1. Background
Human T-lymphotropic virus type 1 (HTLV-1), as a virus of the retroviridae family was firstly recognized in humans during year 1980 (1) and 1982 (2). This virus has an envelope and is categorized as type C retrovirus, containing double-stranded RNA. The HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP) (3) and adult T cell leukemia (ATL) are two major diseases associated with the HTLV-1 virus (4). Although rare infected patients with HTLV-1 develop one of the HTLV-related diseases (< 3% to 5%), the majority of the remaining patients are asymptomatic (4). The HTLV1-infected individuals, who manifest HAM/TSP or ATL, are debilitating with few treatment options and poor prognosis, which is often fatal (5). Since there is no treatment options and preventive vaccine for HTLV-associated diseases, the prevention approach of HTLV infections is very important. The HTLV-1 virus could be transmitted through sexual contact with infected individuals, mother to infant, infected needles, and blood transfusion, however, blood product transfusion is still the main agent of HTLV-1 transmission (5-7).
It has been estimated that almost 15 to 20 million individuals might be infected by HTLV-1 around the world (8). It has been known that HTLV-1 has spread worldwide, however, HTLV-1 is endemic in certain parts of the world, including southwestern Japan, Central and South America, the Caribbean islands, west of Africa, southern Italy, and Taiwan (9-14). In 1986, the first case of Iranian patient with ATL was identified from Mashhad (15). Mashhad is an endemic region for HTLV-1 infection in Iran (16, 17). Although some individuals, such as thalassemia patients, hemophiliacs patients, sex workers, and injecting drug users are at high risk for HTLV-1 infection, hemodialysis patients are also considered as a high risk group for HTLV-1 because of their requirement for blood transfusion (18). To the best of the author’s knowledge, there is no study regarding HTLV-1 prevalence in hemodialysis patients in Tehran, thus, the current researchers decided to investigate the prevalence of HTLV-1 infection in hemodialysis patients in this city.
2. Methods
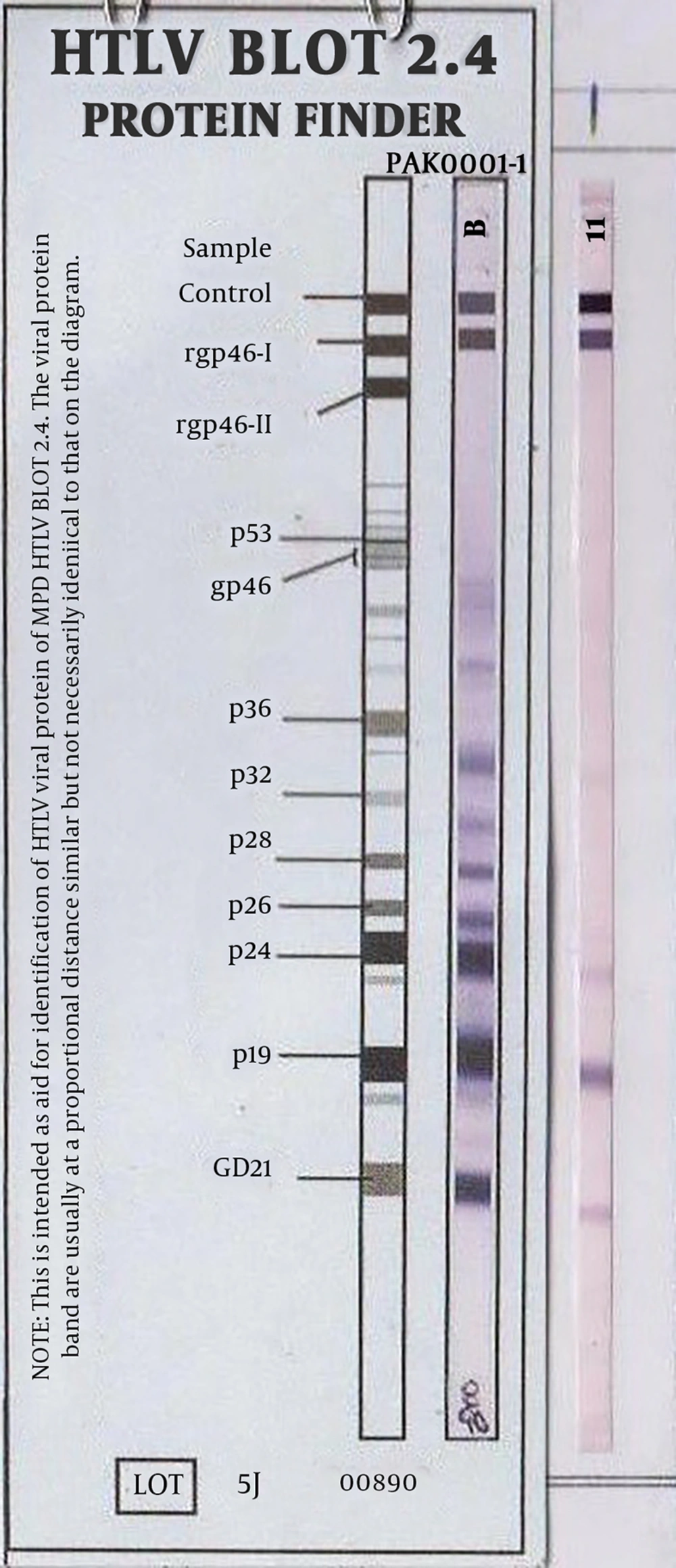
This research studied 150 patients, who attended the hemodialysis units of Imam Reza, Hajar, Golestan and Besat Hospitals of Tehran. Overall, 5 mL of blood was collected from patients and subsequently its serum was isolated and stored at -20°C. A data collection form was completed for patients after blood sampling. Serum level of anti-HTLV-1 was assessed in patients using the enzyme-linked immunosorbent assay (ELISA). To evaluate anti-HTLV-1, this research used the ELISA kit (Dia Pro Diagnostic Bioprobes, Milan, Italy), according to the manufacturer’s instructions. Absorbance at 450 nm was read in a 96-well microplate ELISA reader (BioTek Instruments, Inc.). After screening of anti-HTLV-1 by ELISA, the Western Blot method (Gene Lab Diagnostic Ltd, Singapore) was utilized on positive samples to approve HTLV-1 infection.
3. Results
A total of 150 patients aged 24 to 88 years, who were admitted to hemodialysis units, were included in this study. The mean age of patients at the time of study was 13.39 ± 63.57 years. In the present study, the patients were 80 males and 70 females. Among all patients, three patients died during the survey. All patients lived in Tehran. None of the patients had a history of infection to HTLV-1 in their families. Among the participants, 118 (78.6%) cases had a history of at least one blood transfusion (86.2% of males and 70% of females). Demographic and laboratory data of hemodialysis patients are provided in Table 1.
| Hospital’s Name | Number of Patients | Gender (Male/Female) | Median Age (Y) | Mean Age (Y) | Results (Negative/Positive) |
|---|---|---|---|---|---|
| Golestan | 30 | 18/12 | 24 - 83 | 62.8 ± 16.37 | 0/30 |
| Hajar | 50 | 30/20 | 24 - 88 | 68.16 ± 11.2 | 0/50 |
| Emam Reza | 35 | 18/17 | 27 - 88 | 62.74 ± 13.78 | 0/35 |
| Besat | 35 | 20/15 | 44 - 85 | 59.4 ± 11.81 | 1/35 |
In the primary screening by the ELISA assay, the researchers identified only one patient, who was positive for HTLV-1. Subsequently, the researchers evaluated the sample with western blot and observed intermediate results for HTLV-1. After two months, blood from this patient was obtained and this sample was examined with ELISA and western blot again. Surprisingly, the sample was positive by both ELISA and western blot tests. The patient was a 71-year-old female, who manifested end-stage renal disease due to glomerulonephritis and was under dialysis. Two years prior to the study, this patient had received blood due to bleeding. She had a history of negative results for hepatitis B and C viruses. In total, she had no clinical manifestation. The data demonstrate that the prevalence of HTLV1 in the patients on hemodialysis was low (0.66%).
4. Discussion
Despite advances in finding an appropriate treatment for HTLV-1 mediated-diseases, no therapy has been found for these patients; however, knowing the prevalence of HTLV-1 in various populations and different regions could be useful in setting up prophylactic methods to decrease rates of HTLV-1 infections from infected populations. To the best of the author’s knowledge, there is no study regarding HTLV-1 prevalence in hemodialysis patients of Tehran, thus, the current authors decided to investigate the prevalence of HTLV infection in patients on hemodialysis in Tehran Province. The results demonstrated low prevalence (0.66%) of HTLV1 infection in patients on hemodialysis in Tehran.
The HTLV-1 infection is endemic in specific regions of the world (19). The frequency of HTLV among the population of blood donors in different countries is as follows: America (0.013), Sweden (0.001), Netherlands (0.002), Denmark (0.003), France (0.004), Italy (0.007) (20), and Argentina (0.05) (21). In countries near Iran, such as Kuwait and Saudi Arabia, the prevalence of HTLV-1 infection among blood donors was 0.016% and 0.046%, respectively (22, 23). In Iran, there is also some reports that suggest relatively high prevalence of virus in these patients. Previous studies reported that some parts of Iran, such as Mashhad, Sabzevar, and Neyshabour, are endemic regions of HTLV1 infection (24-26).
The current authors indicated in previous studies that there is an infection with hepatitis G virus among hemodialysis patients referred to Iranian army hospitals (27, 28), thus they assumed that infection with HTLV might be observed in these patients. On the other hand, it seems that blood transfusion is the major route of HTLV transmission in Iran, because identification of anti-HTLV is not a routine laboratory test in all blood transfusion centers. There are several reports about the prevalence of HTLV-1 infection among blood donors in different cities of Iran. The highest rate of infection to HTLV-1 is related to Mashhad, as two studies demonstrated frequency of 3.0% (29) and 2.1% (25) in this city. Furthermore, the prevalence of HTLV-1 infection among blood donors in other cities of Khorasan Province, such as Sabzevar (1.6%) (24) and Neyshabour (6.5%) (30), was also high compared with other provinces of Iran. However, a low prevalence has been reported in other cities of Iran, such as Urmia (0.34%) (18), Mazandaran Province (0.08%) (31), and Golestan Province (0.3%) (32). The prevalence of HTLV-1 was higher in high risk patients, such as individuals with thalassemia, and different frequencies in various regions of Iran, such as Shiraz (25.55%) (33), Bushehr (3.07%) (34), Charmahal-Bakhtiari Province (7.2%) (35), Gorgan (4.4%) (36), and Tehran (6.9%) (37) have been reported.
In addition to patients with thalassemia, patients on hemodialysis are also at high risk for HTLV-1 infection, therefore it is essential to evaluate the HTLV-1 immunoglobulin in blood products.
This study demonstrated that the prevalence of HTLV-1 in the sampled hemodialysis patients was 0.66%. Indeed, this study identified only one patient on hemodialysis, who only had a history of blood transfusion two years ago without clinical manifestation. Although there are some reports about the prevalence of HTLV-1 among hemodialysis patients in several regions of Iran (38), there is no report regarding HTLV-1 infection on hemodialysis patients of Tehran for comparison with the current study. Apart from endemic regions, such as Neyshabour, where the prevalence of HTLV-1 is high (39), the frequency of HTLV-1 infection among hemodialysis patients is very low. Two studies from Bushehr (34) and Sanandaj (40) demonstrated that none of hemodialysis patients were infected with HTLV-1. However, Khameneh et al. (18), evaluated 95 patients in Urmia and found only one hemodialysis patient, who was infected with HTLV-1. Furthermore, Ghafari et al. (41), studied 160 hemodialysis patients of Mazandaran and identified only one infected patient. These results were completely consistent with the current study. Recently, a study indicated that HTLV-1 could be transmitted among patients under hemodialysis, especially older females, similar to the patients of the present study. They showed that older age provides a greater length of exposure to events that might lead to acquiring the virus, including intravenous drug use or blood transfusion (42).
Although the current results demonstrated that the prevalence of HTLV-1 is low among patients on hemodialysis in Tehran, one point regarding the present study is important. Since in the primary screening, the researchers observed intermediate results for HTLV-1 in one patient yet after two months they observed positive results for HTLV-1, thus a possibility arises that HTLV-1 infection may be transmitted by hemodialysis machines because this patient did not receive blood for the past two years. To the best of the author’s knowledge, there is no study that reports HTLV-1 infection in patients, who had not received new blood samples. Although chance of HTLV-1 spread during the hemodialysis procedure is low due to the biology of the virus, the results indicated that there is a possibility of transmission of HTLV-1 among patients under hemodialysis, who did not receive blood sample from two years ago. However, it was shown that proviral load of HTLV1 could be significantly correlated with leukocyte count, hemodialysis duration, and the number of blood transfusions in patients on hemodialysis (43). Generally, further studies need to confirm whether infection HTLV-1 could transmit through infectious hemodialysis machine or other events. In conclusion, patients with HTLV-1 infection are better to be hemodialyzed in separate rooms, hemodialysis machine, and instruments. Moreover, the hemodialysis machine requires to be washed more precisely for positive HTLV-1 patients.