1. Introduction
Progressive multifocal leukoencephalopathy (PML) is a fatal neurological disease, and is also a severe demyelinating disease of the central nervous system (CNS) caused by the JC virus (JCV) (1). The JC virus is a polyomavirus in the Polyomaviridae family, characterized by being small, non-enveloped, double-stranded DNA viruses (2). This virus occurs in immunosuppressed individuals and most of them have advanced human immunodeficiency virus (HIV) infection. In the absence of HIV infection, PML is found in hematological and solid organ malignancies, sarcoidosis, autoimmune disorders, and congenital immune deficiencies, followed by the introduction of biological agents (3).
The initial symptoms of PML can vary from patient to patient, but its predominant symptoms include coordination difficulties, cognitive dysfunction, gait imbalance, visual problems, and limb paresis. The optic nerves and the spinal cord of the CNS are usually spared in this disease. The diagnosis of PML can be established via a histopathologic demonstration of JCV infection in the brain, clinical and radiologic findings, or demonstration of the JCV DNA by the polymerase chain reaction (PCR) in the cerebrospinal fluid (CSF) (4).
The prevalence of PML frequently increases during acquired immune deficiency syndrome (AIDS) epidemics, where up to 5% of AIDS patients may develop the disease (5). Here, we report a case of progressive multifocal leukoencephalopathy as the first manifestation of AIDS. To our knowledge, this case is the first report from Iran. A comprehensive search of electronic databases (PubMed, Scopus, Web of Science, and Google Scholar) was conducted, as well. Searches were confined to the literature using the following search terms: (progressive multifocal leukoencephalopathy or PML) and (acquired immunodeficiency syndrome or AIDS).
2. Case Presentation
A 47-year-old woman was admitted first to the Emergency Department and then to the Neurology Department and finally to the Infectious Department. She had a loss of consciousness, aphasia, and right hemiparesis. Her clinical history showed that she had been admitted to another hospital with right hemiparesis and dysarthria a month earlier. At that time, her right motor force was 2.5 vs. 5.5 for her left motor force on the physical examination.
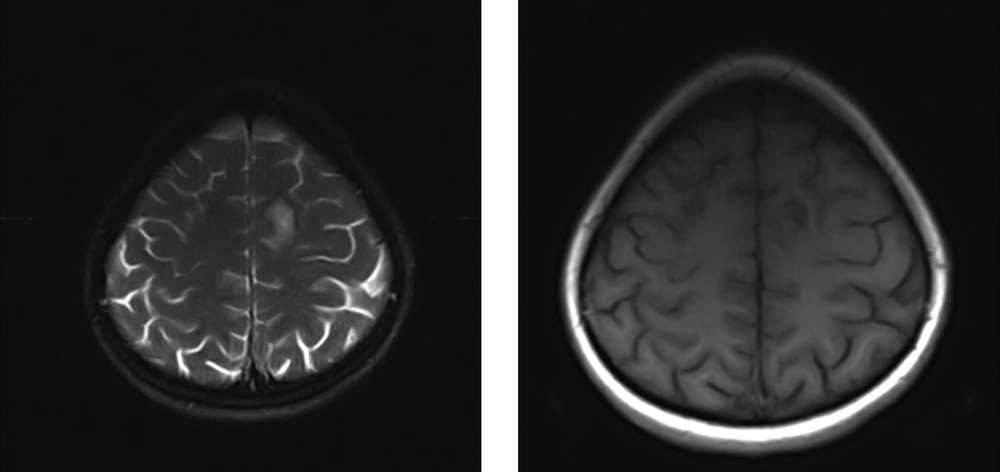
Brain magnetic resonance imaging (MRI) was performed for her at previous hospital admission (Figure 1). The first study showed a focal subcortical white matter with an abnormal intensity that involved U-fibers in the left superior frontal gyrus as T1 low and T2/FLAIR high intensity without the mass effect that did not show the signs of diffusion restriction in DWI sequences. This focal white matter abnormality was not specific to any white matter pathology to allow the detection of subacute neurological deficit symptoms, but the possibility of a demyelinating lesion or embolic ischemia was brought up. Magnetic resonance imaging with contrast and magnetic resonance spectroscopy (MRS) were also recommended for better characterization.
One month later, MRS was performed; the results showed an increased peak of choline although the choline-containing metabolites (Cho)/creatine (Cr) ratio and choline/N-acetyl aspartate (NAA) ratio did not correspond to the tumoral nature of the lesion, and subacute infarction and demyelinating plaques were debated. Since the patient’s symptoms were progressive, she was referred to our center with aphasia, loss of consciousness, and progressive hemiparesis. She was unconscious (a state of semi-coma) with mid-sized reactive pupils and a Babinski sign on the right side and showed grimaces with painful stimuli.
The patient had no history of drug or alcohol consumption. On the physical examination, she was afebrile. The results of fundoscopy, liver and kidney function test, and echocardiography were normal. The laboratory data revealed a white blood cell (WBC) count of 3,400, hemoglobin (Hb) count of 13.4, and platelet (PLT) count of 228,000. The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were 50 mm/h and 2 mg/dL, respectively.
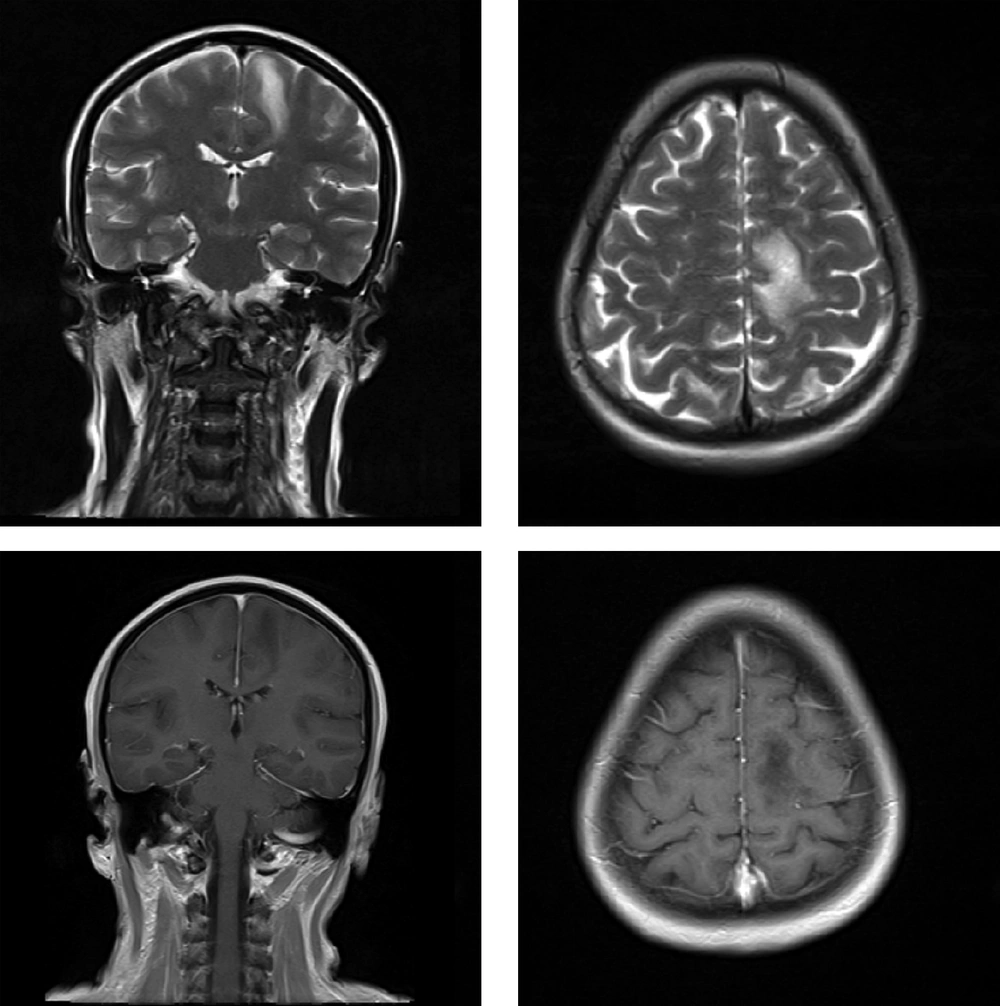
The patient underwent another brain MRI with IV contrast (Figure 2). The results showed a progression in the disease in the form of the involvement of nearly the whole high left cerebral convexity (white matter) in both subcortical and centrum semiovale with U-fiber involvement. In addition, T2-hyperintense foci in the body of the corpus callosum and the right parasagittal subcortical region were noted as the locations of new lesions with no mass effect and enhancement or diffusion restrictions. When these white matter abnormalities set in two months, subacute encephalitis was the most likely possibility although neoplastic causes such as gliomatosis cerebri were also possible.
At this time, HIV testing was requested. The laboratory studies revealed positive HIV-1 serology. This test was confirmed by Western blotting, as well. The serum CD4 count and HIV viral load were 22 and 319,032 IU/mL, respectively. In addition to the initiation of antiretroviral therapy (ART), prophylaxis with Azithromycin and Co-trimoxazole also started. A lumbar puncture was then carried out based on this finding. The toxoplasma antibody was negative with both IgG and IgM ELISA methods. The analysis of CSF revealed red blood cell = 0, white blood cell = 0, protein = 39, and glucose = 67. The CSF smear and culture were also negative. The CSF cytology, VDRL and PCR studies for Epstein-Barr virus, cytomegalovirus, and toxoplasmosis were all negative, as well. Nonetheless, the CSF PCR for JCV was positive and thus, the diagnosis of PML was established. Combined-ART, including Truvada and Raltegravir, also started. The patients’ symptoms ultimately exacerbated and she did not survive.
3. Discussion
Progressive multifocal leukoencephalopathy is an uncommon demyelinating multifocal disease of the CNS caused by the ubiquitous JC virus and characterized by widespread lesions due to the infection of the oligodendrocytes; it has a high mortality and morbidity rate, mostly in immunocompromised patients (6). The AIDS pandemic may lead to a much higher incidence of PML (7). This study reported a patient with AIDS who presented with severe PML. In our opinion, given the ever-increasing HIV patients, it is important to recognize PML manifestation. Progressive multifocal leukoencephalopathy is a rare disease that its exact pathogenesis is still unknown. Three factors, i.e., the host, the virus, and the immune response, are likely responsible for the low expression of clinical disease. Progressive multifocal leukoencephalopathy is the result of the reactivation of a latent infection rather than of initial infection (8).
The diagnosis and management of PML have become a major health concern. Its clinical presentation includes progressive focal neurological dysfunction. Aphasia/dysarthria, monoparesis, hemiparesis, ataxia, cortical blindness, and visual field defects are commonly reported. Mental status changes such as confusion, dementia, and even coma are seen (9). This patient had a loss of consciousness, aphasia, dysarthria, and right hemiparesis.
We found five case-reports of AID- related PML. Most cases diagnosed with this disease are male and only one case was treated (Table 1) (7, 9-12). The diagnosis of PML is based on three stages: clinical suspicion, radiological identification, and etiological confirmation by CSF or tissue analysis (9, 12). This patient was diagnosed with PML by clinical presentation, PCR for the JC virus in CSF, and brain MRI. Although the survival of patients with PML has improved in recent years due to advances in diagnostic techniques and the widespread use of combined ART, the mortality rate associated with this condition is about 50% in HIV-infected patients (1). The patient examined in this study also began combined ART; however, her symptoms progressed. In summary, PML results from brain infection with JCV and it is usually rapidly fatal in cases of HIV infection (12). Our case died like other cases.
| Case No. (Ref.) | Year | Country | Sex | Clinical Presentation | Diagnosis | Outcome |
|---|---|---|---|---|---|---|
| 1 (9) | 2018 | India | Man | Weakness of the left half of the body and deviation of the mouth to the right side | AIDS-related possible PML | Death |
| 2 (10) | 2013 | Japan | Man | Weakness in all limbs | AIDS-related PML | Death |
| 3 (11) | 2013 | Latin America | Man | Headache and generalized tonic-clonic seizures | PML presenting as IRIS in an AIDS Patient | Good clinical condition |
| 4 (12) | 2011 | Brazil | Man | Confusion and alteration of motricity and coordination | AIDS-related PML | Death |
| 5 (7) | 2007 | Taiwan | Man | General tonic-clonic seizure, upward gaze | AIDS with PML | Death |
Literature Review of Similar Cases
3.1. Conclusions
Progressive multifocal leukoencephalopathy should always be considered as an important differential diagnosis in patients with demyelinating brain lesions and HIV testing should be considered in these patients, as well. Although rarely the case, PML may be the first manifestation of AIDS.