems that appetite improvements after therapy have occurred. Appetite improvements and high Ca containing diets may compensate some consequences of Vit D deficiencies. On the other hand some studies have shown that low serum Vit D levels are associated with higher risk of active TB. In a cohort follow-up study from Pakistan, low Vit D levels were associated with progression to active TB in healthy household contacts, and low Vit D levels were associated with a five-fold increased risk for progression to TB (9). In another study, serum Vit D concentrations were measured before treatment in 178 patients with active TB and 130 healthy contacts (from the same ethnic and social background). There was a statistically significant difference in serum Vit D concentrations of the patients and contacts (20.1 vs. 30.8 nmol/L, 95% CI 7.1 to 14.3; P < 0.001) (10). According to a few concordant studies, available data were consistent with a bilateral relationship between Vit D and TB. Considering the decreasing levels of Vit D during anti-TB therapy, and protective effect of Vit D in TB development, it seems reasonable to monitor serum Ca, Vit D and parathormon levels in patients during anti- TB therapy especially in patients that Vit D deficiency is more probable such as children. Interventional studies with supplementary Vit D in the course of anti-TB therapy can clarify these issues in future.