1. Introduction
Chlamydia psittaci is an intracellular pathogen (1). It is a zoonotic pathogen that infects a wide range of birds as hosts and may cause severe disease when is transmitted to humans (2). Infected birds are often asymptomatic, but sometimes they may have symptoms like chills, anorexia, and diarrhea (3). Contaminated birds pass pathogens through their stool and nasal secretions, and humans get sick from contact with them (4). The disease caused by Chlamydia psittaci is called psittacosis or parrot fever (4). Since this disease is not restricted to parrot and other birds can also transmit microorganism, it is also called Ornithosis (3). Infection in humans mostly presents as community-acquired pneumonia (CAP), which is responsible for 1% - 1.2% of all causes of CAP (5, 6). Human-to-human transmission is rare and isolation and chemoprophylaxis are not necessary. This patient was chosen for the case presentation because of receiving various treatments. Diagnosis in the early stages of the disease and initiation of prompt treatment can reduce mortality from 20% to 1% (3).
2. Case Presentation
The patient was a 47-year-old man complaining of fever and chills, dyspnea, and cough that began two weeks before admission. The patient visited a doctor in the outpatient service at the early stage of disease, who diagnosed acute sinusitis and prescribed co-amoxiclav and clarithromycin subsequently. After seeing no improvement, he once again returned to the clinic and was admitted this time.
The patient or his family did not have a history of lung disease or other illnesses. He traveled to India in the last year. History revealed the presence of a parrot at home with no history of smoking. In his career, he had not been in contact with chemicals. The patient mentioned a weight loss of 6 kg in the last 2 weeks. The vital signs were: Temp. 38°C, B / P 100/70 mm/Hg, RR 24 / Min and PR 90/Min. Clinical examination was normal except for bilateral coarse crackle in the lung. The examination of the heart did not have an abnormal point. The patient was admitted with a diagnosis of pneumonia and the treatment was started with meropenem and levofloxacin.
Laboratory investigation revealed leukocytosis with 16300 WBC and 78% Polymorphonuclear (PMN) and platelet count was 453,000 and eosinophil and band-bone were higher than normal but other CBC indices were normal (Table 1). Collagen-vascular tests, including P-ANCA, C-ANCA, ANA, and Anti-dsDNA were reported normal. In the liver tests, alkaline phosphatase showed higher than normal range but other indices were normal. The CRP and ESR were 47 and 72, respectively.
| Test | First Day | Third Day | Normal Range | Flag |
|---|---|---|---|---|
| WBC | 16300 | 10200 | 4500 - 11000 | High |
| Neutrophil, % | 77.9 | 71.5 | 55 - 75 | High |
| Lymphocyte, % | 12.4 | 18.1 | 20 - 45 | Low |
| CRP, mg/L | 47.7 | ----- | < 8 | High |
| ESR 1st hour, mm/h | 72 | ----- | 0 - 22 | High |
| Chlamydia psittaci (IgM), RU/mL | 1.5 | ----- | < 0.8 | High |
| Chlamydia psittaci (IgG), RU/mL | 61.5 | ----- | < 16 | High |
Laboratory Values Throughout Hospitalization
In bronchoscopy, there was copious purulent discharge but other findings were normal. Bronchoalveolar lavage (BAL) was performed and the samples were sent to the laboratory for bacterial, mycobacterial and fungal smear and culture, which gram-positive cocci (Staphylococcus) and gram-negative bacilli were reported.
Due to the lack of recovery, the history of contact with a parrot and the previous antibiotic regimen (meropenem and levofloxacin), the treatment was changed to Doxycycline and Ceftriaxone. In the next visit, the fever discontinued and RR reached 16/Min. In subsequent tests, the patient's leukocyte was reduced to 10,200 with a predominance of 71% PMN. Serological test results for Chlamydia psittaci were IgM 1.5 RU/ML (normal range less than 0.8 RU/ML) and IgG 61.5 RU/ML (normal range less than 16 RU/ML), which were positive and diagnosis of pneumonia due to Chlamydia psittaci was established for the patient. Eventually, the patient was discharged in a good general condition with oral doxycycline.
3. Discussion
After 5 to 15 days of incubation period, the disease may start insidiously and suddenly lead to multiple syndromes. The disease may present as atypical pneumonia with non-productive cough, fever, headache, and abnormal changes in chest graph, which is usually more than expected on the basis of clinical symptoms and examination (3). In a study, 11% of patients with probable or confirmed psittacosis had productive cough (7).
According to the signs and symptoms of the patient, he was hospitalized with the diagnosis of pneumonia, which was treated with meropenem and levofloxacin. Finally, due to no relief in symptoms, history of contact with a parrot, and the possibility of chlamydial induced pneumonia psittaci, antibiotics were changed to Doxycycline and Ceftriaxone. The patient responded quickly to the treatment. It is notable that in one study, 60% of patients with probable or definite psittacosis had no history of contact with birds (7). There are many differential diagnoses that are variable according to psittacosis-induced syndromes, for example in the atypical pneumonia form, viral pneumonia, Q fever, Legionellosis, Mycoplasmal pneumonia are considered to be differential diagnoses (3). Although pneumonia is the most common manifestation of psittacosis, all organs can be involved in this disease (8). Several cases of severe pneumonia with ARDS and pericarditis have been reported (9). Severe pneumonia may be the primary manifestation of the disease that led to ICU admission (10).
In a study of 85 patients with suspected Psittacosis, 48 cases were confirmed as definitive or probable psittacosis (7). In another study that reviewed 11 articles over a 30-year-period, it was found that in patients with psittacosis and severe respiratory insufficiency, 10 out of 12 patients had exposure to birds as a major risk factor. Severe hypoxemia and kidney failure were associated with poor prognosis. Eight patients died of psittacosis or complications of the infection (11).
The most common symptom is fever, occurring in 50 to 100% of cases but most often in the last stages of the disease. Headache and myalgia have been reported in 30 to 70 percent of the cases; however, these symptoms are misleading until the cough occurs due to lack of specificity. Even at this time, there are many distinct diagnoses. The most common findings in the examination are fever, throat erythema, rale or other abnormal findings in lung auscultation and hepatosplenomegaly. Horder’s Spot, one of the cutaneous manifestations of psittacosis, is a maculopapular lesion on the chest or trunk that is pink. The involvement of other organs, such as cardiac and kidney involvement, hepatitis, neurological manifestations, etc., are consequences of the systemic nature of the disease (3). In one study, the prevalent symptoms were fever, cough, headache, myalgia, nausea, diarrhea, chills, sputum, chest pain and shortness of breath (7). Our patient’s presentations were pulmonary involvement, headache, fever, chill, and productive cough.
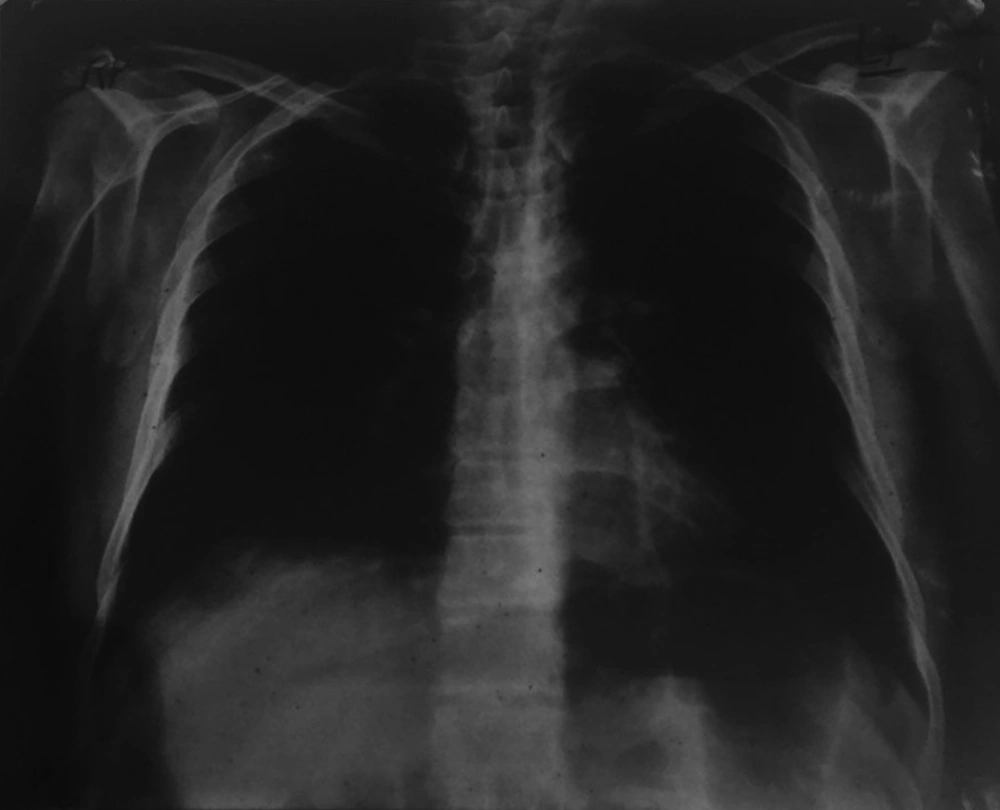
In the CBC test, WBC usually is normal or increased slightly and two-thirds of cases have a leftward shift. In 50% of cases, liver tests are abnormal. The CXR is abnormal in 75% of cases, which is more than expected on the basis of respiratory signs and symptoms. The most common abnormal appearance in X-ray is a consolidation in a single lower lobe. Other patterns include ground glass opacity (GGO), patchy view, segmental view, or lobar and miliary view, and sometimes have Halo Sign view that may be misleading with other respiratory illnesses. In 50% of cases, we have pleural effusion, which is small and asymptomatic (3). In this patient, leukocytosis was observed with the leftward shift and patchy infiltration in right lower lobe in X-ray (Figure 1).
According to the CDC, the definitive case of psittacosis is a person with consistent clinical symptoms and laboratory confirmation having one of the following criteria:
1- A titer of 1/16 IgM by MIF (microimmunofluorescence) method.
2- Positive culture of respiratory secretions.
3- Four-fold or greater rise in titer in CF (Complement fixation) or MIF antibody to a titer 1/32 in the specimens with two weeks intervals.
The probable case is an individual with compatible symptoms along with a confirmed history of contact with a patient with confirmed disease or a titer of 1/32 in a sample by CF or MIF assay (3). Based on a single serologic test, which was positive, the patient is considered a probable case of psittacosis.
The blood and sputum cultures are possible in the first 4 days and the first two weeks of the disease, respectively but usually cultures are not considered. Because the risk for laboratory staff and serological method is preferred (3). In a study, because of the cross-reactions of old methods such as cultural, serological, and MIF assays, the replacement of new molecular methods such as PCR and RT-PCR for diagnosis has been discussed and was emphasized that modern methods are more standardized (12).
Drug of choice is doxycycline, 100 mg twice daily or tetracycline 500 mg four times a day for 10 to 21 days. Macrolides are effective in vitro and are recommended as alternative therapies in children and pregnant women; however, they may be less effective in severe cases and do not protect the fetus during pregnancy. Fluoroquinolones need more clinical experiences. Most patients feel better within 24 hours with therapy. Without treatment, the fatality rate of psittacosis is approximately 20%; however, it is reduced to 1% following the treatment (3).
3.1. Conclusions
Given the high mortality rate of disease in the absence of treatment, it is necessary that the disease is quickly diagnosed and treated. Due to the non-specificity of the symptoms and on the other hand, the absence of contact with birds in a considerable number of patients, many differential diagnoses may be possible and achieving an accurate diagnosis is more difficult. However, paying attention to the symptoms and history of contact with birds can improve the diagnosis. As soon as the disease is diagnosed, the treatment should be started and continued for 10 to 21 days. The shorter course of the treatment will be associated with possible recurrence.