1. Introduction
The term hepatobiliary tuberculosis refers to the localized form of hepatic tuberculosis as a distinct clinical entity, with signs and symptoms related to the hepatobiliary tract (1). The abdomen is one of the most common extrapulmonary sites of infection (2).
In fact, 50% to 80% of cases of pulmonary tuberculosis are associated with concurrent hepatobiliary involvement (3). Biliary tract obstruction caused either by tuberculous adenitis or by intrinsic involvement of the biliary tract remains a rare occurrence (4, 5).
Hepatobiliary tuberculosis, like any other extrapulmonary and gastrointestinal tuberculosis, can occur due to Mycobacterium tuberculosis. The organism reaches the hepatobiliary tract through the hematogenous route and via the hepatic artery such as pulmonary tuberculosis (which may be active or inactive) (6).
In some cases, tuberculosis of hepatobiliary system comes through the portal veins (7, 8), especially if there is concomitant gastrointestinal tract tuberculosis. Lymphatic system is another way that tubercle bacilli may reach the liver. The rupture of a tuberculosis lymph node in the portal tract leading into the portal vein has also been mentioned as a route of infection (7, 9).
Primary hepatic tuberculosis is probably rare because even if there is no clinical or radiological evidence of tuberculosis elsewhere, pulmonary TB is discovered at autopsy in those patients who died, even if it is inactive (1).
We aimed to report a case of primary biliary tuberculosis with subsequent pulmonary presentation.
2. Case Presentation
A 28-year-old woman was admitted to our hospital due to recurrent abdominal pain, low-grade fever, and icterus. The abdominal pain was from 1 year ago, and it was intermittent without clear reason after outpatient work up. She had weight loss and pruritus as well. She did not mention cough, chest pain, or shortness of breath. She did not have other associated symptoms.
In habitual history, she denied using alcohol or tobacco. Family history was negative, and there were no such symptoms in other members of the family. The patient appeared ill on physical examination with a temperature of 38.2°C, blood pressure of 112/75 mm Hg, pulse rate of 92 beats per minute, and respiratory rate of 17 per minute.
Icteric conjunctiva was prominent. Pupils were equally reactive to light and accommodation. Auscultation of the chest and cardiac was normal. Abdominal exam showed tenderness in the right upper quadrant and right lower quadrant. Other examinations were normal. The results of the patient’s laboratory tests are shown in Table 1. Chest radiograph was normal, and tuberculin (purified protein derivative) skin test was negative at 2 mm induration.
| Parameters | Values |
|---|---|
| White blood cell count | 16000 |
| Differential (%) | |
| Granulocytes | 45 |
| Lymphocytes | 19 |
| Monocytes | 5 |
| Eosinophils | 31 |
| Hemoglobin (g/dL) | 10.9 |
| Hematocrit (%) | 84 |
| Platelet count (×103/μL) | 317000 |
| Erythrocyte sedimentation rate (mm/h) | 100 |
| C protein reactant | 75 |
| Amylase | 20 |
| Liver Function Tests | |
| Total bilirubin (mg/dL) | 1.2 |
| Aspartate aminotransferase (U/L) | 39 |
| Alanine aminotransferase (U/L) | 14 |
| Alkaline phosphatase (U/L) | 1056 |
| Gamma-glutamyl transferase | 43 |
| Viral markers | negative |
| S/E | NL |
| Anti-smooth muscle antibody | NL |
| Antimitochondrial antibodies | NL |
| Antinuclear antibody | NL |
Results of Laboratory Tests in Our Patient
On ultrasound evaluation the size of the liver was 158 mm with mild heterogeneous echo pattern and diffuse internal hepatic duct dilatation with common bile duct (CBD) measuring 10 mm. One hypoechoic focal lesion measuring 12 × 7 mm in the IVth segment of the liver was also reported.
Magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) elicited increased wall thickness in one-third of the proximal CBD and common hepatic duct, as well as cystic duct extending to intrahepatic main ducts and gall bladder neck, which caused bifurcation in the hepatic duct, right and left ducts, in particular the right proximal duct. Increased wall thickness of the gall bladder neck was observed. Brief dilatation in intrahepatic bile ducts was also noted.
Endoscopy and colonoscopy were performed, which showed normal findings. Biopsy of the abdominal lymph node revealed chronic granulomatous inflammation with high eosinophilia, which was negative for acid-fast bacilli. Bone marrow flow cytometer showed 2% immature myeloid cells without evidence of leukemia or lymphoma.
According to MRCP and IgG4 and high eosinophil with impression of autoimmune cholangiopathy, corticosteroid was administered. A few weeks later, the patient’s symptoms deteriorated, with fever and leukocytosis and the creation of multiple lymph nodes in the neck and abdomen, thus, she were hospitalized again.
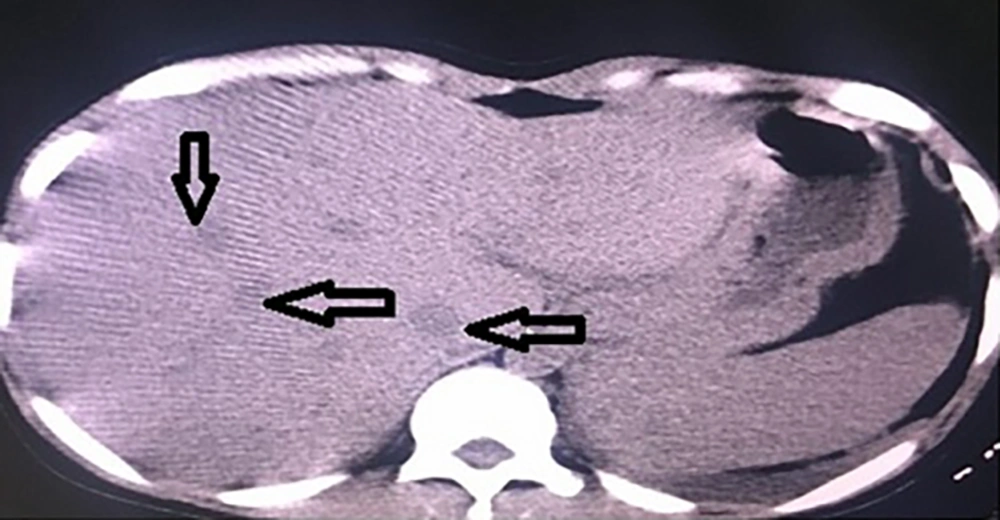
Ultrasound evaluation of the abdomen revealed common bile duct with a diameter of 11 mm, which had intraluminal echoes. Intrahepatic bile duct was dilated locally. Gall bladder wall was thickened (4 mm). A necrotizing lymph node measuring about 21 × 22 mm near gall bladder fundus was observed, which had mass effect. Multiple lymph nodes in porta hepatis, para aortic, peripancreatic, and around common iliac vessels were noted, most of which were necrotizing. Multiple hypoechoic lesions were seen in the liver.
Abdominal computed tomography (CT) confirmed these data (Figure 1). Also, endoscopic retrograde cholangiopancreatography (ERCP) was performed for the patient, but it was normal and could not help with neither definite diagnosis nor treatment. Biopsy of the cervical lymph node was carried out, the results of which revealed accumulation of histiocytes, eosinophils, and polymorphonuclear leukocytes (PMN), therefore, it was not diagnostic.
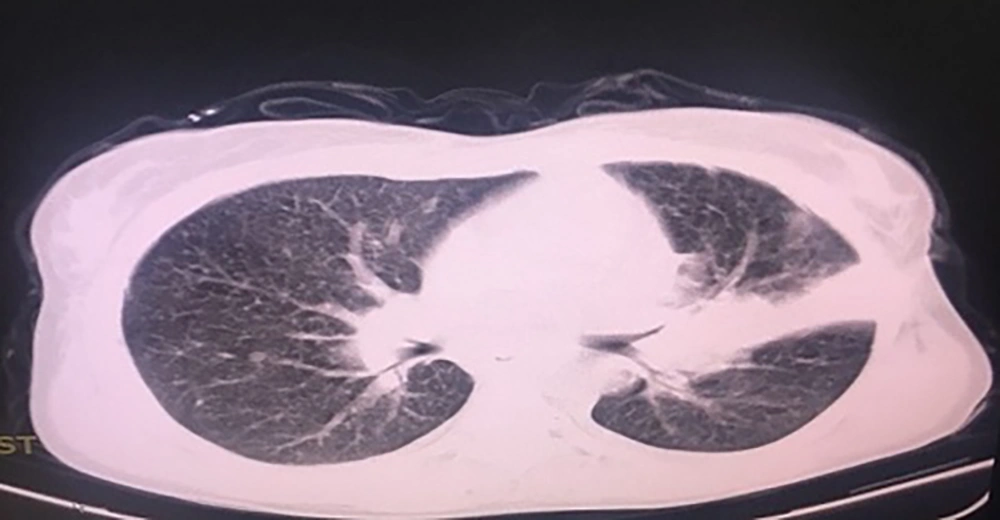
Smear, culture, and polymerase chain reaction (PCR) for tuberculosis were negative and branching filament suggested Nocardia infection. According to negative acid-fast bacillus and ruling out malignancies (lymphoma) and because of eosinophilia and hypointense masses with the possibility of parasitic causes (Fasciola hepatica) triclabendazole was started for the patient. The symptoms briefly improved and she had little weight gain, but four months later she was hospitalized with pulmonary symptoms such as cough and shortness of breath. Chest CT was performed and miliary pattern was observed (Figure 2). Culture and sputum smear were positive for acid-fast bacilli. Anti-tuberculosis treatment was started with the standard four-drug regimen (i.e., isoniazid, rifampin, pyrazinamide, and ethambutol). Generally, the patient recovered completely after two months, and four months after starting treatment, the patient got pregnant.
3. Discussion
The prevalence of tuberculosis is increasing in the developed countries (10), but biliary involvement is an extremely rare (2, 11, 12) form of hepatic tuberculosis. It has delayed presentations with nonspecific manifestations. Various forms of it occur such as local, miliary, and tuberculoma or granulomatous tuberculosis of the liver (12). The most common symptom is fever followed by abdominal pain, and hepatomegaly is the most common abnormality found on clinical examination. Liver function tests are often near normal and therefore not diagnostic (11). Highly variable imaging findings may present in hepatobiliary tuberculosis such as nonspecific hepatomegaly, abscess formation, or solid focal lesions, like hepatic tumors. Biliary tract involvement with ductal dilatations from underlying strictures may also be detected (13). With complete anti-tuberculous treatment, the prognosis is good.
Range of mortality for hepatic tuberculosis is between 15% and 42% (12). One study has reported a mortality rate of 42% (14). Respiratory involvement and ruptured esophageal varices due to associated cirrhosis were the cause of approximately 50% of deaths in a study performed in the Philippines, while hepatic failure is not a usual cause of death from hepatobiliary tuberculosis. The risk factors with poor prognosis are miliary tuberculosis, concurrent steroid therapy, age less than 20, cachexia, HIV, associated cirrhosis, and liver failure (12).
In our patient, despite the clinical presentations matched those of hepatobiliary tuberculosis, multiple biopsies from abdominal and peripheral lymph nodes could not verify it. The eosinophilia was really unusual for tuberculosis and tuberculin skin test was negative too. Therefore, diagnosis was made with delay, and finally, pulmonary presentation and positive smear for acid-fast bacilli confirmed tuberculosis. Albeit, miliary tuberculosis was proposed for her, and after treatment her condition improved and prognosis was acceptable.