1. Background
Asymptomatic bacteriuria is characterized by the isolation of a specific quantitative count of bacteria in the urine sample of an asymptomatic patient. In routine practice, screening for or treatment of asymptomatic bacteriuria in premenopausal, nonpregnant women is not recommended (1-3). Nevertheless, women with asymptomatic bacteriuria are more prone to symptomatic urinary tract infections (UTIs) (4).
The prevalence of asymptomatic bacteriuria in healthy women increases with age, ranging from about 1% among schoolgirls to more than 20% among women over 80 years in the community (1, 5, 6). Several studies have been previously published regarding the association of serum vitamin D level and recurrent UTI in premenopausal women (7). The association between vitamin D deficiency and increased risk of infection has been clearly addressed in the literature. Children with nutritional rickets are more susceptible to respiratory tract infections, leading to the coining of the phrase “rachitic lung” (8).
There is also a speculation that common virological infections have marked seasonal variations because of seasonal changes in vitamin D status (9, 10). There are several ongoing randomized trials to clarify the possible beneficial effects of vitamin D supplementation on infectious diseases (see National Institutes of Health and European Clinical Trial registries) (7). Several studies have demonstrated that immunological responses to Mycobacterium tuberculosis, the causative agent of tuberculosis, are augmented in individuals receiving higher levels of vitamin D (11, 12). Therefore, the potential role of vitamin D in the pathogenesis and immune responses to bacterial pathogens has been recently highlighted.
The significant role of vitamin D against bacterial infections through induction of antimicrobial proteins, such as cathelicidin and β-defensin, has been clearly addressed in the literature. Previous studies have demonstrated that women taking vitamin D supplements are more likely to produce cathelicidin, compared to the controls (13). Cathelicidin, induced by vitamin D, can potentially exert a local effect rather than a systemic one; this could help researchers design selective therapies against pathogens without perturbing commensal microbes elsewhere in the body.
According to previous studies, vitamin D insufficiency can potentially predispose patients to UTIs (7). Therefore, researchers hypothesized that vitamin D might play a significant role in the prevention of UTIs. The high incidence of symptomatic UTI has been reported among young sexually active women. In a university-based cohort study, the incidence of UTI was high, ranging from 0.5 to 0.7 episodes per person each year (14).
Furthermore, postmenopausal women are more susceptible to cystitis. In a prospective cohort study by Jackson et al., a total of 1017 postmenopausal women were enrolled and followed-up for 2 years; in this study, the culture results confirmed the diagnosis in 138 participants (15). The prevalence of low vitamin D level may be increasing globally (16-18). In a review of vitamin D level in different regions of the world, vitamin D levels below 30 ng/mL (75 nmol/L) were prevalent in every studied region. Low vitamin D levels (< 10 ng/mL; 25 nmol/L) were more common in South Asia and Middle East, compared to other regions (17).
Considering the growing antimicrobial resistance and potential progression of asymptomatic bacteriuria to frank UTI, vitamin D could play a major potential role in the prevention of UTI if there is an association between vitamin D deficiency and asymptomatic bacteriuria. To the best of our knowledge, this is the first study to examine the relationship between serum vitamin D level and asymptomatic bacteriuria in individuals, referred to a private laboratory for screening in Tehran, Iran.
2. Objectives
The aim of this study was to address any association between serum vitamin D level and asymptomatic bacteriuria in pre- and postmenopausal women.
3. Methods
3.1. Study Population
During 6 years, 65 pre- and postmenopausal women with asymptomatic bacteriuria were enrolled in the study. Negaresh pathobiology laboratory in Tehran was the reference laboratory. The serum concentration of 25(OH)D was analyzed quantitatively via direct competitive and fully automated enzyme-linked immunosorbent assay (ELISA), using EUROIMMUN 25-OH Vitamin D (Medizinische Labordiagnostika AG). The EUROIMMUN 25-OH Vitamin D ELISA assay consists of an ELISA microwell plate, coated with monoclonal anti-25(OH)D antibodies. This kit has been designed for in vitro analysis of 25(OH)D in human serum or plasma samples.
Subjects with asymptomatic bacteriuria were compared to 65 age-matched women with no asymptomatic bacteriuria (control group) in terms of serum 25(OH) vitamin D level. The exclusion criteria were as follows: 1) diabetes mellitus; 2) pregnancy; 3) chronic renal failure (creatinine clearance test < 30 ml/min); 3) HIV, HBV, or HCV infection; 4) rheumatic disorders; 5) spinal cord injuries; 6) indwelling urinary catheter; 7) history of urologic surgery (e.g., urinary tract stent and nephrostomy tube); 8) urinary incontinence; 9) history of vesicoureteral reflux; 10) neurogenic bladder; 11) congenital urinary tract abnormalities; 12) renal stones; 13) gynecological problems; 14) organ transplant; 15) chronic use of immunosuppressive agents; 16) antibiotic use within the last 3 months; 17) vitamin D supplementation; and 18) substance abuse. The control group consisted of eligible pre- and postmenopausal women with negative urine culture. All the participants were of the same racial background.
3.2. Definitions
Vitamin D sufficiency was defined as 25(OH) vitamin D level of 30 - 100 ng/mL, insufficiency was defined as 10 – 30 ng/mL, and deficiency as < 10 ng/mL. Diagnosis of asymptomatic bacteriuria was confirmed if a specific quantitative count of bacteria (105) was isolated from appropriately collected urine samples of an asymptomatic patient.
3.3. Study Design
The medical records of pre- and postmenopausal women, referred for screening tests during 2011 - 2016, were retrospectively reviewed. We compared the groups of pre- and postmenopausal women with and without asymptomatic bacteriuria in terms of serum 25(OH) vitamin D level. The study protocol was in accordance with the ethical guidelines of declaration of Helsinki (1975) (19).
3.4. Statistical Analysis
The data were analyzed using SPSS version 20 (IBM, New York, USA). Kolmogorov–Smirnov test was performed to evaluate the normal distribution of data. Data are presented as mean ± SD if normally distributed and median (range) if not. Independent sample T-Test was used to investigate the differences in serum vitamin D level between the groups.
4. Results
A total of 200 medical records were evaluated in this study. After excluding records with missing data or other exclusion criteria, 65 pre- and postmenopausal women with asymptomatic bacteriuria were enrolled in the study. Cases with asymptomatic bacteriuria were compared to 65 age-matched women without asymptomatic bacteriuria (control group) in terms of serum 25(OH) vitamin D level.
The mean age of women with asymptomatic bacteriuria was 38.8 ± 14 years, and the mean age of the controls was 40.6 ± 13 years. The mean serum 25(OH)D3 level was 28.8 ± 10 ng/mL among women with asymptomatic bacteriuria and 50.3 ± 9 ng/mL among the controls (Table 1). Based on the findings, the serum levels of 25(OH)D3 were significantly lower in patients with asymptomatic bacteriuria, compared to women without asymptomatic bacteriuria (P < 0.001).
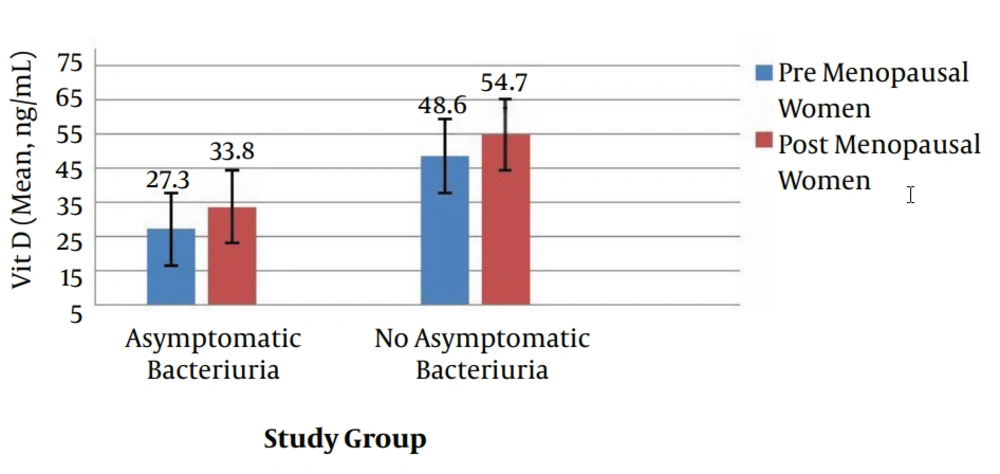
In the study group, the mean serum level of 25(OH)D3 was 33.8 ± 10 ng/mL among postmenopausal women with asymptomatic bacteriuria and 54.7 ± 8 ng/mL among postmenopausal women without asymptomatic bacteriuria (Figure 1). Therefore, the serum level of 25(OH)D3 was significantly lower in postmenopausal women with asymptomatic bacteriuria, compared to the corresponding group without asymptomatic bacteriuria (P < 0.001).
| Valuea | Study Group (n = 65) | Control Group (n = 65) | P Value |
|---|---|---|---|
| Age (years) | 38.8 ± 14 | 40.6 ± 13 | 0.4 |
| Vitamin D (ng/mL) | 28.8 ± 10 | 50.3 ± 9 | < 0.001 |
Table 1
The mean serum 25(OH)D3 levels among premenopausal women with and without asymptomatic bacteriuria were 27.3 ± 10 and 48.6 ± 9 ng/mL, respectively (P < 0.001). In total, 40% of the study population with asymptomatic bacteriuria had sufficient 25(OH) vitamin D (30 - 100 ng/mL), while 100% of the control group without asymptomatic bacteriuria had sufficient levels. Moreover, 1.53% of the study population with asymptomatic bacteriuria had 25(OH) vitamin D deficiency (< 10 ng/mL), while 58.46% had vitamin D insufficiency (10 - 30 ng/mL). All the participants were of the same racial background.
5. Discussion
Vitamin D or calciferol refers to a group of lipid-soluble compounds, characterized by a 4-ringed cholesterol backbone. From a pharmacological and clinical point of view, the most important circulating form of vitamin D is 25(OH)D. Vitamin D adequacy is best evaluated by measuring the serum level of 25(OH)D. The lower limit of normal for 25(OH)D varies considerably in different studies and is influenced by several factors, including geographical location and sunlight exposure of the population.
Vitamin D plays an important role in antimicrobial activities of macrophages, whereas its impact on asymptomatic bacteriuria and UTI has not been extensively explored. The importance of vitamin D in the induction of innate immunological responses against bacterial infections has been clearly addressed in previous studies. This significant role has been mainly explained by increasing neutrophil motility and phagocytic function (20, 21).
According to recent studies, expression of specific endogenous antimicrobial peptides in immune cells is regulated by vitamin D (22). Production of cathelicidin, as a human antimicrobial peptide, is induced by Escherichia coli infection, which could play a significant protective role against the development of UTIs in humans and mice (23). In the present study, serum 25(OH)D3 levels were significantly lower in patients with asymptomatic bacteriuria, compared to women without asymptomatic bacteriuria.
Considering the abovementioned mechanisms, susceptibility of women with low serum levels of 25(OH) vitamin D to asymptomatic bacteriuria and probably recurrent UTI could be explained. Our findings are consistent with previous studies regarding the association of vitamin D level with UTIs. In a study conducted in Turkey, the relationship between serum vitamin D level and urine cathelicidin level was measured in children with UTI, caused by E. coli. Their findings demonstrated that the serum level of vitamin D was significantly higher in the control group. Moreover, cathelicidin level was significantly different among individuals with sufficient and insufficient vitamin D (24).
In another case-control study conducted in the Netherlands, vitamin D level was compared among patients with E. coli UTI and healthy individuals. Interestingly, 27% of UTI patients with bacteremia and 19% of UTI patients without bacteremia showed vitamin D insufficiency; in contrast, vitamin D level was insufficient in 11% of the controls. It should be noted that all the controls were recruited in winter, and the frequency of vitamin D insufficiency was relatively high in these healthy individuals. Moreover, comparison of the controls with patients recruited in winter indicated similar results, and vitamin D level was significantly higher in healthy subjects (25).
In another study by Nseir et al., the relationship between serum level of 25(OH) vitamin D and recurrent UTI was assessed in premenopausal women. The results showed that 25-(OH)D level was significantly lower in patients with recurrent UTI, compared to the healthy controls. After adjusting for potential confounders, the association between 25(OH)D insufficiency and risk of recurrent UTI episodes remained significant. Maternal history of recurrent UTI and lack of probiotic use were other suggested risk factors (7).
The strength of this study was the inclusion of both pre- and postmenopausal women. On the other hand, the main limitation of this study was the retrospective design. Moreover, we did not collect any data regarding other potential factors for susceptibility to recurrent UTI, such as diabetes mellitus, maternal history of recurrent UTI, drug history (oral contraceptives and probiotics), and sexual intercourse; therefore, we could not perform any multivariable analyses. Furthermore, the study was conducted in a private laboratory in Tehran, which limits the generalizability of the obtained results.
In conclusion, our results demonstrated that insufficient vitamin D level might be associated with asymptomatic bacteriuria in both pre- and postmenopausal women. Our findings highlight the importance of understanding the nonskeletal functions of vitamin D, particularly its immunomodulatory effects. Moreover, the findings underscore the importance of establishing screening programs for early detection of vitamin D insufficiency, especially in women who are more susceptible to UTIs. However, further prospective studies with a larger sample size are essential to substantiate the available evidence.