1. Introduction
Toxoplasma gondii is an apicomplexan protozoan parasite which is a highly successful global pathogen. T. gondii has the ability to infect any nucleated cell in any warm-blooded animal, including humans. Infection with T. gondii is typically acquired orally, through the ingestion of contaminated raw or undercooked meat containing cysts, or after ingestion of contaminated fresh water or vegetables (1). A key feature of T. gondii pathogenesis is the ability of the parasite to cross formidable biological barriers in the infected host and enter tissues such as the brain, eye, and placenta. Chronic asymptomatic infection affects 30% - 50% of the global population with host cells of the parasitic cyst located mainly in the central nervous system (2). Cerebral toxoplasmosis typically presents as cerebral mass lesions with headache, confusion, fever, lethargy, seizures, cranial nerve palsies, psychomotor changes, hemiparesis, and/or ataxia (3). Studies on patients with acquired toxoplasmosis that included immune-competent patients showed that the most common symptoms of cerebral toxoplasmosis were headaches and peripheral lymphadenopathy (4). This article presents a case of cerebral toxoplasmosis in a patient without AIDS or any history of immunodeficiency. The differential diagnosis of cerebral toxoplasmosis will be discussed.
2. Case Presentation
A 39-year-old woman presented to the emergency department of a teaching hospital in Tehran, Iran with complaints of headache, weakness, and pain in her neck that had persisted for the previous eight weeks. She had no focal weakness, numbness, or seizure activity. Her headaches were generalized mostly in the occipital and parietal lobes, and had a pulsatile character. There was no relief following positional changes or administration of paregoric. After a few days, she began to complain of nausea and dizziness, along with her other symptoms. After a while, she began to experience weakness in her left hand, which gradually spread to the whole left side of her body. It was revealed that she kept a cat in her house. She had been visited once by a neurologist who made the diagnosis of nervous headache. Her condition did not improve, so she went to another specialist who ordered a magnetic resonance imaging scan (MRI), which reported a mass.
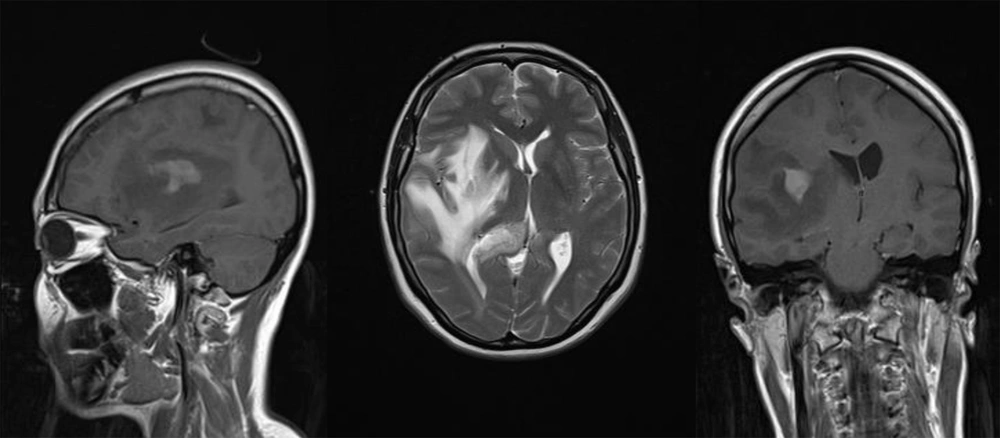
Gadolinium-enhanced MRI showed a small, well-enhanced, hyperintense signal lesion in the right temporoparietal region with significant mass effect and edema in the lobes. It was difficult to differentiate cerebral toxoplasmosis based solely on the MRI (Figure 1).
The following step was to perform a biopsy. It revealed inflammation in a chronic granulomatous lesion, compatible with tumefactive toxoplasmosis and right centrum semi-ovalae involvement. Ziehl-Neelsen (ZN) and periodic acid–Schiff (PAS) stains were negative for acid-fast bacilli and fungi, but gimsa staining demonstrated tachyzoites. Immunohistochemical (IHC) staining was positive for CD68 in hystocytes and for Glial fibrillary acidic protein (GFAP) in background proliferated glial cells, as well as for Leukocyte common antigen (LCA) in lymphoid cells. Chest X-ray and ultrasound of the abdomen were normal.
Laboratory investigations revealed a hemoglobin (Hb) of 12 g/dL, total white blood cell count (WBC) of 9.1 × 109/L, and platelet count of 253 × 109/L. The erythrocyte sedimentation rate (ESR) was noted to be elevated at 28 mm/1st hour. Serum electrolytes, blood sugar, renal parameters, and liver function tests were normal. Her CD4+ T cell, CD8+ T cell, and CD4/CD8 ratio were normal, and general biochemical investigations showed no abnormalities. The HIV antibody for HIV-1 and HIV viral load were negative, but Toxoplasma antibody test was positive. Toxoplasma serological tests, both IgG and IgM, were requested for the patient. Both tests were found to be strongly positive (IgG 98 IU/mL, reference positive range > 8 IU/mL; IgM 44 IU/mL, reference positive range > 10). Hepatitis B surface antigen (HBsAg), hepatitis B core antibody (HBcAb), and hepatitis C virus antibody (HCV Ab) tests were negative as well.
She was treated with Pyrimethamine 25 mg/TDS, sulfadiazine 500 mg/TDS, and folic acid 15 mg/TDS. She was discharged from the hospital in an ambulatory state.
3. Discussion
Toxoplasmosis is caused by infection with the obligate intracellular parasite T. gondii. Human latent toxoplasmosis occurs in as much as half the world’s population, though most cases are asymptomatic (5). With the advent of the human immunodeficiency virus (HIV) pandemic, cerebral toxoplasmosis has become one of the more frequent opportunistic infections and the most common cause of focal brain lesions complicating the course of AIDS (6). Human infection occurs through the oral or transplacental routes. The major clinical features of cerebral toxoplasmosis are headache, hemiparesis, speech disturbances, cerebellar dysfunction, and cranial nerve palsies (7).
Migraine and/or other types of headaches are a common concern affecting 5% and 10% of children and adolescents, respectively, as well as nearly 30% of reproductive-age women (8). Studies have shown that children with recurrent headaches are subject to an ever-increasing risk of such diseases in adulthood, as well as many physical symptoms and psychiatric disturbances, such as depression disorders (9). Studies involving immune-competent patients with acquired toxoplasmosis have revealed that the most common symptom of cerebral toxoplasmosis is headache; unfortunately, cerebral toxoplasmosis is not mentioned in textbooks or scientific papers as a cause of various types of headaches.
Cerebral toxoplasmosis is the reactivation of disease from a prior parasitic infection. Patients may present with fever, headache, seizures, confusion, dementia, or focal neurological deficits. Infection with T. gondii was considered in this patient when it was revealed that she had cats. She did not appear to have any evidence of immune depression. A brain biopsy was positive for toxoplasmosis. Neither computed tomography (CT) nor MRI scans can reliably distinguish CNS infections, such as toxoplasmosis (10). Cerebral toxoplasmosis was suspected from the high serum toxoplasma antibody level, and the patient went into remission with sulfadiazine (7). This case emphasizes the need to consider cerebral toxoplasmosis in immune-competent patients and, therefore, screening patients for toxoplasma infection is recommended.