1. Context
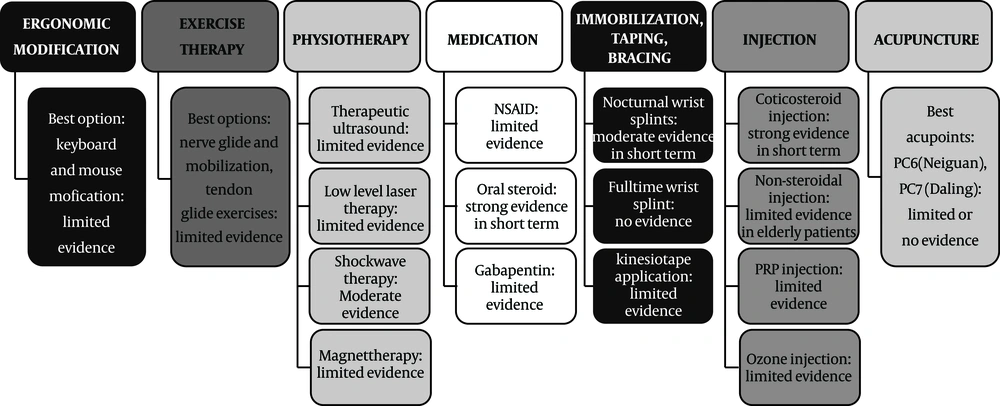
One of the most common forms of entrapment neuropathy in the general population and athletes is Carpal Tunnel Syndrome (CTS) (1). The prevalence of CTS is around 5% and 2% among adult women and men, respectively (2). In athletes, CTS is especially very common in sporting activities with repetitive wrist movements or vibration and heavy manual weights such as swimming, moto-cross-riding, and body-building (3). Various treatment options are available for management of CTS, and in persistent pain and dysfunction, carpal tunnel release is done. However, due to the lack of appropriate rehabilitation, pain and dysfunction could persist after the operation. The purpose of the present review was to classify the existing non-surgical treatments in the literature, such as ergonomic modifications, exercise therapy, physiotherapy, medications, immobilization, taping and bracing, injections, and acupuncture. In addition, post-surgery management and rehabilitation methods were summarized. The available treatment options were summarized and categorized in three sections (1) non-surgical managements of CTS (summarized in Figure 1), (2) post-operative management of CTS and (3) practical open carpal tunnel release post-op protocol.
2. Non-Surgical Management of CTS
2.1. Ergonomic Modifications
Although a plethora of conservative treatments are used for CTS, patients’ education and modification of incorrect positions should be considered as the first line of management by specialists. Patients can reduce their symptoms by changing their wrong ergonomic position as well as using ergonomically corrective tools. In order to treat CTS, ergonomic positioning or equipment intend to position the wrist in a neutral position and to prevent prolonged positioning of the wrist in flexion or extension where the median nerve passage is at its most capacious (4). However, studies on the efficacy of ergonomic treatments are few (5-8). A study by Annina et al., demonstrates that ergonomic mouse pads and a vertical mouse change wrist position but do not decrease CTS (9). Based on a recent Cochrane review, there is no strong evidence for using (or non-using) of ergonomic keyboards for the treatment of CTS (10). Overall, due to the lack of sufficient data from randomized controlled trials on the beneficial or detrimental effects of ergonomic treatment on CTS, no conclusions are made, and the choice of ergonomic tools is an individual preference.
2.2. Exercise Therapy
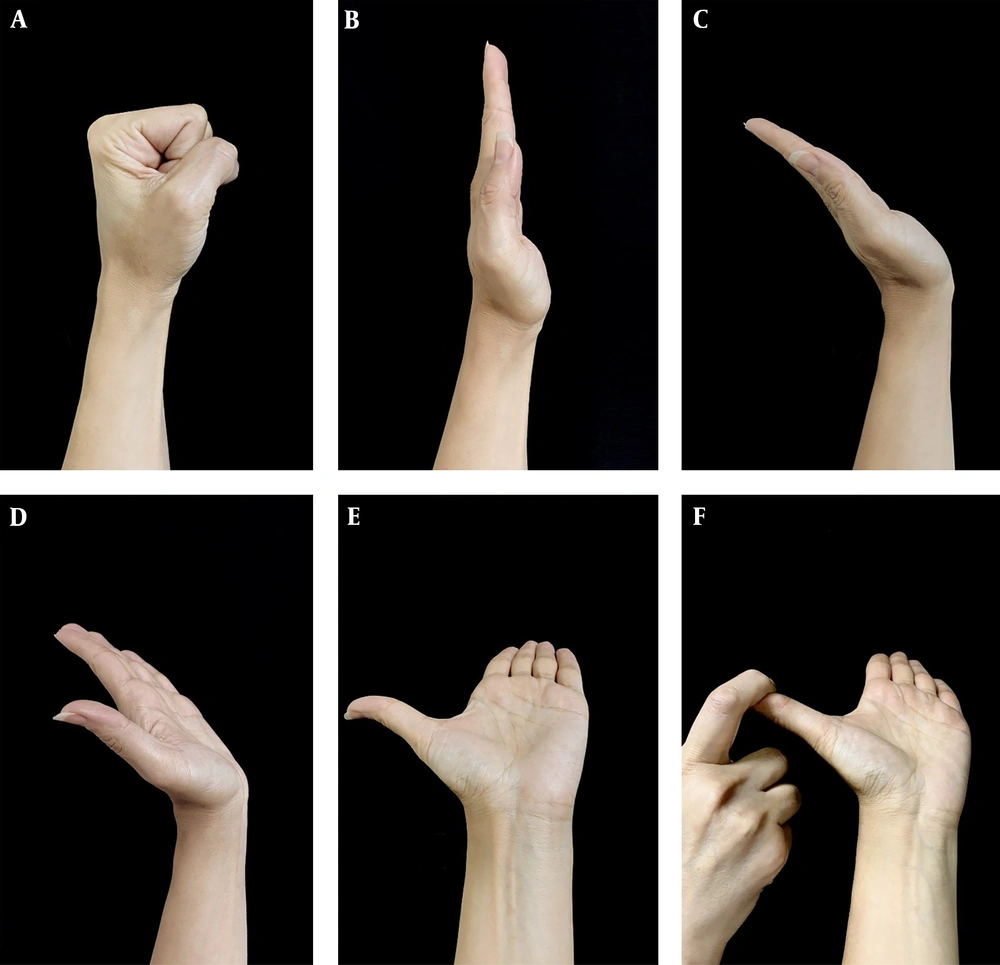
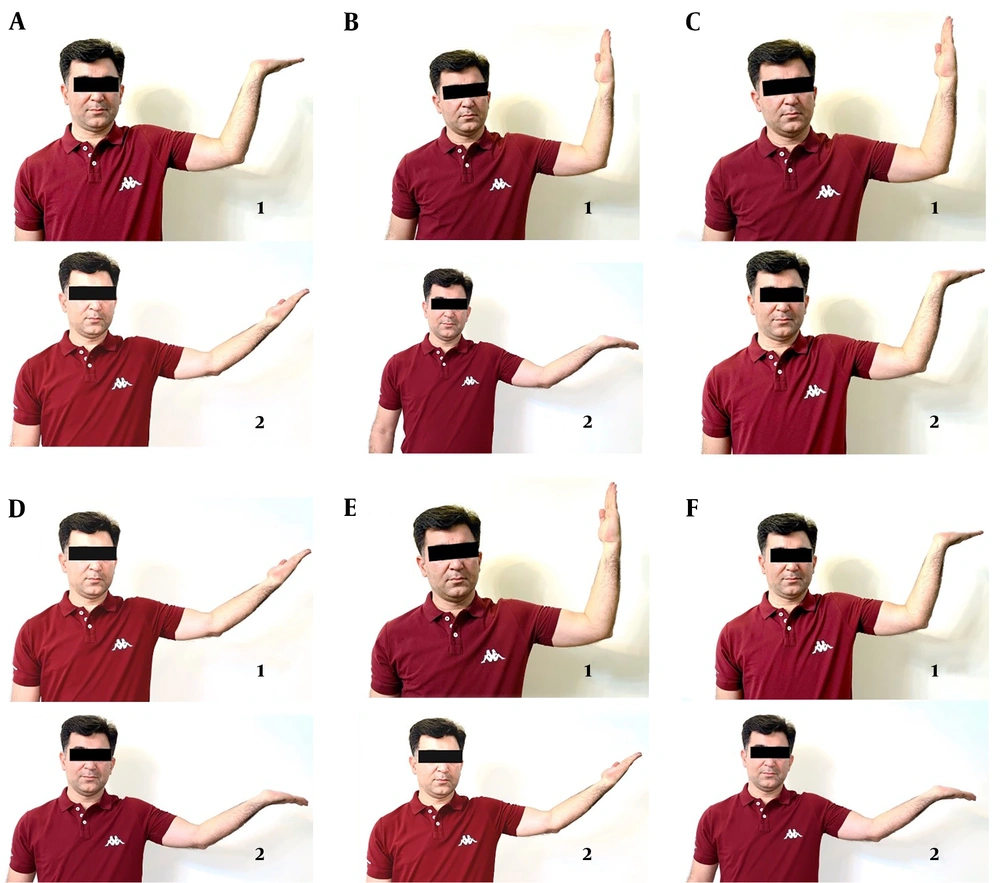
Exercise is recommended for mild to moderate cases of CTS or those waiting for surgery (11-15). Exercise decreases intracarpal pressure and inflammation and improves venous return by lowering edema and adhesions (12, 15, 16). However, studies on the impact of exercise therapy in CTS are limited. Moreover, a Cochrane review highlighted the poor quality of existing studies and concluded that exercise does not have any superiority over other non-surgical treatments. Moreover, exercise doesn’t resolve the need for operative interventions (15). However, several studies recommend that exercise in combination with other methods for short time pain relief in a specialized center under clinical observation may be beneficial (12-17). The most common exercises which are used for CTS, are median nerve glide mobilization and tendon glide. The recommended regimens, such as stretching and soft tissue exercises, should be performed one to five times per day with 5 - 10 repetitions (Figures 2-4). Nerve gliding exercises should be combined with adjacent joints mobilization to increase decompression of the nerve bed. A cautionary note is that the suggested exercises should be done in a manner that does not cause symptoms or increase tension on the nerve (11, 12, 18-21).
Totten and Hunter nerve gliding exercises (11) (A-F): “(A) wrist in neutral, fingers and thumb in flexion; (B) wrist in neutral, fingers and thumb extended; (C) wrist and fingers extended, thumb in neutral; (D) wrist, fingers, and thumbs extended; (E) as in (D) with the forearm in supination; (F) as in (E) with gentle stretch of thumb”.
Illustration of the six different mobilization techniques (11): “(A) sliding technique; (B) tensioning technique; (C) wrist motion with the elbow in flexion; (D) wrist motion with elbow in extension; (E) elbow motion with wrist in neutral; (F) elbow motion with the wrist in extension. The number 1 illustrates the starting position, and the number 2 illustrates the ending position. The techniques consisted of repeated movements between the starting and end position.”
2.3. Physiotherapy
A variety of different physiotherapy modalities such as ultrasound, magnet, and shockwave therapy are used for the treatment of CTS and are summarized below.
2.3.1. Therapeutic Ultrasound
According to a Cochrane review, the quality of evidence in comparing therapeutic US with placebo is poor in the short or long-term (22). In the field of comparing different types of therapeutic ultrasound, or comparing US with non-surgical interventions (such as exercise programs, oral drugs, etc.) for CTS treatment, there is insufficient evidence (22). Few studies reported no adverse effect of US (23-25).
2.3.2. Low-Level Laser Therapy
Low-level laser therapy is an alternative for other non-surgical treatments of CTS. However, according to the recent Cochran review, low-level laser therapy studies have poor quality and have little effect in treating CTS (26). Moreover, one study reported harmful laser therapy for CTS (27). Consequently, more data is required before any conclusions on the safety and efficacy of low-level laser therapy can be made.
2.3.3. Extracorporeal Shock Wave Therapy (ESWT)
There is moderate evidence for using radial ESWT versus placebo for short or long-term symptom relief in people with CTS (28, 29). On the other hand, there is no evidence for the short term effectiveness of ESWT versus a nutraceutical intervention or for the efficacy of short and midterm efficacy of ESWT versus a steroid injection (30).
2.3.4. Magnet Therapy
There are insufficient data to support the short term, midterm or long-term effectiveness of different types of magnet therapy (e.g., dynamic, static, or pulsed) versus placebo treatment (31-33). A comparative study in 38 CTS patients showed no effect of the magnetic field when compared to placebo on the symptoms of idiopathic CTS (34).
2.4. Medications
2.4.1. NSAID
There is no evidence on the efficacy of NSAIDs (non-steroidal anti-inflammatory drugs) on CTS symptoms when compared to placebo or the use of diuretics in the short term (35, 36).
2.4.2. Oral Steroid
There is strong evidence that short term use of oral steroids is more effective than a placebo (37). However, the therapeutic benefits of long-term use of steroids remains unknown (38-40). In some studies, short term oral steroid use was more beneficial than splinting the wrist for treating CTS (41).
2.4.3. Gabapentin
No evidence was found to support the therapeutic benefit of gabapentin (100 and 300 mg) compared to placebo (42), and there is limited evidence for its use as an additive to splinting in the short term (43).
2.5. Immobilization, Bracing, and Taping
2.5.1. Wrist Splint in a Neutral Position
The most common non-surgical treatment is wrist splint prescription, typically at night, and sometimes combined with other treatment modalities (2). The treatment of CTS with wrist splint has been compared with non-surgical treatments such as steroid injection or stretching exercises, in some randomized trials. Studies concluded a better clinical outcome in patients with mild to moderate CTS with a single steroid injection in primary care when compared to night splinting (2, 44-46). Concurrent application of splinting and nerve tendon glides was not more effective than splinting alone (47). On the other hand, a combination of splints and stretch exercises on lumbrical muscles was more effective than splints alone (33, 48, 49). In sum, the clinical effect of splinting or efficacy in comparison with other interventions for CTS treatment was supported only with limited evidence (50).
2.5.2. Nocturnal Wrist Splints
Results from several placebo-controlled studies favor the use of a nocturnal hand brace on symptom relief, hand function, and overall improvement during a 4-week follow-up (2, 44). Based on systematic reviews done so far, in the short-term use of nocturnal hand wrist splints as a therapy for the treatment of patients with CTS, there is moderate evidence. However, in the long-term, there is limited evidence (2, 51). Based on one RCT, steroid injection in local form caused further patient satisfaction and less analgesic use without more side effects in comparison with night splint (46, 52). Furthermore, there is no report for the superiority of using a full-time wrist splint in comparison to night splint in the treatment of CTS in the short term (51). It is concluded that a night splint is a valid treatment option, especially in patients not using medications.
2.5.3. Kinesiotaping
Today, Kinesio taping (KT) has become popular for several forms of musculoskeletal pain such as knee pain and shoulder pain (53, 54). By either inhibition or facilitation of the primary pathology, it provides support and protection to the intended muscle by allowing an efficient and safe range of motion (55, 56). Cochrane reviews related to KT in CTS patients but based on RCTs done so far are lacking. Pain improvement was noted with the KT application, but the best technique remains to be defined. Overall, there is limited evidence in favor of KT application for CTS patients (54).
2.6. Injection
Infiltrations have been studied and shown to cure symptoms, function, and patients’ perception of their wrist pain in CTS (47, 57, 58). The most commonly infiltrated drugs are prednisolone, methylprednisolone, dexamethasone sodium phosphate, triamcinolone acetonide, methylprednisolone acetate, and diclofenac diethyl ammonium (51, 59). The therapeutic effects of NSAID injections of carpal tunnel with lidocaine, ozone, Platelet-Rich Plasma (PRP), and dextrose water (DW) have been reported; however, the best doses and protocols for short-term prescription are still unknown (2, 47, 57, 60, 61).
2.6.1. Local Corticosteroid Injection
A clinical practice guideline published by the American Academy of Orthopedic Surgeons (AAOS) in 2009 indicated that corticosteroid injections cause significant symptom relief in CTS. However, improvement in symptoms did not persist (17, 58, 62, 63). Local injection of corticosteroid for a month in CTS patients provides greater clinical symptom relief when compared to placebo (45, 52). Longer treatments, however, are not effective (48). In a recent review of clinical trials, injection and night splinting are superior to only night splinting in mild or moderate CTS (45, 46). Corticosteroid injection produces the most rapid response option for relieving the symptoms (47).
2.6.2. Local Non-Steroidal Injection
According to a recent clinical trial, injection of lidocaine and normal saline in the carpal tunnel is as effective as low or high dose steroid medication in elderly patients with CTS (64). Multiple local injections of lidocaine were superior to a single injection in significant symptom reduction and electrophysiological improvement. Injection of DW exhibited a significant reduction in pain and disability through the 4th to the 6th month, (60). However, more research is needed to make a conclusion about the effectiveness of DW. In elderly patients, non-steroid injections may be a better option due to fewer adverse effects; however, further studies are needed.
2.6.3. Platelet-Rich Plasma Injection
Platelet-rich plasma (PRP) injection to the injured tissue with a high concentration of autologous growth factors enhances the self-healing ability of the body (65). Limited studies support the efficacy of PRP treatment in CTS. For example, a single perineural PRP injection into the carpal tunnel improved CTS symptoms (66). Malahias et al. showed very encouraging mid-term results (12 weeks) regarding the use of PRP for treatment in CTS patients (67). A single dose of PRP injection improves the Visual Analog Scale (VAS) pain score in CTS patients (67). Results of another high-quality RCT concluded that PRP injection in a single dose was significantly superior to local corticosteroid injection. Study outcomes were the improvement of the VAS pain score and functional domains at short and midterm follow-ups (68). Although the vast majority of the research so far confirmed that PRP improved the clinical outcomes of the patients and that PRP injection was useful for patients with mild-to-moderate CTS, the efficacy of PRP injection in CTS patients requires further clinical investigations (65, 69).
2.6.4. Ozone Injection
Recent studies have recommended local ozone therapy in some musculoskeletal conditions (70, 71). Rascaroli et al. showed that neurophysiological and functional parameters after O2-O3 treatment were improved significantly more than the motor and sensory nerve conduction parameters (72). The best clinical improvements were found in mild and moderate CTS groups (72). Although ozone therapy is a safe and low-cost method with some promising outcomes in patients with mild to moderate CTS, at least for short-term (70), further studies are needed in the future.
2.7. Acupuncture
There is little or no effect of acupuncture or laser acupuncture on the symptoms of CTS in the short term (3 months or less) when compared with placebo according to a Cochran review (73). It is unclear whether acupuncture is more or less effective in improving symptoms of CTS than other treatments such as nerve blocks alonside corticosteroids, oral drugs, or supplements such as corticosteroid, ibuprofen, vitamin B12, and other treatments such as splints (73). Acupuncture, however, was not associated with serious adverse events. Minor complications such as discomfort, pain, local paresthesia, and temporary skin bruises were reported (73). Common protocols involve Daling (PC7) and Neiguan (PC6) as primary acupoints (74).
3. Post-Operative Management of CTS
There is no consensus concerning clinical practice intervention and rehabilitation protocol used by therapists after carpal tunnel release (CTR). Additional studies with a larger sample size and greater power are required to distinguish statistically significant differences between interventions and determine the effects of different rehabilitation programs (75). A Cochrane review from the results of 22 trials with 1521 patients which compared different rehabilitation measures after surgery such as splint application, dressing, local treatment with cold and ice, exercise, applying a mixture of multiple rehabilitation therapies, laser, electricity, desensitization of the scar, and Arnica concluded that there were limited data with poor quality regarding the efficacy of these therapeutic measures as well as limited safety. Types of surgical intervention in the review were endoscopic (single or double portal); open; minimal-incision open (more common); and some other carpal tunnel surgery (including secondary procedures, such as epineurotomy, internal neurolysis, synovectomy or reconstruction of the transverse carpal ligament). The period of treatment ranged from 48 hours to 6 weeks. A summary comparing treatment methods is reviewed below. All studies show limited efficacy. However, the quality of experimental designs is poor (76).
3.1. Low-Level Laser Therapy
In a study between two groups (low-level laser therapy vs. sham therapy) no statistically significant differences were noted in numbness or palmar pain at three months and scar pain and pillar pain at six months follow up post-surgery (77).
3.2. Immobilization, Orthosis
Comparison between wrist immobilization with the orthosis and bulky dressing showed that there is no significant benefit on grip strength (kg), pinch strength, function, pain severity, the incidence of scar tenderness, or pillar pain (78-80).
3.3. Immobilization Versus Mobilization
In a study, the use of volar orthosis with the wrist in neutral position in addition to bulky dressing vs. light bandage dressing for 48 hr post-surgery, showed no significant difference in pain score, swelling, scar pain, excessive scaring, pillar pain, and neurophysiological parameters (81).
In addition, short and long period dressings showed no significant differences in functional improvement and symptom severity (79, 82, 83). Limited studies indicate that shorter post-operative dressing is associated with better grip strength (82, 83).
3.4. Elevation
In a study, home elevation device (with a Bradford sling intervention held over at night) and crepe sling in ambulatory position for five days after surgery was compared with standard care. There was no significant difference in pain score and swelling (84).
3.5. Ice Therapy
Ice therapy was compared to controlled cold therapy (CCT) immediately after CTR among 72 patients after surgery for CTS. Pain, edema, and the need for narcotics were significantly reduced in the CCT group. The authors suggested that using CCT instead of conventional ice therapy in this condition may be advantageous (85).
3.6. Electrical Stimulation
Gordon et al. compared the electrical stimulation of the median nerve 30 min after CTR for one hour versus no treatment. Zero-point and three months after surgery nerve conduction (using motor and sensory nerve conduction latency) were determined. Although there was no significant change in latency among the control group, motor latency was considerably accelerated in the early phase in the stimulation group 3 months after surgery. On the other hand, recovery of conduction velocity was delayed in the control group compared to the stimulation group who showed early recovery at 3 months (84).
3.7. Bath, Exercise
For post-operative edema control immediately after CTR, there were no significant differences in swelling, among the patients who receive bath plus exercise and those receiving bath alone (86).
3.8. Exercise
No significant difference has been shown between multi-modal hand therapy (including range of motion and strengthening sessions with 30 min of nerve gliding, and further treatments such as massage, fluid therapy etc.), and formal therapy regarding pain score, grip strength (kg), return to work and adverse events. However, it is found that multi-modal hand therapy improves lateral pinch strength compared with formal therapy (87). Evaluation of a multi‐modal hand rehabilitation program benefits (10 sessions of intervention such as soft tissue mobilization, scar massage, nerve gliding, and grip and pinch exercises, etc.), compared to a progressive patient‐directed home exercise training, showed no significant difference in the occurrence of CTS symptoms (e.g. pain, numbness, and paresthesia) (88).
3.9. Physiotherapy and Exercise Therapy
No significant difference was reported in the occurrence of CTS symptoms, functional ability, and grip or pinch strength between the multi‐modal hand treatment (physiotherapy) group and the home exercise group (76, 87).
Ultrasound and laser therapy improve some symptoms of CTS, including pain, numbness, and paresthesia. However, ultrasound and laser procedures are favored over the exercise groups; and ultrasound and laser groups are equally effective. Investigators reported improvement in pinch strength with ultrasound, laser, and exercise therapy. (89).
Nerve and tendon gliding exercises alone or plus laser or ultrasound therapy were evaluated. There was a significant improvement after treatment in all groups, and combined groups showed significant improvement compared to the exercise therapy group (89). According to the GRADE approach, the overall quality of evidence in this field was moderated (76, 90).
4. Open Carpal Tunnel Release Post-Operative Management and Rehabilitation Protocol
Several post-operative protocols have been used in CTS patients, some based on surgeons’ experience and others developed by specialized hospitals. The authors summarized the evidence and recommended a step by step post-op education and rehabilitation protocol in Table 1. However, post-operative rehabilitation is not supported by national medical insurance in some countries such as France. Therefore, surgeons could educate their patients for post-operative exercises and other care by prepared pamphlets under the guidance of Table 1.
| Post-Operative Time | General Recommendations | Patient Educations | Home Exercises | Goals |
|---|---|---|---|---|
| 3rd-5th day (1st visit) | Remove post-op dressing after 5 days, wound check (91); Usage of the sterile and dry dressing over incision at all times till suture removal; Assess finger mobility (91, 92). | Explain the patient to take care of the suture site, and edema control; Patient’s education about ROM of the fingers without wrist flexion and extension; Wear the splint at all times except for exercises until the 2nd visit; Avoid bending the operated wrist forward until 2 weeks post operation, the splint will help with this; Do not perform heavy lifting, gripping or grasping at this time (91, 93, 94). | Gentle thumb flexion, extension, and opposition, AROM exercises, as well as elbow and shoulder AROM exercises, 10 reps, 3 - 5 times/day (91, 94-96). | Pain reduction; Control of edema (91, 92, 94). |
| 10-12th day (2nd visit) | A surgical follow-up; Sutures can be removed from 10 days up to 3 weeks after surgery (according to the hand surgeon) (91, 96); Change sterile dressing (91). | Learn patients to keeping hand clean and dry until 2 weeks post-op (91, 93); Continue to use a splint and re-educate about no heavy lifting (91); Symptoms oftentimes resolve quickly after surgery, exception for the numbness that may take time to resolve (94). | Similar to the previous stage. | Pain reduction; Control of edema (91, 92, 94). |
| 5th day-3rd week | Therapy Visit; Usage the modalities such as ultrasound; Ensure proper wound healing and scar mobility (94); Start desensitization as needed (wound softening, massage and desensitization, at least 5 - 10 minutes, 5 times/day); Start control of edema, elevation, massage, whirlpool, hand fisting with the overhead position, 10 times/hour to prevent swelling; Wear a splint at night for a total of 6 weeks following surgery (91, 92, 97). | Similar to the previous stage. | Start the gentle active wrist flexion and extension (10 reps, 3 - 5 times/day); Continue of thumb flexion, extension and opposition AROM exercises, in addition to shoulder and elbow AROM exercises (10 reps, 3 - 5 times/day); Do tendon-gliding exercises (complete series of fists 10 repetitions, 5 times/day) (91, 93, 94, 96). | Achievement of full PROM and AROM in the fingers and wrist; Pain reduction; Control of edema (91, 93). |
| 3rd-5th week | If there is prolonged paresthesia or hypersensitivity, add a program for desensitization such as different textures, pulsed US, topical ointments; If excessive edema persists, may try an isotone glove, or Coban wrapping for compression (93). | Massage the scar with cream for 5 minutes 5 times/day; Decrease the scar sensitivity and flatten it by use of moderately deep pressure; For scar flattening/softening wearing the silicone scar pad once the scar has closed, usage Us, mild cross-friction massage and scar pump as needed (93); Wash the wound each morning with soap and water, and dry it (93); Wear the splint at night, as needed for support, till 6 weeks post-operation; Try a gradual return to activities without pain (Begin gentle activities of daily living) (91). | Nerve Gliding Exercises (5 Rep/5 times/day –with holding each position 10 seconds) (91); Gentle composite hand/wrist extension (light exercises against resistance) (93). | Gradually return to activities (91, 93) |
| 5-6th week | The patients with poor outcomes where symptoms persist (or other problems such as persistent hypersensitivity or Complex Regional Pain Syndrome) may require longer rehabilitation program, with a gentle progression (consult a surgeon if necessary) (93, 94). | Do not start squeezing hand-immobile objects (e.g. tennis ball) (93). | Start on a gradual hand grip-strengthening program (repeated 5 times/day), with Thera-putty, power web, etc. Progress strength exercises as the patient tolerate; Add wrist curl with graded weight in multi-direction (flexion, extension, supination, pronation, radial, and ulnar deviation); Use biceps curl and shoulder strengthening trainings if have a weakness (94-97). | -Return to full AROM-PROM; Restore grip strengthening (93). |
| 6-8th week | Similar to the above. | The patients can do lighter tasks (house cleaning and work tasks permitted) (93). | Progress strengthening exercises as tolerated (93); Wrist curls with graded weight for flexion, extension, supination, pronation, and ulnar and radial deviation (93); Use biceps curls and shoulder strengthening exercises if they are weak (93). | Restoration of wrist power (93). |
| 8-12th weeks | Return to work after 8 weeks for sedentary jobs, 10 - 12 weeks for heavier jobs (93). | |||
5. Conclusion
Physicians can prescribe multiple treatment options to CTS patients. Only corticosteroids in oral or injectable form have strong therapeutic effects in pain control, functional improvement in the short term, and some methods have moderate evidence such as shockwave therapy, and nocturnal wrist splints. Post carpal tunnel release rehabilitation can be started a few days after the operation.