1. Introduction
Mucormycosis is an important cause of infectious mortality in patients with predisposing factors such as uncontrolled diabetes or immunosuppression (1-3). Systemic antifungal therapy combined with surgical debridement and underlying disease control are the standards of care for invasive mucormycosis (4). Herein, we describe the successful management of extensive sino-orbital mucormycosis complicated by intracranial involvement in a diabetic patient.
2. Case Presentation
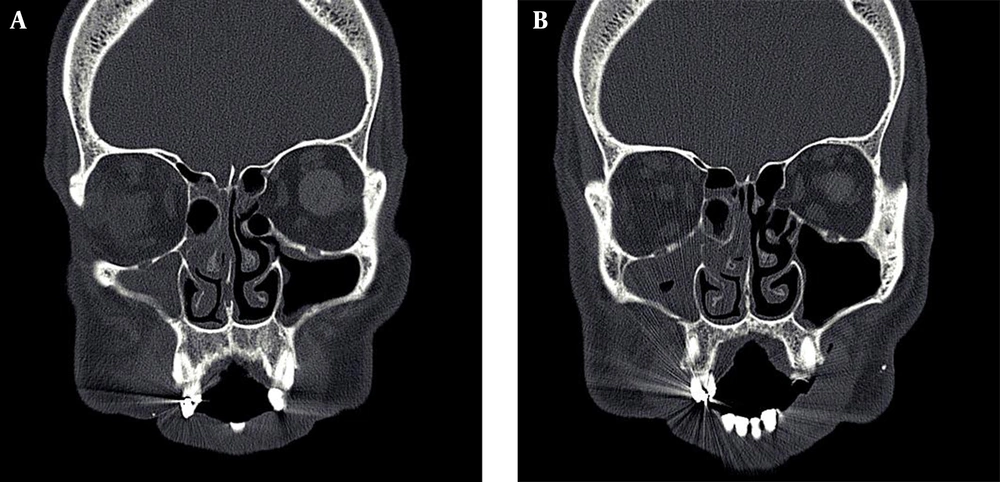
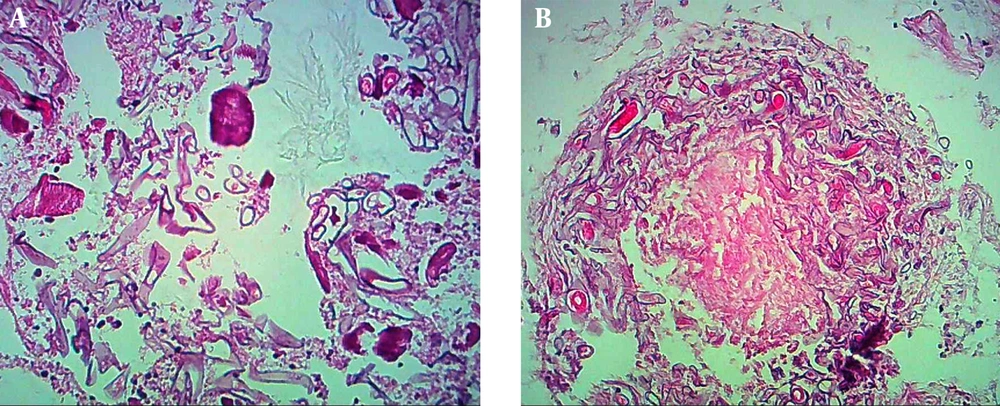
In July 2014, a 55-year-old Iranian man, a known case of uncontrolled diabetes mellitus, presented with fever, headache, right periorbital pain and swelling for the past two days. His left globe had been replaced by prosthetic device due to damage in the war since 30 years earlier. At the time of admission he was febrile (oral temperature: 38°C). No physical finding was detected on examination except for the right facial and periorbital swelling. Considering the clinical picture, a diagnosis of preseptal cellulitis was made and parenteral antibiotics were started in conjunction with insulin therapy. Relevant laboratory values on admission were as follows: total leukocyte count 19700 per mm3 with segmented neutrophil 87%, blood glucose 290 mg/dL, serum creatinine 1.4 mg/dL, and C-reactive protein (CRP) 20 mg/dL. Despite three days of treatment with intravenous antibiotics, fever persisted and he developed an obvious right sided proptosis accompanied by chemosis, ocular palsy, blindness and absence of pupillary response. Computed tomographic (CT) scan of paranasal sinuses showed total opacity of the right maxillary and ethmoid sinuses with extension to the right nasal cavity (Figure 1). At this time, CT scan of the brain was normal. Based on the history and clinical presentations, a provisional diagnosis of mucormycosis was made. Hence, intravenous amphotericin B deoxycholate (1.5 mg/kg/d) was initiated and ophthalmological consultation was requested. One day later, he underwent functional endoscopic sinus surgery and surgical debridement of all necrotic tissues was performed. In addition, tissue specimen was sent for histopathologic examination. Infusion of amphotericin B deoxycholate was complicated by a rise in serum creatinine level to 4 mg/dL; therefore, it was replaced by liposomal amphotericin B (L-AMB) with a dosage of 7 mg/kg/d. The histopathological report of sinus mucosal revealed invasive fungal infection with vascular thrombosis and infarction; there were foci of broadened hyphae with no septation in the necrotic vessel wall (Figure 2).
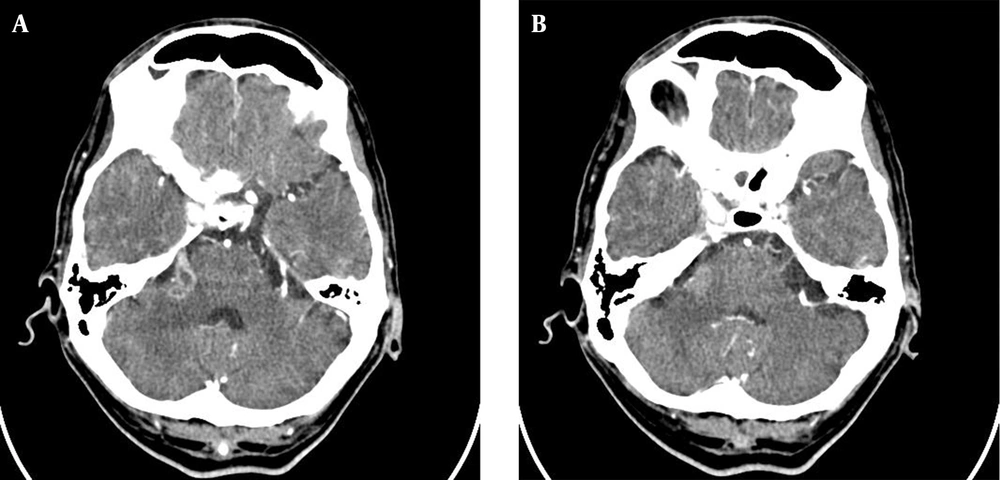
Based upon the above findings, a definite diagnosis of sino-orbital mucormycosis was given. Unexpectedly, despite the appropriate management, no improvement was observed after 15 days of L-AMB monotherapy and multiple sinus debridements; therefore, posaconazole 400 mg twice daily was added to L-AMB at the abovementioned dose. As a result of his optimal response to combined antifungal therapy, after six weeks, L-AMB was discontinued. At this time, biopsy of sinus tissue specimen was negative for evidence of active mucormycosis. After two weeks of monotherapy with posaconazole, the patient complained of severe headache and facial numbness. Considering the presence of the left globe prosthetic device, magnetic resonance imaging (MRI) was contraindicated practicality in this patient; hence, CT scan of the brain was performed and showed lobulated lesion with peripheral enhancement, overall measuring 21 × 11 mm in right cerebellopontine angle (CPA). Additionally, involvements of the right ophthalmic nerve and the cavernous sinus were revealed (Figure 3). Due to the occurrence of intracranial lesions while the patient was on posaconazole monotherapy, intravenous L-AMB 7 mg/kg/day was reintroduced in addition to oral posaconazole and consequently neurological symptoms disappeared after 10 days. Combination treatment was continued for a total of 42 days. A follow-up CT scan of the brain showed regression of his intracranial lesions. Therefore, the patient was discharged to continue maintenance therapy with posaconazole at home for at least another six months. At follow-up visits, the patient appeared to be in good health condition with no recurrence of symptoms.
3. Discussion
Mucormycosis is an opportunistic fungal infection, especially in immunocompromised patients (1-3). Additionally, as reported by the previous case series, diabetes is the most common risk factor among the immunocompetent population (5, 6). This fungal infection is characterized by a fulminant course and exceedingly high mortality rate. Certainly, an early recognition and management can lead to a better outcome (7). Invasive mucormycosis of the paranasal sinuses can easily invade the wall of blood vessels leading to cavernous sinus thrombosis, as was evident in our case. A definite diagnosis of mucormycosis is often done by histopathological identification of an organism; sinus cultures and blood cultures are rarely positive (8-10). The principals of management of this fatal infection are systemic antifungal therapy, aggressive surgical debridement and control of the underlying medical disease (4). Based on the published data, a high dose of L-AMB (5 - 10 mg/kg/day) is a first-line treatment for invasive mucormycosis (11). However, our patient showed poor response to amphotericin B monotherapy; thus, we decided to add posaconazole to the L-AMB treatment regimen. In some previous studies, the combination antifungal treatment with L-AMB plus posaconazole displayed synergistic in vitro activity (12, 13). Therefore, this combined regimen can be considered as an option after failure of appropriate first-line therapy (11). However, gaps in knowledge remain regarding the end point of treatment for sino-orbito-cerebral mucormycosis; based on the patient’s clinical responses, the length of antifungal treatment can be verified (7). We think, in our patient, prolong antifungal maintenance therapy was an important factor in survival.
In our patient, many factors affected the patient outcome. Early recognition, combination treatment with L-AMB plus posaconazole, multiple surgical debridement, and control of hyperglycemia led to recovery from invasive mucormycosis. Response failure to amphotericin B monotherapy and proper treatment with combined regimen were the prominent features in this case.
Finally, clinicians should be alert of the clinical presentation of this rapidly progressive fatal disease, since by rapid diagnosis and timely intervention they have the chance to increase the survival rate.