1. Literature Search
A literature search was done on Medline and EMBASE using relevant keywords like lipoglycopeptides, vancomycin, telavancin, dalbavancin, oritavancin, MRSA, VRSA, pneumonia, and skin infection in keywords, titles, or abstracts. Additional references were found from bibliographies of the selected papers. Relevant medical texts were checked when required. Randomized controlled trials and other types of studies were considered.
1.1. Structure
Glycopeptides have a common heptapeptide core, which enables them to inhibit the cell wall synthesis (1). The peptide backbone of glycopeptides forms the D-alanyl-D-alanine binding site that is important for their antimicrobial activities (2). Glycopeptides can bind to C-terminal D-alanyl-D-alanine (D-Ala-D-Ala) of cell wall precursor units and disrupt the polymerization of N-acetylglucosamine and N-acetylmuramic acid. Because of their large molecular size, they are unable to penetrate the outer membrane of Gram-negative bacteria (3). All three lipoglycopeptides contain lipophilic side chains, which prolong their half-lives and increase their activities against Gram-positive cocci (4). The length of the lipophilic side chain is important; an increase in the chain length increases the activity of the agent against enterococci but it reduces the activity against MRSA (5, 6). Dalbavancin is a semisynthetic derivative of teicoplanin. Modifications include the removal or substitution of sugars and derivatization of the functional groups such as the carboxy group of amino acid 7 (the C-terminus of the peptide), the N-terminus of the peptide, and different hydroxy groups. All modifications are at sites that do not directly affect the D-alanyl-D-alanine binding pocket (7). Oritavancin is a synthetic derivative of naturally occurring glycopeptides chloroeremomycin. N-alkyl-p-chlorophenyl benzyl substituent improves the activity of oritavancin against both vancomycin-susceptible enterococci (VSE) and VRE (8). Telavancin is a derivative of vancomycin. Unlike vancomycin, it has hydrophobic and hydrophilic moieties enabling it to be active against VRE and MRSA (9).
1.2. Mechanism of Action
In general, lipoglycopeptides are the inhibitors of the cell wall (10). Cell wall synthesis is impeded in a different way compared to beta-lactams. Lipoglycopeptides are linked with D-alanyl-D-alanine terminus of the peptidoglycan precursor binding to the C55 -lipid transporter (bactoprenol). The drug-amino acid complex effectively inhibits transglycosylase and thus the polymerization of N-acetyl muramic acid and N-acetyl glucosamine is impeded. The linear polymers must be cross-linked by transpeptidase to form a strong cell wall. In addition to the inhibition of transglycosylation, lipoglycopeptides are able to inhibit transpeptidation (11-13). Compared to vancomycin, oritavancin and telavancin exhibit a dual mechanism of action by the inhibition of transpeptidation. It has been shown that telavancin and oritavancin are more potent inhibitors of transpeptidase than vancomycin. Moreover, telavancin and oritavancin are able to disrupt the integrity of bacterial membrane and increase the permeability by the hydrophobic tail. Membrane destabilization by dalbavancin has not been shown yet (11, 14-16). Of note, unlike telavancin and dalbavancin, oritavancin has a unique property to inhibit D-alanyl-D -lactate in VRE and VRSA, which is of great importance in clinical practice. D -alanyl-D -lactate can reduce the binding affinity of vancomycin by 1000 times (17-19).
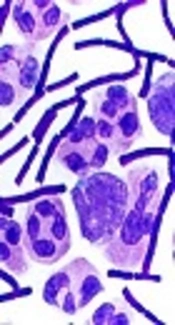
1.3. Microbiology
As stated, lipoglycopeptides are active against Gram-positive bacteria with varying efficacy (20). In general, they have a lower MIC than vancomycin against MRSA, VISA, VRSA, VISA, Staphylococcus epidermidis, vancomycin-susceptible enterococci (VSE), VRE, Streptococcus spp., and Clostriudium spp. (21). From a microbiological point of view, they have important differences; dalbavancin has an excellent activity against MRSA and VISA with a poor activity against VRE. Its effects against Clostridium spp. is comparable with that of vancomycin (22). Oritavancin has the widest spectrum against Gram-positives. Oritavancin is 16- to 32-fold more potent than vancomycin against MRSA. It displays a potent activity against VISA and VRE. Oritavancin has the lowest MIC against S. pneumonia and penicillin-resistant phenotypes (23). Like dalbavancin, telavancin displays a similar activity for MRSA and VISA with the lowest MIC against Clostridium spp. (24).
1.4. Indications
Compared to vancomycin, lipoglycopeptides are more potent and exhibit a faster bactericidal activity against important pathogens including MRSA, VRSA, and VRE. In addition to these benefits, they have longer half-lives affecting the frequency of administration, and perhaps the side effects (25, 26). Until date, several clinical trials have been performed to evaluate the efficacy and safety of lipoglycopeptides. At present, lipoglycopeptides are considered useful choices for the treatment of skin and skin structure infections. Of note, telavancin has been introduced as an alternative in the therapy of hospital-acquired pneumonia including ventilator-associated bacterial pneumonia caused by susceptible organisms (25-27). Dalbavancin is administered either at a one-dose regimen of 1500 mg IV or at a two-dose regimen of 1000 mg IV followed one week later by 500 mg IV. The infusion time is 30 minutes (28). Oritavancin is used as a single 1200 mg dose over three-hour IV infusion (29). Telavancin is given 10 mg/kg IV every day for 7 - 14 days. Its infusion time is one hour (30). Seltzer et al. performed an open-label, randomized, controlled, Phase II multi-center trial examining one-dose and two-dose dalbavancin versus standard-of-care therapy for the treatment of skin and soft tissue infection (SSTI) including vancomycin, cephalosporins, clindamycin, piperacillin-tazobactam, or linezolid. 20 patients were given a single 1500 mg intravenous dose of dalbavancin, 21 patients were given a 1000 mg dose of dalbavancin followed by a 500 mg dose 7 days later, and 21 patients were administrated the comparator therapy for 7 to 21 days (21 patients). On day 10 and day 20, and on the last day of treatment, the clinical response was examined for one-dose dalbavancin, two-dose dalbavancin and for the comparator regimens, respectively. The success rates were 75% (15 out of 20) for one-dose dalbavancin, 91% (19 out of 21) for two-dose dalbavancin, and 81% (17 out of 21) for the comparator therapy (31). In addition, Jauregui et al. compared dalbavancin and linezolid efficacy for the treatment of skin and skin structure infection. Dalbavancin group was composed of 571 patients receiving a 1000-mg dose on day one of therapy and a second dose of 500 mg on day 8. The linezolid group was composed of 283 patients receiving 600 mg twice daily for 14 days, with at least 24 hours of initial intravenous therapy. The clinical response was measured on day 14 (± 2 days). The success rates were 88.9% and 91.2%, respectively, for dalbavancin and linezolid groups. Two doses of dalbavancin were as effective and as well tolerated as twice daily doses of linezolid (32). A phase II, multicenter, randomized, double-blind, parallel group, active-comparator study named SIMPLIFI was conducted by Dunbar to evaluate the oritavancin efficacy for the treatment of complicated skin and skin structure infections (cSSSI). Treatment groups were daily (100 patients, 200 mg daily for 3 - 7 days), infrequent (103 patients, 800 mg on day 1 with an optional 400 mg on day 5), and single-dose (99 patients, 1200 mg a one-time dose) groups. The clinical response was measured on days 21 - 29, decided by the investigator. This investigation showed that the single dose of oritavancin was as efficacious as a daily dose and had a similar safety profile (33). Furthermore, the efficacy of a single dose of oritavancin and multi-doses of vancomycin were tested in two pivotal double-blind, randomized phase III studies, SOLO I and II; 1910 subjects with acute bacterial skin and skin structure infections (ABSSI) received a single 1200-mg dose of oritavancin or 1 g dose of vancomycin for 7 - 10 days. This study confirmed that oritavancin was non-inferior to vancomycin for the primary endpoint at early clinical evaluation (80.1% for oritavancin vs. 82.9% for vancomycin), the clinical cure endpoint at post-therapy evaluation (82.7% vs. 80.5%, respectively), and a ≥ 20% reduction in lesion size endpoint at early clinical evaluation (85.9% vs. 85.3%, respectively) (34, 35). Of note, the efficacy and safety of lipoglycopeptides have not been investigated in children, yet. For this reason, a phase I, multicenter, open-label, pharmacokinetics, safety, and tolerability study of oritavancin in pediatric patients who are younger than 18 years with suspected or confirmed Gram-positive bacterial infections is recruiting. Approximately, 48 patients will be enrolled at 10 - 15 centers in the United States. The starting dose will be IV oritavancin 15 mg/kg. The safety, tolerability, and PK data will be reviewed to determine the appropriate dose (36). Unlike oritavancin and dalbavancin, telavancin can be used as an alternative drug in pneumonia and in cSSSIs. In the ATTAIN study, two methodologically identical, double-blind studies were done in patients with hospital-acquired pneumonia (HAP) due to Gram-positive pathogens (37). 1503 patients received telavancin (10 mg/kg every 24 hours) or vancomycin (1 g every 12 hours) for 7 - 21 days. In the pooled clinically evaluable population, cure rates were 82.4% with telavancin and 80.7% with vancomycin. The adverse events were comparable between the treatment groups. The mortality rates for telavancin and vancomycin were 18.5% and 21.5%, respectively. Increases in serum creatinine levels were more common in the telavancin group (16% vs. 10%), which is important in patients with moderate to severe renal impairment. Overall, it was shown in the ATTAIN study that telavancin is non-inferior to vancomycin for treating HAP. In the ATLAS-1 and ATLAS-2 trials, two parallel, randomized, double-blind, active-control, phase 3 studies were performed in 1867 patients with complicated skin and skin-structure infections. Patients were given telavancin (10 mg/kg every 24 hours) or vancomycin (1 g every 12 hours). After the receipt of the last antibiotic dose, success was achieved as 88% in the telavancin group and 87% in the vancomycin group at 7 - 14 days after the last administration of drugs. Therapy discontinued because of adverse events in 8% and 6% of patients who received telavancin and vancomycin, respectively. Except for mild gastrointestinal upset and foamy urine in the telavancin group and pruritus in the vancomycin group, the adverse events were similar. This work demonstrated that telavancin given once daily is at least as effective as vancomycin for the treatment of patients with complicated skin and skin-structure infections, including those infected with MRSA (38, 39). Besides FDA approved indications, some new case reports have provided limited experiences in other situations caused by Gram-positive pathogens. A recent case study reported uselessness of four weeks of treatment with dalbavancin in a woman with infective endocarditis (40). In addition, an acceptable clinical response to oritavancin has been recently reported in a patient with osteomyelitis (41).
1.5. Safety
In general, lipoglycopeptides have acceptable safety profiles. The most frequently reported side effect is gastrointestinal upset. Of note, taste disturbance, nausea, and vomiting are more common than diarrhea (35-42). However, dalbavancin administration is associated with a higher rate of nausea and vomiting compared to dalbavancina and oritavancin. Another common side effect of telavancin is foamy urine that is not dangerous. Dizziness, pruritus, and rash are less common side effects seen with telavancin (43). Mild and reversible ototoxicity has been reported in a study (44). Reversible rises in creatinine levels and increases in QTC interval have been observed in FAST study (45). For this reason, co-administration of telavancin with drugs that can increase QTC interval should be avoided. Amiodarone, procainamide, disopyramide, sotalol, ibutilide, ondansetron, and cisapride are well-documented drugs associated with an increase in QTC interval (46). Telavancin should not be prescribed for patients with pre-existing moderate to severe renal impairment unless benefits outweigh the risks. Nausea, headache, and vomiting are the most common side effects seen with oritavancin use. In addition, a slight rise in hepatic transaminases, phlebitis, and tachycardia are rarely reported. Unlike telavancin, it does not need a dose adjustment in renal impairment. It is noteworthy that oritavancin is a weak inducer of CYP3A4 and CYP2D6 and a weak inhibitor of CYP2C9 and CYP2C12. The metabolism of carbamazepine, clonidine, and disopyramide are significantly reduced by concomitant administration of oritavancin. On the other hand, the levels of phenytoin, warfarin, and valproic acid will increase if they are used with oritavancin (45, 47). Dalbavancin has a lower rate of gastrointestinal problems compared to oritavancin and telavancin. Pyrexia and rash have been rarely seen. Unlike other lipoglycopeptides, dalbavancin is associated with hematotoxicity, in particular, leukopenia. Anemia, thrombocytopenia, and hemorrhage have been noticed very rarely in patients treated with dalbavancin. Reported cases of leukopenia have had spontaneous cure (48). Until date, no clinical interaction has been observed for dalbavancin either major or minor. Of note, the pregnancy category for all three lipoglycopeptides is C, and it is not documented whether they are distributed in milk.
2. Conclusions
In conclusion, dalbavancin, oritavancin, and telavancin offer important alternatives in skin infections. Dalbavancin is a promising agent in pneumonia. High quality clinical studies on the efficacy and safety in addition to clinical experience can promote them as preferred antibiotics against Gram-positive pathogens. They are welcome agents in other serious infections as add-on therapy.