1. Introduction
Hydatid disease is an infection caused by Echinococous granulosus. Despite the fact that humans are considered as accidental intermediate hosts of this parasite, cystic echinococcosis (CE) could be fatal (1). This zoonotic disease, associated with poverty and poor hygiene, is especially endemic in animal husbandry communities with low-income (2). Age, dog ownership, residence area, and educational level are believed be significantly associated with echinococcosis (3). The rate of hydatid disease is high in different parts of Asia including the Middle East, and especially in Iran, and is even hyper-endemic in some areas (4-8).
The liver is the most common site to be affected by this disease (70%), followed by the lungs (20%) (6). Hydatid disease of breast is rare and occurs in less than 1% of the cases (5, 7, 9, 10). In this paper, we presented a known case of hepatic hydatidosis readmitted due to hydatid cyst of the breast.
2. Case Presentation
A 38-year-old woman, who was a known case of hydatid cyst of the liver since eight years ago, presented with new onset of abdominal pain in the right upper quadrant (RUQ) and the left upper quadrant (LUQ). The patient was a candidate for cystectomy, but refused to undergo liver resection. She also neglected her medical treatment. She presented to our hospital with the aforementioned abdominal pain for the first time after her initial diagnosis.
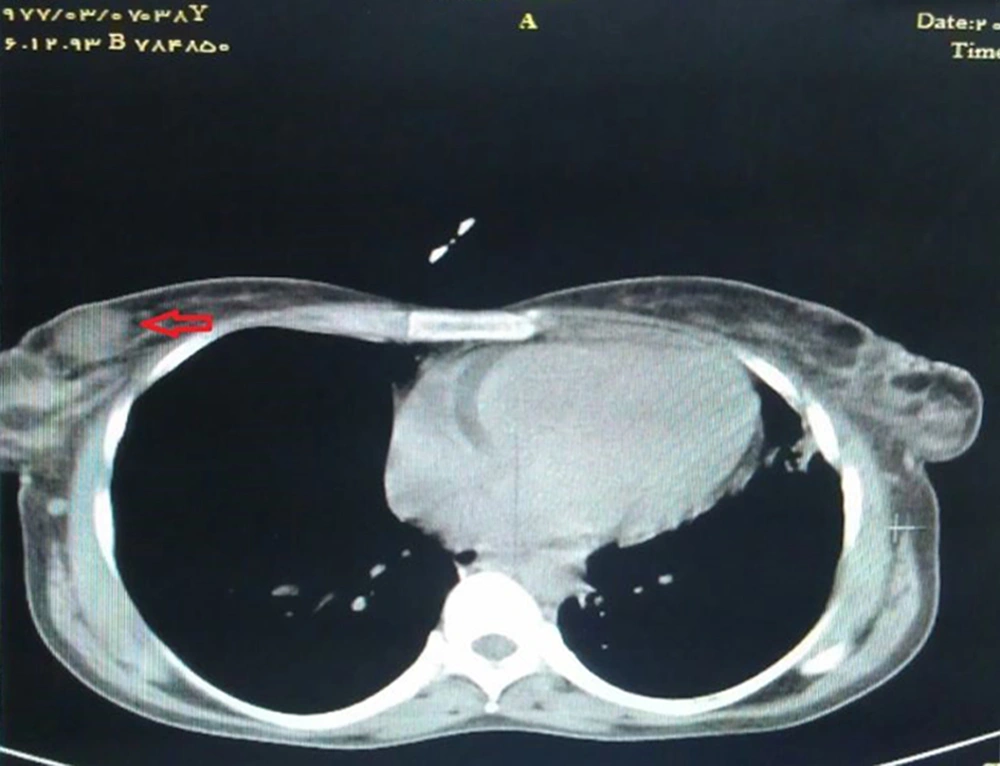
In the process of her evaluation, computed tomography (CT) scan was performed, which was not only suggestive of hydatid cysts in the right lobe of the liver and spleen (Figure 1), but also accidentally revealed two suspicious masses in the left breast and another in the right one (Figure 2). The size of the breast cysts was estimated to be 35 × 35 and 25 × 31 mm in the upper lateral and lower lateral quadrants of the left breast and 31 × 31 mm in the upper lateral quadrant of the right breast. The results of blood analysis and chest radiograph were normal.
The patient underwent surgery and the breast cysts were resected (Figure 3). Laparotomy followed by total splenectomy and complete resection of the liver cysts was also performed. In addition, cholecystectomy was carried out due to the closeness of the cysts to the gallbladder and severe adhesions to the adjacent tissue.
Histopathologic studies of the resected cysts and cyst materials confirmed the diagnosis of hydatid disease. Finally, the patient was discharged with albendazole (10 mg/kg daily for three weeks) and was advised to come back for further follow-up.
3. Discussion
Cystic echinococcosis is a parasitic infection caused by several Echinococcus species (11). The adult tapeworm lives in the small intestine of canines (the definitive host). Its reproductive segments (proglottids) are released in the feces. The intermediate hosts (e.g., sheep, goat, and cattle) are then infected by ingesting contaminated plants. After entering the ruminant's gut, the egg hatches and releases an oncosphere, which penetrates the intestinal wall, migrates to different organs (especially the liver and lungs) and there develops into a cyst. The cycle is completed when the definitive host ingests the cyst-containing organs of the intermediate host (12, 13).
Humans are considered as an incidental host, acquiring the infection mainly by consumption of contaminated vegetables and water. Similar to intermediate hosts, ingested larvae penetrate the systemic or lymphatic circulation from the intestinal mucosa and finally reside in different organs, mostly the liver and lungs (6, 13). Rarely, the larvae may also infest the muscles, kidneys, spleen, bones, and breasts (5, 7, 9, 10, 14).
Hydatid disease of the breast is rare and accounts for less than 1% of all cases (5-7, 10). Cystic echinococcosis usually involves the breast as the secondary site following hematologic or lymphatic dissemination. However, rarely breasts can be the primary site of hydatidosis (15, 16). The typical presentation of breast hydatidosis is painless slow growing breast lump without regional lymph node involvement. It generally affects women between 30 - 50 years of age. It might mimic fibroadenoma, phyllodes tumors, chronic abscess, or even carcinoma. Thus, hydatid cyst of the breast should be included in the differential diagnosis of breast lumps, especially in endemic areas (4, 9). The disease can be diagnosed by radiologic or serologic means, neither of which is definitive. The diagnosis of hydatid disease is based on the findings of enzyme-linked immunosorbent assay (ELISA) for echinococcal antigens and results are positive in approximately 85% of infected patients (9, 12, 17). In patients with intact cysts or without any scolices or any viable parasites, ELISA results may be negative. Serologic tests such as intradermal and indirect hemagglutination tests may be used to confirm the diagnosis (4, 5).
Mammography may show the characteristic ring shape structures inside the mass, which strongly suggests hydatid cysts of the breast (4, 18). Ultrasound and magnetic resonance imaging are helpful diagnostic tools. Although fine needle aspiration biopsy in suspected lesions may confirm the diagnosis by observing the hooklets of the parasite, it should be avoided due to the high risk of anaphylactic reaction (5).
3.1. Conclusion
Although hydatid cyst of the breast is rare, it should be considered as a differential diagnosis of breast lumps, especially in endemic areas and among immigrants from endemic areas. In the breast, hydatidosis may mimic a simple cyst, fibroadenoma, chronic abscess, phyllodes tumor, or even carcinoma. Both serologic (such as ELISA) and radiologic studies (such as mammography, ultrasonography, and CT scan) can be helpful to establish the diagnosis of hydatid disease. Finally, surgical removal without spillage is the best method of the treatment of hydatid lesions.