1. Background
Over the past decades, the development and spread of resistance in bacterial pathogens and the identification of their genetic determinants has become a global health concern throughout the world (1). The latest report by the World Health Organization (WHO) showed high levels of resistance in a number of serious bacterial infections in both developed and developing countries. One of the major resistant bacteria is Staphylococcus aureus, a common pathogen in both hospital and community that is capable of causing skin and soft tissue infections as well as other life-threatening infections and has gradually evolved towards resistance to many classes of antibiotics (1-3).
Particularly, burns patients due to the disruption of protective barriers and reduction of cellular and humoral immunity are at high risk for infection and colonization with S. aureus strains (4). Dissemination of resistance among S. aureus isolates leads to therapeutic challenge and dramatic clinical outcomes. In burns patients, one of the major impediments regarding the treatment of S. aureus infections is the increasing emergence of methicillin-resistant S. aureus (MRSA) strains (5). Nowadays, in order to treat burn wound infections caused by MRSA and eradicate MRSA nasal carriage in patients and healthcare workers, the use of mupirocin has widely increased. It appears that mupirocin can significantly reduce MRSA carriage in healthcare workers and patients (6).
Mupirocin, a topical antimicrobial agent with protein synthesis inhibitor activity, is used for the elimination of MRSA strains in patients and healthcare staff. According to the literature, two types of phenotypic resistance to mupirocin are described: (i) Low-level mupirocin resistance (LLMUPR) with minimum inhibitory concentrations (MICs) of 8 - 256 µg/mL and (ii) high-level mupirocin resistance (HLMUPR) with MIC ≥ 512 µg/mL. HLMUPR has been associated with the acquisition of a plasmid-borne mupA or isoleucyl-tRNA synthetase (IRS) gene (iles) that encodes an additional modified IRS with reduced affinity for mupirocin, while LLMUPR is linked to point mutations in the native iles. A related gene, mupB, has also been shown to confer high-level resistance to mupirocin (7).
Dissemination of antibiotic resistance genes through the horizontal gene transfer mechanisms is mediated by mobile genetic elements such as plasmids and transposons. In recent years, the role of integrons as a key system involved in spreading antibiotic multi-resistance has been well established. Based on the homology of integrase gene, several classes of integrons which are related to antibiotic multi-resistance have been described. Among the classes of integrons, class 1 and 2 are often identified in clinical isolates of S. aureus. Reports are limited to other classes of integrons (8).
Due to the increase in the prevalence of S. aureus infections in burns patients, identifying the molecular characteristics and resistance patterns of this bacterium is necessary. Despite the existence of different techniques for S. aureus typing, it is believed that polymerase chain reaction (PCR)-based methods such as spa typing can be advantageous for typing S. aureus isolates because of their cost-efficiency, rapidity and high throughput capability (9).
2. Objectives
There is a scarcity of data regarding the molecular characteristics and integron prevalence of MRSA strains isolated from burns patients in Tehran, Iran. Therefore, the present work was designed to determine the molecular characterization, the prevalence of integrons, and the pattern of antimicrobial resistance in the MRSA strains in a referral burns hospital in Tehran, Iran.
3. Methods
3.1. Study Design and Bacterial Isolation
In this cross-sectional research, 64 consecutive MRSA isolates were gathered from burns patients admitted to a burns center in Tehran from January 2017 to April 2018. All the S. aureus strains were obtained from burn wounds and cultured on sheep blood agar (BA; Merck, Germany) and mannitol salt agar media (MSA; Merck, Germany) after transfer to the laboratory of Shahid Beheshti University of Medical Sciences. The study protocol was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU. RETECH. REC.1397.246). Bacteriological testings including colony morphology and hemolysis patterns on blood agar, Gram staining, coagulase, catalase, and DNase tests, and mannitol fermentation were used for preliminary identification. nucA gene was detected by PCR assay to confirm the results as previously described (10).
3.2. Mupirocin Resistance Screening
Confirmed S. aureus isolates were subjected to mupirocin resistance screening. For this purpose, S. aureus isolates were evaluated for mupirocin sensitivity by 5-µg mupirocin disc (Mast, UK) as the first step. Isolates were categorized as i) mupirocin susceptible if inhibition zone diameter was ≥ 14 mm, which were excluded from our study and ii) mupirocin resistant if inhibition zone diameter was ≤ 13 mm, which were subjected to the broth microdilution method to determine MIC titer. Particularly, the isolates with MIC values between 8 and 256 µg/mL were considered as LLMUPR phenotype; on the other hand, the MIC value ≥ 512 µg/mL was considered a HLMUPR phenotype (11). Isolates with MIC < 4 μg/ML were interpreted as sensitive. All mupirocin-resistant isolates were investigated for the presence of mupA and mupB genes by utilizing PCR, as previously described by Goudarzi et al. (10). Mupirocin-resistant isolates were stored in Tryptic Soy Broth (TSB; Merck, Germany) containing 20% glycerol at - 70°C for further investigation.
3.3. Disc Diffusion Susceptibility Testing
Antimicrobial sensitivity testing was performed by the Kirby-Bauer method for the following antibiotics: Amikacin, ciprofloxacin, clindamycin, erythromycin, gentamicin, kanamycin, linezolid, quinupristin-dalfopristin, rifampicin, tetracycline, teicoplanin, tobramycin, and trimethoprim-sulfamethoxazole. The MICs for vancomycin and fusidic acid (Sigma-Aldrich, St. Louis, Mo) were determined by the broth microdilution test. The entire procedures were performed and the breakpoints were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) (11), with the exception of fusidic acid which was interpreted according to the European Committee for Antimicrobial Susceptibility Testing (EUCAST) guidelines.
MRSA screening was carried out by using 30-µg cefoxitin discs on Mueller-Hinton agar (Merck, Germany) plates supplemented with 4% NaCl. Consequently, the findings were interpreted after overnight incubation at 37°C according to the CLSI guidelines (11). Isolates with positive phenotypic results for MRSA screening were subjected to PCR assay in order to detect the mecA gene, as described elsewhere (12). As instructed by the CLSI (11), isolates were susceptible to clindamycin; nonetheless, they were resistant to erythromycin which showed the flattening of the clindamycin zone towards erythromycin (D zones) were considered as inducible macrolide, lincosamide, and streptogramin B (iMLSB) phenotypes.
Constitutive MLSB (cMLSB) phenotype was defined for strains that showed resistance to both erythromycin and clindamycin with circular clear zone, if any, around clindamycin. MS phenotype (macrolide and streptogramin type B) was defined when isolates were resistant to erythromycin and sensitive to clindamycin with a circular zone of inhibition around clindamycin without D zone formation. To confirm all the three detected phenotypes, was subjected to microbroth dilution test according to the CLSI recommendation (11). Multidrug-resistant (MDR) phenotype was defined as MRSA to three or more unique antimicrobial categories in addition to beta-lactam (10). In each susceptibility experiment, reference strains S. aureus ATCC25923 and ATCC29213 were used as control.
3.4. Genomic DNA Preparation
Total genomic DNA was extracted from an overnight pure culture of S. aureus strains on 5% sheep blood agar (BA; Merck, Germany) by using phenol-chloroform extraction. Briefly, one to five bacterial colonies were suspended in 100 µL of lysis solution containing 1% Triton and 20 μL of 1 mg/mL lysostaphin (Sigma-Aldrich, USA) as recommended by Asiimwe et al. (13). The purity of DNA was measured by using NanoDrop (Thermo, USA). The extracted DNA was eluted in 200 µL of elution buffer (10 mM Tris-Cl, 0.5 mM EDTA [pH 9.0]) and stored at - 20°C until use.
3.5. Amplification of Integrase Gene and PCR-Restriction Fragment Length Polymorphism Analysis
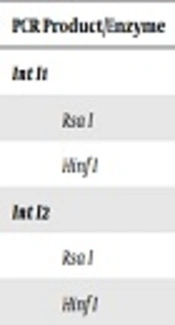
Conventional PCR was applied for the detection of a conserved region of integron-encoded integrase gene utilizing specific degenerated primers as described by Japoni et al. (14). Positive PCR products in terms of the presence of integrase gene were subjected to restriction fragment length polymorphism (RELP) method by using the two restriction enzymes of Rsa I and Hinf I. RFLP reaction was performed as described by Japoni et al. (14) and different classes of integrons were defined based on the pattern of generated fragments presented in Table 1.
| PCR Product/Enzyme | No. of Fragment | Fragment Size (s) (bp) |
|---|---|---|
| Int I1 | ||
| Rsa I | 1 | 491 |
| Hinf I | 1 | 491 |
| Int I2 | ||
| Rsa I | 2 | 334, 157 |
| Hinf I | 2 | 300, 191 |
| Int I3 | ||
| Rsa I | 3 | 97, 104, 290 |
| Hinf I | 2 | 119, 372 |
3.6. Molecular Analysis
Spa typing of the isolates was performed as described by Harmsen et al. (9). Positive spa PCR products were purified and subjected to DNA sequencing for both strands by Macrogen (Macrogen, South Korea). Sequence edition was performed through Chromas software (version 1.45, Australia). Th edited sequences were assigned to specific spa types by utilizing the Ridom Spa Server database (http://www.spaserver.ridom.de).
3.7. Statistical Analysis
Statistical analysis was performed using SPSS, version 18.0 (SPSS Inc., Chicago, IL).
4. Results
All the isolates were found to be MRSA in the phenotypic and genotypic assays. The results for antimicrobial susceptibility testing revealed that the majority of the investigated isolates were resistant to tetracycline (55; 85.9%), followed by erythromycin (48; 75%), amikacin (48; 75%), gentamicin (42; 65.6%), kanamycin (39; 60.9%), ciprofloxacin (33; 51.6%), clindamycin (21; 32.8%), trimethoprim- sulfamethoxazole (18; 28.1%), tobramycin (17; 26.6%), rifampicin (15; 23.4%), and quinupristin-dalfopristin (7; 10.9%). A total of 64 mupirocin-resistant isolates did not display any resistance to linezolid, teicoplanin, vancomycin, or fusidic acid. Out of 64 tested isolates, 37 exhibited resistance to 5 (57.8%) antibiotics followed by 6 (40.6%) antibiotics simultaneously.
All the mupirocin-resistant isolates were inhibited by fusidic acid at similar MIC50 and MIC90 of 0.25 µg/mL. The results of MIC50 and MIC90 for vancomycin were found to be 1 and 2 µg/mL, respectively. The cMLSB and iMLSB phenotypes were detected in 21 (32.8%) and 25 (39.1%) isolates, respectively. MS phenotype was only detected in 2 (3.1%) isolates. Out of the 64 S. aureus strains confirmed as mupirocin resistant by microdilution and disc diffusion methods, 24 (37.5%) carried high-level resistance, while 40 (62.5%) isolates were categorized as having low-level resistance. All the isolates displayed the same results in both disc diffusion and microbroth dilution methods. All the 24 HLMUPR strains harbored the mupA gene. No mupirocin-resistant isolate harbored the mupB gene.
Spa analysis of the mupirocin-resistant isolates revealed six different types including t860, t790, t037, t064, t008, and t631 among the examined isolates. Spa typing also revealed that high-level mupirocin resistance was present in multiple spa types, namely t037 (11/64; 17.2%), t064 (11/64; 17.2%), t008 (1/64; 1.6%), and t631 (1/64; 1.6%), while low-level mupirocin resistance was present in t860 (26/64; 40.6%) and t790 (14/64; 21.8%). Surprisingly, all MRSA t037 isolates showed iMLSB phenotype. The 13 remaining iMLSB phenotypes were t860 (6 isolates), t790 (5 isolates), and t064 (2 isolates).
Regarding integron frequency, our results indicated that class 1 integron was present in 38 (59.4%) isolates, class 2 in 11 (17.2%) isolates, and both class 1 and 2 integrons in 4 (6.2%) isolates simultaneously. All the strains carrying class 2 integron belonged to t037, while isolates carrying both class 1 and 2 integrons belonged to t064. Out of 38 isolates carrying integron class 1, 22 (57.9%) isolates belonged to t860, 9 (23.7%) isolates belonged to t790, and 7 (18.4%) isolates pertained to t064.
5. Discussion
The present survey yielded several outcomes regarding the MRSA strains isolated from burns patients. Primarily, all the HLMUPR strains obtained from patients were found to carry the mupA gene. Secondly, MRSA strains were broadly resistant to tetracycline (85.9%), erythromycin (75%), amikacin (75%), gentamicin (65.6%), kanamycin (60.9%), and ciprofloxacin (51.6%), whereas they had greater sensitivity to quinupristin-dalfopristin (10.9%). Thirdly, MRSA strains displayed a high diversity with a predominance of t860 (40.6%) followed by t790 (21.9%), t037 (17.2%), t064 (17.2%), t631 (1.6%), and t008 (1.6%). Eventually, our analysis demonstrated a high prevalence of class 1 in t860 spa type strains and class 2 integrons in t037 spa type strains.
Iran remains one of the regions with the most antibiotic overuse; as a consequence, the increasing emergence of resistance to the available antimicrobial agents among MRSA strains has limited the choice for therapeutic options; furthermore, this issue has become a dilemma for the future treatment of MRSA infections (3). Therefore, novel strategies and medications are needed for the control of infections caused by MRSA strains (3, 15). In general, there is a significant relationship between accurate susceptibility data and appropriate treatment decisions (3). In the present work, more than half of the strains were resistant to tetracycline (85.9%), erythromycin (75%), amikacin (75%), gentamicin (65.6%), kanamycin (60.9%), and ciprofloxacin (51.6%), which is in agreement with the results of the previous studies from Iran (10), Italy (15), China (16), Turkey (17), and Ko et al. study in Asian countries (18).
In fact, the improper use of tetracycline and erythromycin, which are often prescribed as antibiotics in Iran, may be the primary reason for the high level of resistance taking place in Iran (10). However, some previous findings regarding the resistance rate among MRSA strains are different from our results, which could be possibly due to the size and type of our clinical samples, cultural, geographic, social, and economic factors, infection control policies and unrestrictive policies in the use of these antimicrobial agents in our country. In accordance with a study that reported a low frequency of resistance to quinupristin-dalfopristin among MRSA strains (10), our study also indicated low resistance to quinupristin-dalfopristin in 10.9% of the tested isolates. This finding distinctly suggests trimethoprim-sulfamethoxazole as a suitable first-line therapeutic option against MRSA strains, which could be used for the empirical treatment of wound infections associated with this bacterium.
Although the recent published data indicated a significant increase in the emergence of MRSA with reduced susceptibility to vancomycin in Iran (19), findings of the present study revealed that all the MRSA isolates were susceptible to vancomycin. These findings can indicate the role of limited and appropriate use of vancomycin, proper antibiotic management and clear prescription protocols in Iranian hospitals. Although resistance to fusidic acid among MRSA isolates has been pointed out by several researchers, similar to studies conducted by Aschbacher et al. (15) in Italy and Otokunefor et al. (20) in the UK, our results showed that none of the investigated isolates was resistant to fusidic acid, which reflects the fact that fusidic acid could be an appropriate choice for the treatment of wound infections associated with S. aureus (21).
As previously stated, failure to identify the inducible phenotype may lead to clinical failure of clindamycin therapy (22). In this experiment, MS, cMLSB, and iMLSB phenotypes were present in 3.1%, 32.8% and 39.1% of the isolates, respectively. Similar results were obtained by Fiebelkorn et al. (23). They reported the prevalence rates of 34% and 29% for cMLSB and iMLSB phenotypes, respectively. Lavallee et al. also reported that 64.7% and 35.3% of isolates had iMLSB and cMLSB phenotypes, respectively (24). In a study, the incidence of clindamycin resistance in S. aureus strains recovered from clinical specimens in Turkey was investigated. That study reported cMLSB, iMLSB, and MLSB phenotypes in 23%, 18%, and 48% of tested isolates, respectively (25).
As previously stated, integrons are the key systems involved in spreading antibiotic multi-resistance among pathogenic bacteria. In this experiment, class 1 integron was present in more than half of the strains (59.4%), while class 2 integron was encountered in 17.2% of the isolates. These findings indicate that class 1 integrons are more prevalent than class 2 integrons in clinical isolates; apparently, the data is in accordance with the results of Marathe et al. (26). They reported the prevalence of MRSA isolates harboring class 1 integrons was 71%. In a previous study, we detected class 1 and 2 integrons in 72.6% and 35.2% of S. aureus strains isolated from clinical samples, respectively (8). In 2007, Xu et al. in China reported 53% of S. auerus strains isolated from environment and surgical patients were integron-positive (27). The findings of a study carried out in Iran on 106 MRSA isolates isolated from burn wound infections also showed that the majority of the isolates harbored integron class 1 (54.7%) (12), while class 2 integron was presented in 3.8% of the isolates. It is worth mentioning that the current findings are contrary to the findings of Guney from Turkey (17). They reported that none of the tested isolates contained class 1 integron. Recent evidence support the hypothesis that class 1 integron may serve as a reservoir for antimicrobial resistance in MRSA strains. Discrepancies in the prevalence of integron classes can be attributed to the different geographic regions, the bacterial strains, or indiscriminate and overuse of antibiotics.
In the present work, the predominant spa type was t860, which was present in 40.6% of the isolates. All the t860 isolates exhibited the LLMUPR phenotype and carried integron class 1 with the multi-resistant pattern. In a similar study performed by Vali et al., carriage rate of 5.8% for t860 with the multi-resistant pattern and mupirocin resistance was found (28). Boswihi et al. in a study conducted from 1992 - 2010 in Kuwait also reported a low prevalence of t860 (4.5%) among their tested isolates, which were not resistant to mupirocin (29). This result suggests the dissemination of spa type t860 among clinical MRSA strains in our region.
Our results imply that 21.8% of the tested isolates belonged to t790, the second most common spa type detected, which is in line with previous studies conducted in Iran (10, 12). It is remarkable that in the present experiment, all the t790 isolates exhibited LLMUPR phenotype and carried integron class 1. According to the results of the previous studies from other countries, spa type t790 was found in both LLMUPR and HLMUPR-phenotype MRSA strains (29-31). It is generally accepted that spa type t790 is the predominant type in CA-MRSA strains (29, 30). Based on the obtained results, it is inferred that the high prevalence of t790 among the clinical LLMUPR-MRSA strains in the present study could be due to their transfer from the community to hospitals.
Spa type t037 was detected in 17.2% of MRSA isolates. This spa type has been previously reported in Saudi Arabia, China, Iran, and among HA-MRSA isolates in Europe, the United States and several Asian countries (10, 29, 30, 32). In the present study, we showed that all t037 isolates harbored class 2 integron and displayed high-level resistance to mupirocin and carried mupA gene. In an Iranian study on 106 MRSA isolates recovered from burn wound infections during a 7-month period, t037 was detected in 14.2% of isolates, out of which five isolates were resistant to mupirocin (12).
Another HLMUPR-MRSA type with reduced susceptibility to clindamycin was t064 (17.2%). In a study regarding clonal distribution of MRSA isolates in 13 public hospitals in Kuwait during a 12-year period, Boswihi et al. (29) reported spa type t064 with HLMUPR pattern and different resistance patterns. Similar observations about this spa type have been presented before (30, 33).
In the present study, we demonstrated the same frequency of spa types t008 and t631 harboring the mupA gene (1.6%). Many studies in Switzerland, Japan, Hong Kong, Australia, Spain, Kuwait, and the United Arab Emirates (29, 30) have noted similar distributions of t008 isolates. In a study conducted in 2017 in Iran by Goudarzi et al. (10), it was found that HLMUPR-MRSA strains belonged to ST15-SCCmec IV/t084 (40%), ST22-SCCmec IV/t790 (23.3%), ST239-SCCmec III/t631 (20%), and ST239-SCCmec III/t030 (16.7%) clones. In this study, it was shown that all the ST239-SCCmec III/t631 strains harbored the mupA gene, which is consistent with the studies of Abimanyu et al. (34) and Boswihi et al. (29) who reported high-level mupirocin resistance in the MRSA ST239 clone. Similar to the data from the previous studies, we found that none of the isolates contained class 3 integron (12).
In sum, MRSA isolates are genetically diverse. The most frequent integron detected in our study was class 1, which probably facilitates the dissemination of resistance to mupirocin among MRSA strains. In fact, the increase in the prevalence of mupirocin resistance and MDR-MRSA strains associated with integron indicates that molecular typing data could be applied to evaluate the significance of distribution of these integron-bearing MRSA isolates and their clonal relationships in the future.