1. Introduction
Hydatid disease, as an important zoonotic infection, has remained a major health problem in endemic areas; however, it could be seen all over the world (1).
Hydatid disease can involve any part of body, most commonly liver and lungs. Almost all pulmonary hydatid cysts may be ruptured (2), which could be hazardous in certain circumstances. The rupture of a pulmonary hydatid cyst can occur spontaneously particularly in larger cysts or secondary to an infectious process, chest trauma, coughing, and iatrogenic after needle aspiration. A variety of imaging modalities are used to help the diagnosis although unusual radiologic findings are not uncommon (3). Serological tests, in spite of their worthiness in diagnosis, are mostly not applicable in urgent situations. Therefore, the diagnosis is frequently made by a combination of clinical, laboratory, and radiological data. When the diagnosis is in doubt, a high level of clinical suspicion is needed to avoid diagnostic error. Here, we describe a case with a complicated pulmonary hydatid cyst that misdiagnosed as diaphragmatic hernia and its subsequent frightening complications.
2. Case Presentation
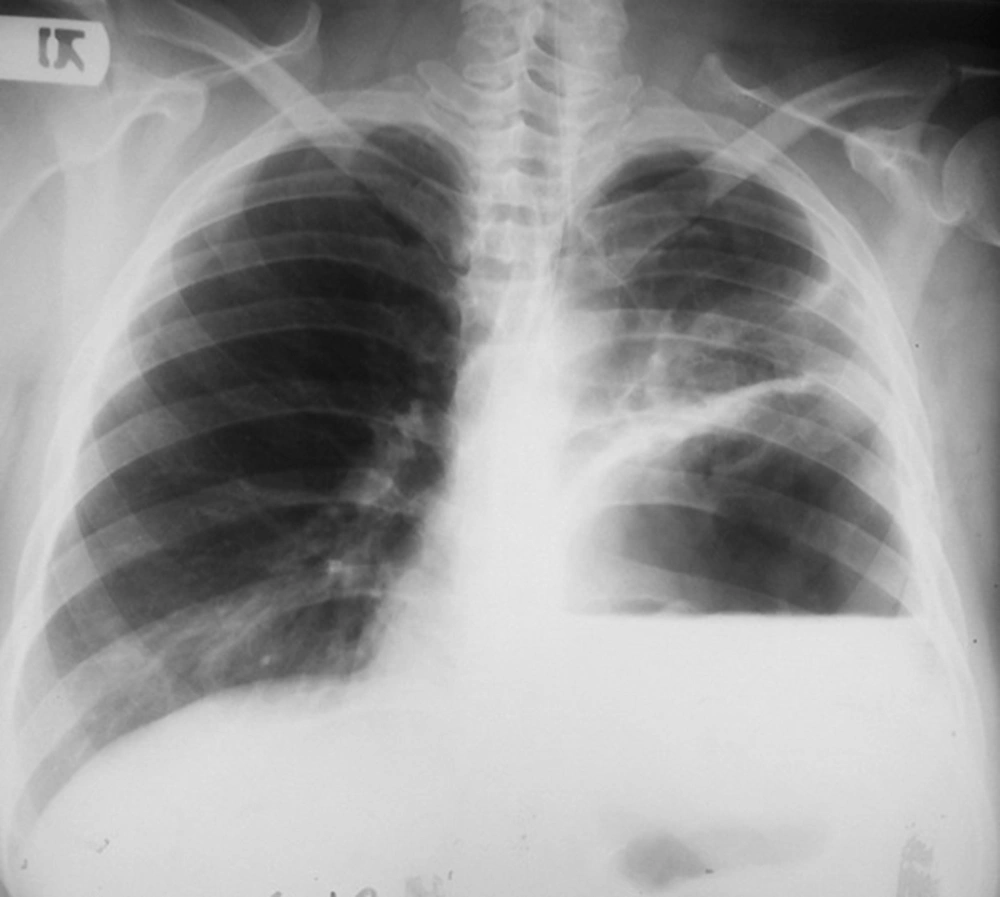
A 37-year-old woman developed an acute onset of the left sided upper abdominal and chest pain, vigorous vomiting, and dyspnea while driving for holiday. She was immediately referred to a medical center with limited facilities in a small town. A chest X-Ray was obtained (Figure 1) and a surgical consultation was made. Based on her clinical presentations and radiologic findings, the surgeon suspected a complicated large diaphragmatic hernia in the left side. There was no ability to achieve CT scan at that center. Due to deterioration of patient’s general condition despite resuscitation with IV fluids, she underwent a midline laparotomy with the diagnosis of a complicated left sided diaphragmatic hernia and potentially incarcerated/strangulated viscera. The diaphragm was intact without any sign of herniation. At this time, the patient developed a cardiovascular collapse and cardiac arrest. The surgeon immediately performed a left anterior thoracotomy in the 5th intercostal space. A large amount of air was escaped and after a few seconds of open cardiac massage, hemodynamics became stable. A large perforated hydatid cyst in the left lower lobe was diagnosed and a left lower lobectomy was performed. Because of continued air leakage of tube thoracostomies in post-operative days, the patient was referred to our tertiary referral center for thoracic diseases. She underwent the 2nd operation two weeks later with the diagnosis of bronchopleural fistula and empyema. A large bronchial opening was closed by interrupted 3/0 absorbable sutures and decortication was carried out. The post-operative course was uneventful.
3. Discussion
Despite recognition of etiology and the ways of prevention, echinococcosis is still a serious public health issue in certain parts of the world including Australia, South America, North Africa, Middle East and Mediterranean region (1, 4, 5). It seems it is the inevitable cost of living in sheep-raising areas of the world. The clinical picture of a pulmonary hydatid cyst generally depends on the size of the cyst and whether it is an intact cyst or a complicated one. While intact cysts could be asymptomatic and recognized incidentally in imaging modalities, nearly all complicated pulmonary cysts are symptomatic (3). Almost all pulmonary hydatid cysts could be complicated by rupture even small-sized lesions (2). The rate of rupture in pulmonary hydatid cysts has been reported as high as 60% and even more (6).
Rupture may give rise in anaphylaxis, asphyxia, and infection (7, 8). Hemoptysis, lung abscess formation, empyema, and hydropneumothorax are other possible consequences of a complicated lung cyst highly relevant to the site of perforation (9). Mostly, the rupture is to adjacent bronchi, so cough and dyspnea are amongst the most frequent symptoms of a complicated cyst. Once in a while, the patient may declare vomiting for expectoration of sour fluid and cyst contents (3). This statement besides a related radiographic feature may accurately confirm the diagnosis of a ruptured pulmonary hydatid cyst.
A variety of radiologic findings might be seen according to: size of the cyst, its location, the presence or absence of rupture or other types of complications (8). While some of them particularly water lily sign (floating membrane over cyst fluid) have been recognized as the characteristics of pulmonary hydatid cyst, imaging signs are generally just suggestive, supporting clinical data (3, 10). CT scan is the most useful diagnostic tool that is advised for all suspected cases (11). It may give further useful information regarding the cyst, its location, adjacent lung parenchyma, additional cysts in other lobes, contralateral lung or liver and associated complications. Pleural complications of a ruptured pulmonary hydatid cyst include: pneumothorax, pleural effusion, empyema, and disseminated pleural cysts (12). With acting as a check valve mechanism by a ruptured cyst, a simple pneumothorax could easily change to a life-threatening condition, tension pneumothorax (9).
Serology has traditionally been playing an important role in the diagnosis of echinococcosis. Nowadays, due to their low sensitivity and specificity, Cassoni intradermal test, complement fixation test (CFT), and indirect haemagglutination (IHA) test have been largely substituted by more reliable and accurate tests including: enzyme-linked immunosorbent assay (ELISA), indirect immunofluorescence antibody test (IFAT), and immunoblotting test (13). A major drawback for most serological assays is their time-consuming nature, making them impractical in urgent circumstances. Serology is more useful for follow-up of patients after surgical or pharmacological treatment.
As we described here in our case, regarding vomit-like complaint and weird x-ray findings, it is not impossible to misdiagnose a perforated hydatid cyst as diaphragmatic hernia particularly in the left side. As a matter of fact, delayed-onset diaphragmatic hernias (congenital or traumatic) make usually diagnostic challenges (14). It has not been uncommon to place a tube thoracostomy erroneously for a diaphragmatic hernia misdiagnosed as pleural effusion or pneumothorax (15, 16). Obtaining precise clinical history, conducting detailed physical examination, and applying proper diagnostic methods may discriminate these two conditions from each other more accurately. Sometimes, a simple adjunct test may confirm the definite diagnosis. Whenever the diagnosis of a complicated diaphragmatic hernia is suspected, early placement of a nasogastric tube could be of both diagnostic and therapeutic importance (17, 18). Misdiagnosing a ruptured pulmonary hydatid cyst as a complicated diaphragmatic hernia could be life-threatening because of serious morbidities and even mortality. A complicated diaphragmatic hernia prompts an urgent operation (mostly a laparotomy) due to the risk of strangulation of herniated viscera (19). Therefore, in cases of diagnostic errors, positive pressure ventilation during anesthesia can easily convert a simple perforated hydatid cyst or simple pneumothorax to a tension pneumothorax and its serious cardiovascular complications as occurred in our case. In cases of remaining debate in the diagnosis and inability to use more advanced imaging modalities, the use of some simple adjuncts would be of a great benefit. In the case described here, these terrible events might have been easily prohibited if a nasogastric tube had been placed preoperatively.
3.1. Conclusions
Pulmonary hydatid disease is keeping on to be a considerable health problem in endemic areas, affecting both sexes in all age groups. Yet, there is no a single laboratory or imaging test that could definitely confirm the diagnosis. A complicated pulmonary hydatid cyst in lower lobes may mimic a diaphragmatic hernia radiologically and have to be considered in suspected cases. A detailed clinical approach consisting of accurate history, physical examination, and proper radiologic studies will lead to a more accurate diagnosis preoperatively, making such hazardous misdiagnosis less frequent. Use of appropriate adjunct examinations may be helpful in clinically equivocal cases.