1. Background
Fever of unknown origin (FUO) has been a challenging diagnosis for decades. The definition of FUO has been refined since first introduced by Petersdorf and Beeson in 1961 as a result of access to new para-clinical tests and treatment options (1-3). A body temperature above 38.3°C in different occasions for over 3 weeks with undefined etiology after 3 outpatient visits or 3 days of in-hospital work-up is now known as the FUO (3-6).
The clinical and epidemiological picture of FUO has been constantly changing. The causes and different approaches taken to reach a definitive diagnosis have been widely investigated in the literature (all + Louizidou). For a long time, infectious agents have been the primary cause of FUO (7-11). Despite the widespread use of antimicrobials, there are rare agents that may present with chronic unexplained fever and require high clinical suspicion (12). Case reports are also published on iatrogenic causes of FUO that were not commonly seen before (13). In developed countries, the epidemiology of FUO has changed from a prolonged fever in general or outpatient clinics to FUO among ICU patients (14).
Although the new imaging technologies including fluorodeoxyglucose positron emission tomography (FDG-PET) are now known to be of high diagnostic yield, they are not readily accessible in many settings and have limitations in the detection of certain etiologies of FUO (15). Hence, the inclusion of modern approaches in the diagnostic algorithms of FUO is not yet practical.
In Iran and the neighboring countries, infections have been the major cause of FUO with the highest numbers reported among TB patients (9, 16, 17). Several studies have investigated the etiologies of FUO both in children and in adult populations in Iran (18-21). The number of unknown cases has not evolved significantly in years and the clinical picture is still focused on infectious causes. However, new studies from tertiary centers are not available.
An update on the local prevalence of various etiologies of FUO and their distribution based on the gender and age of patients helps clinicians in their work-up and diagnosis of FUO. Hence, we conducted the present observational study to document the latest information available through hospital database in an academic and referral setting.
2. Methods
2.1. Participants and Setting
In a retrospective cohort, documented patient files at the Department of Infectious Diseases of a Tertiary Academic Center were reviewed. The tertiary center is located in the capital city of Tehran with over 1300 active beds and 200 daily admissions in the emergency room including patients diagnosed with infectious diseases.
We retrieved all files registered with the initial diagnosis of fever of unknown origin (FUO) from March 2009 to April 2014. The patient records were then investigated using a prepared checklist.
All patients aged 18 years or older, with at least three weeks of fever (> 38.3°C) measured at different time points without a known cause in three outpatient visits or after three days of hospital work-up, were included in the study. Patient files with the diagnosis of neutropenic or hospital-acquired FUO or those with HIV/AIDS were excluded from the final sample.
2.2. Checklist
A checklist was prepared to evaluate patient records concerning the following characteristics: age, gender, days of fever before admission, time of admission, and discharge. The clinical course of the disease (e.g. response to empiric therapy) during a hospital stay, as well as laboratory findings, was documented. The laboratory tests included complete blood counts, biochemical, and metabolic panels, followed by serologic, immunologic, and bacteriologic tests when necessary. Other para-clinical findings including imaging study results and report of pathologic evaluations were also documented in the checklist where available. Patients were classified in four groups in terms of the main etiologies of FUO: infection, neoplasia, non-infectious inflammatory disease (NIID), and miscellaneous (others); a final category was considered for patients with no defined etiology after a thorough work-up (unknown).
Patients were also categorized based on the type of test/clinical approach utilized to reach the final diagnosis: invasive, non-invasive, or self-limited during a hospital stay.
2.3. Analysis of Data
We used the statistical package for social sciences (SPSS) version 16.0 (IBM Inc.) for data entry and analysis. Frequency and percentages were utilized for descriptive variables. For comparisons between categorical variables, we performed the Chi-square test. The level of significance was considered 0.05 (P value < 0.05).
2.4. Ethical Considerations
The study was approved by the Review Boards of the Tehran University of Medical Sciences. All files were reached through a local database after obtaining written consent from the Review Boards. The checklists were completed by a trained research staff in anonymous forms and final documents were filed and only accessed by the principal investigator.
3. Results
In total, we investigated the records of 101 patients with the diagnosis of FUO in our retrospective cohort from March 2009 to April 2014, among whom, 95 were 18 years or older that were included in the final analysis.
The median age of the patients was 39 years (interquartile range (IQR): 30 to 60). Among them, 53.7% were women. The median days of fever before admission were 30 days (IQR: 22 to 60), and the patients were hospitalized for a median of 10 days (IQR: 6 to 14).
3.1. Descriptive Analyses
Infections (23.1%) and non-infectious inflammatory diseases (21.1%) constituted the most common known causes of fever in our patient population. Table 1 indicates the frequency of other etiologies of FUO with detailed classifications.
| Etiology of FUO | No. (%) |
|---|---|
| Infections | |
| Pulmonary TB | 2 (9.1) |
| Extrapulmonary TB | 1 (4.5) |
| Milliary TB | 1 (4.5) |
| Brucellosis | 6 (27.3) |
| Endocarditis | 1 (4.5) |
| Salmonellosis | 1 (4.5) |
| Urinary tract infection | 4 (18.2) |
| Sinusitis | 1 (4.5) |
| Leptospirosis | 1 (4.5) |
| Pulmonary abscess | 1 (4.5) |
| Vivax malaria | 1 (4.5) |
| Infectious mononucleosis | 1 (4.5) |
| Cytomegalovirus infection | 1 (4.5) |
| Total | 22 (23.1) |
| Neoplasias | |
| Leukemia | 1 (5.9) |
| Lymphoma | 7 (41.2) |
| Hepatocellular carcinoma | 1 (5.9) |
| Colon cancer | 5 (29.4) |
| Pancreas cancer | 1 (5.9) |
| Thyroid cancer | 1 (5.9) |
| Myelodysplasia | 1 (5.9) |
| Total | 17 (17.8) |
| Non-infectious inflammatory diseases | |
| Systemic lupus erythematosus | 7 (35) |
| Rheumatoid arthritis | 5 (25) |
| Still disease | 4 (20) |
| Temporal arteritis | 2 (10) |
| Leukocytoclastic vasculitis | 1 (5) |
| Polyarteritis nodosa | 1 (5) |
| Total | 20 (21.1) |
| Others | |
| Drug reaction | 1 (20) |
| Familial Mediterranean fever | 2 (40) |
| Fibromyalgia | 1 (20) |
| Idiopathic thrombocytopenic | 1 (20) |
| Purpura | 5 (5.4) |
| Total | |
| Unknown | 31 (32.6) |
From 95 patients, invasive tests had been documented for 39 (41.1%) while non-diagnostic in 19 (20%). Non-invasive tests leading to final diagnoses were performed for 46 (48.4%). Two patients (2.1%) had self-limited fevers during the hospital stay and no specific diagnosis was found for them.
Laboratory tests were diagnostic for 37 (38.94%) patients (infection: 18 and NIID: 19). Pathologic studies led to a definitive diagnosis in 18 (18.9%) patients (neoplasia: 14 and NIID: 4), five patients (5.3%) were diagnosed using imaging studies and six others (6.3%) were diagnosed based on a response to empiric treatment. There was a significant association between the type of the utilized test for diagnosis and different etiologies of FUO (P = 0.001).
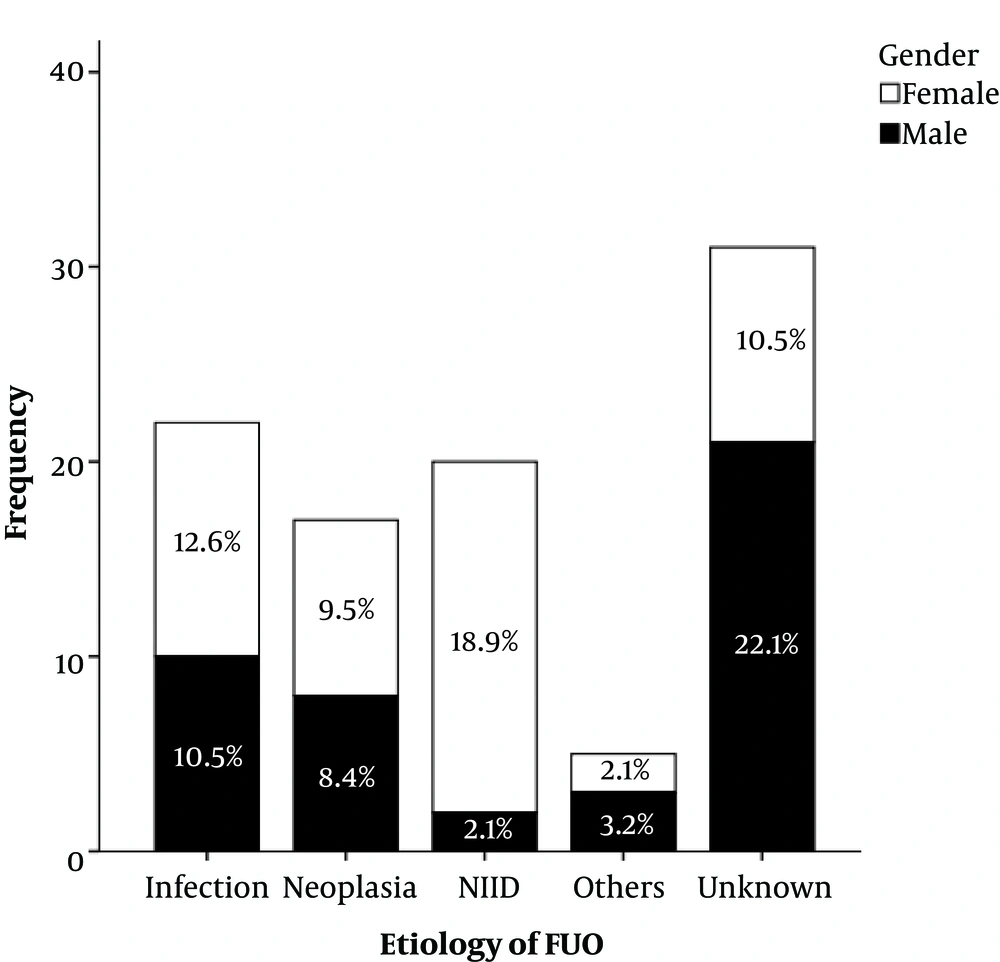
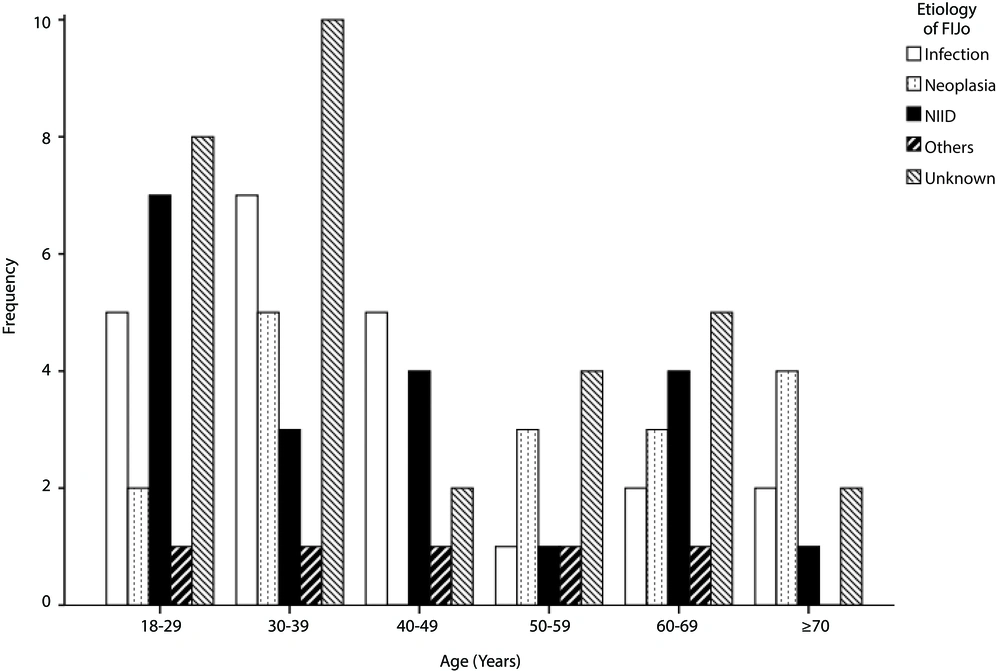
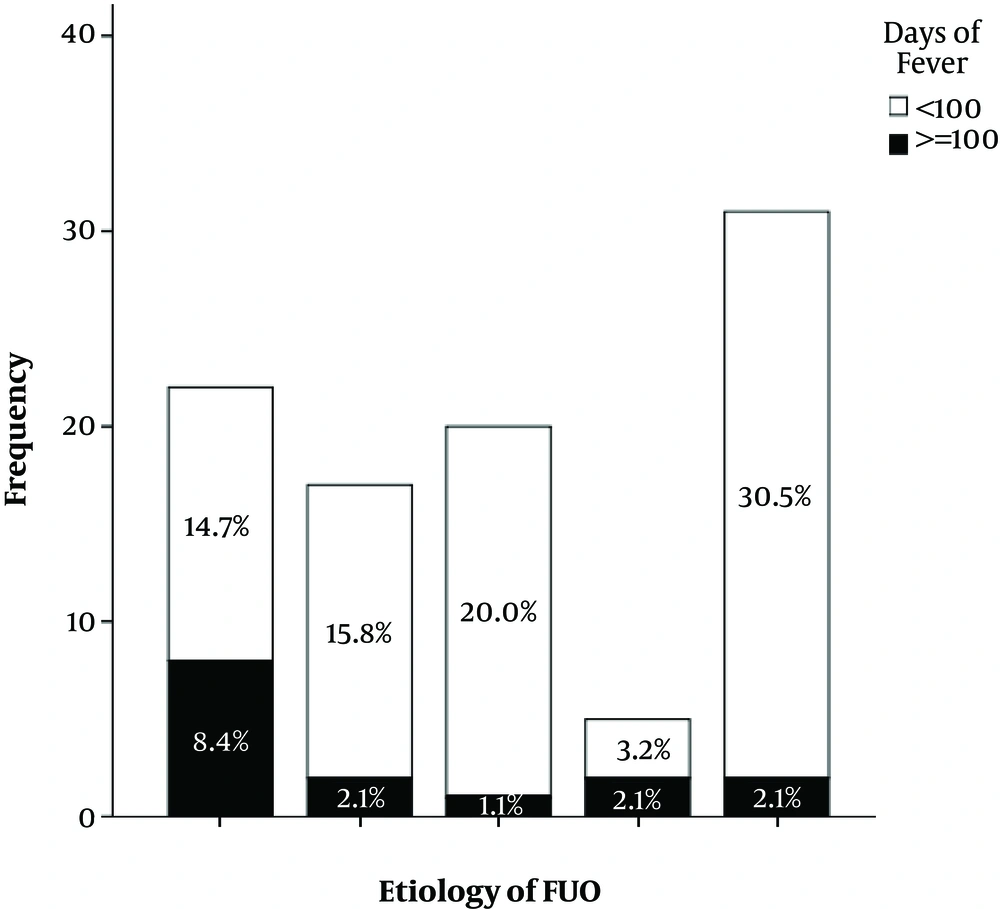
Figures 1 - 3 show the distribution of etiologies of FUO along gender, age categories, and days of fever before admission. We also examined the correlation between the etiology of fever and each of these demographic features. There was a significant correlation between gender and the etiology of fever (χ 2 = 16.7, P = 0.001); NIIDs constituted the major cause among women (35.3%) while most men were in the “unknown” category (47.7%). Days of fever also differed significantly with the etiologies of FUO (χ2 = 13.2, P = 0.011); among those with fever for over 100 days, 53.3% were diagnosed with an infectious cause. The etiology of fever had no significant correlation with age category (P = 0.594).
4. Discussion
The findings of our study indicate that infections and NIIDs are the two most common causes of FUO among adults in our tertiary center. The study was conducted in a referral hospital in a five-year retrospective observation.
Although the causes of FUO vary during the time and in different geographical areas, a few updates from national academic and tertiary centers have been recently available. This is a 5-year cohort from a referral hospital located in the most populated city in Iran. The findings, though generalizable, may be explained differently compared to peripheral centers. The extensive use of antimicrobials besides the widely available new diagnostic methods has facilitated the definitive diagnosis of many patients before referral to tertiary centers (14).
Previous investigations both in our country and in the region address infections as the major cause of FUO (Iran, Saudi, and Turkey). However, the findings from the current study show almost similar numbers of patients diagnosed with infections and NIIDs. This trend can partly be explained by the exclusion of HIV infected patients, but still comparable to the results from other studies since the 1930’s that show a decline in infectious causes of FUO (10, 14). The considerable proportion of “unknown” cases in the patient population is also analog to the concerns expressed elsewhere, specifically in the developed world (Horowitz).
From the spectrum of infectious causes of FUO, tuberculosis remains the most prevalent etiology. This finding is compatible with the studies performed in our neighboring countries (Turkey and Saudi). Despite advancements in case detection and patient management, modern technologies are not readily available in many areas, and clinical and conventional screening methods may overlook patients. Hence, FUO persists to be a presenting sign of TB (22). Unlike previous studies, no cases of osteomyelitis were observed in this investigation. We suggest that this finding can be attributed to successful management in peripheral settings, as well as early detection of local infections in outpatient clinics. However, the lower median age of our patients may have been a contributing factor (7, 8).
Lymphoma is the common malignancy presenting with FUO; a similar pattern has been reported in a previous evaluation in our setting (21). Considering the insidious nature of lymph node involvement in hematologic malignancies, the findings of other studies confirm the same picture (10).
We also observed a difference in the etiologies of FUO along demographic features. As expected, NIIDs were far more common among women although the age categories were not significantly associated (14). On the other side, men constituted the highest proportion of unknown cases among whom, one patient died and others had self-limited fevers during hospitalization or follow-up visits. Outpatient prescription of wide-spectrum antibiotics may have led to an increase in infectious agents presenting with FUO that are not routinely detected in our clinical work-up (Horowitz, implant, melioidosis). Thus, the periodic assessment of changes in local viral and bacterial epidemics needs to be considered in research works of epidemiologists and infectious disease specialists.
A major limitation of the present study was the large number of “unknown” causes of FUO among our patient population, which hinders the interpretation of the existing data. However, this has been evident in many studies performed elsewhere. Conducting prospective cohorts can minimize the issue.
4.1. Conclusions
This 5-year retrospective study shows that infections and non-infectious inflammatory diseases comprise the top two causes of FUO in a major referral center in Iran. TB remains a major threat to our population and FUO should always trigger work-up for TB, especially in high-risk groups. More attention needs to be drawn to the non-infectious causes of FUO that are on the rise while less addressed beforehand.