1. Background
Over the past twenty years, the global population has experienced a significant increase in the rate of overweightness and obesity, resulting in a worldwide obesity epidemic (1). This epidemic has resulted from the consistent overconsumption of high-calorie diets and high rates of physical inactivity (2). Due to these decreases in physical activity and increases in food/calorie consumption, a concomitant increased prevalence of overweight/obesity in children has been found with the prevalence of overweightness/obesity doubling between 1976 and increasing by a further 13% in 1994 and an additional 15.5% in the year 2000 (3). There are various risks associated with overweightness/obesity in children, including risks such as neurological, orthopaedic, pulmonary, and endocrine conditions. Children's self-esteem, body image, and economic mobility are also negatively affected as they age. Additional complications involve the development of non-communicable diseases (NCDs) and the persistence of childhood overweightness/obesity into adulthood (4). Thus, childhood overweightness/obesity is likely to challenge worldwide public health if the current problems are not addressed (4, 5).
Physical activity/exercise is essential in the childhood and adolescent years, this is due to drastic psychological and physical modifications occurring at this point in time. Furthermore, behaviours of lifestyle are formed, that could affect behaviours in an individual’s adult life and later health (6). Unless children become more physically active, it is likely that the overweightness/obesity rate, as well as its associated health risks will continue to rise (7), which is why early intervention for overweightness/obesity is crucial. While a low level of physical activity is a major case of overweightness/obesity (8), evidence exists indicating that participation in various forms of physical activity could positively affect health (9, 10).
Reversing this troubling trend may mean addressing the energy surplus in the home where children are likely to feel the most comfortable (11, 12). For this reason, it is believed that interventions should target the overweight and obese children in their home environment, where they can partake in a training program without the need for an array of expensive and bulky equipment (13, 14). This maintenance and restoration of health and independence in the overweight/obese population in a cost-effective manner and is especially important in developing countries, such as South Africa, where there is limited transport or funds for transport (14). Further, there may be an increased need for home-based training since, when compared to a gymnasium, home-based training adds an element of privacy, which is a major concern for most overweight and obese individuals (14). In this regard, callisthenic training is a form of dynamic exercise consisting of a variety of simple, often rhythmical, movements generally using minimal equipment or apparatus. These exercises are intended to increase muscular strength and flexibility with movement such as bending, jumping, swinging, twisting, or kicking using only the individual’s body weight for resistance (14).
2. Objectives
This study attempted to determine and compare the efficacy of home-based callisthenic resistance training on CVD risk in overweight compared to normal-weight children.
3. Methods
3.1. Participants
A sample of 15 previously sedentary overweight/obese children (OOC) (boys ≥ 22% body fat (%BF); girls ≥ 27% BF) and 15 previously sedentary normal-weight children (NWC), aged 9 - 11 years were assigned to a six-week home-based callisthenic resistance training program, while an additional 15 previously sedentary normal-weight children were assigned to a non-exercising control group (NON). For six months before the study, the participants were required to be weight stable and not participate in any structured exercise, not be on any dietary interventions of supplementation, and have no absolute and/or relative contraindications to testing/training (15). Prior to participation in the study, all participants and their parents/guardians gave assent and written informed consent, respectively. Ethical clearance to conduct the study was obtained from the relevant Institutional Review Board (REC-01-194-2015).
3.2. Procedures
Kinanthropometric evaluations took place in line with ISAK standards (16). All participants’ body mass (BM) was evaluated using a Trojan scale (BSA16056v, Duteck Industrial co. ltd, Taiwan) and stature was evaluated with a Seca stadiometer (216, Seca, United States of America). To calculate body mass index (BMI), each participant’s BM was divided by stature squared. Waist circumference was divided by hip circumference to calculate the waist-to-hip ratio (WHR), while waist circumference was divided by stature to determine waist-to-stature ratio (WSR). Triceps and subscapular skinfolds were used to determine the sum of skinfolds (SKF) using a caliper (Harpenden, HSB-BI, ATICO Medical Pvt. Ltd, UK). The two skinfold measurement sites were used to determine body fat percentage (BF%) using the Durnin and Rahaman equation (17): %BF = 1.21(triceps + subscapular skinfolds) – 0.008 (triceps + subscapular skinfolds)² - 3 - 2. Body mass was multiplied by percentage body fat and divided by 100 to determine fat mass (FM), and lean body mass (LBM) was determined by subtracting the FM from the BM.
Each participant’s resting heart rate (RHR) and resting diastolic (RDBP), and systolic blood pressure (RSBP) were measured in the seated position after a five-minute rest using established auscultatory methods (18). In addition to each participant’s RBP and RHR, these parameters were used to calculate rate-pressure product (RPP) and resting mean arterial pressure (RMAP). Rate-pressure product (RPP) was computed by multiplying RHR and RSBP, while resting mean arterial pressure (RMAP) was calculated using the following equation (19):
The participants were also expected to participate in a 1.6 km walk/run test on a level field. Upon completion of this distance, the participants’ time was recorded and used in the final analysis (15).
3.3. Intervention
Participants in the OOC and NWC groups were required to participate in a six-week, three times weekly, home-based callisthenic resistance training program (20, 21), for approximately 45 minutes. The children in the CON group were instructed to maintain their usual daily activities and not engage in any structured physical activity. Participants in the training groups were required to complete a 5min warm-up consisting of light jogging on the spot followed by six callisthenic exercises (Table 1), after which they were required to complete 10min of stretching as a cool-down (3).
| Exercise | Repetitions | Sets |
|---|---|---|
| Weeks 1-3 | ||
| Sit-ups | 6 | 1 |
| Jumping jacks | 10 | 1 |
| Toe touches | 10 | 1 |
| Knee push-ups | 6 | 1 |
| Double leg forward jump | 10 | 1 |
| Double leg backward jump | 10 | 1 |
| Weeks 4-6 | ||
| Walking on hips | 10 | 2 |
| Knee-chest lifts | 10 | 2 |
| Bicycle in the air | 10 | 2 |
| Leg raises | 10 | 2 |
| Jump & turn 90° | 10 | 2 |
| Ankle jumps | 10 | 2 |
3.4. Statistical Analysis
Data analysis was done using SPSS-25 (IBM Corporation, Armonk, New York). Data analysis involved the determination of means and standard deviations and t-tests to determine if any significant changes occurred pre- versus post-test within each group and to compare any changes across the various groups. A P ≤ 0.05 was considered statistically significant.
4. Results
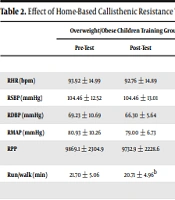
Results indicated that the home-based callisthenic resistance training program significantly (P ≤ 0.05) decreased BM (from 44.54 ± 10.53 to 43.77 ± 10.38 kg, P = 0.002), BMI (23.27 ± 5.05 to 22.85 ± 5.00kg.m-2; P = 0.002), BF% (from 33.01 ± 5.15 to 31.94 ± 5.55%, P = 0.042), FM (from 15.01 ± 5.45 to 14.30 ± 5.33kg, P = 0.001), sum of skinfolds (from 46.46 ± 11.65 to 44.38 ± 11.61 mm, P = 0.032), and run/walk time (from 21.70 ± 5.06 to 20.71 ± 4.96 min; P = 0.003) in the OOC (Table 2). The training regime also decreased HC (from 73.26 ± 5.84 to 72.76 ± 5.88 cm, P = 0.031), and sum of skinfolds (from 29.38 ± 10.18 to 25.84 ± 8.11mm, P = 0.035) in the NWC.
| Overweight/Obese Children Training Group (OOC), n = 15 | Normal Weight Children Training Group (NWC), n = 15 | Non-Exercising Control Group (CON), n = 15 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | Sig. | Pre-Test | Post-Test | Sig. | Pre-Test | Post-Test | Sig. | |
| Cardiovascular Measures | |||||||||
| RHR (bpm) | 93.92 ± 14.99 | 92.76 ± 14.89 | 0.414 | 88.76 ± 15.5 | 88.53 ± 11.85 | 0.917 | 93.92 ± 14.99 | 92.77 ± 14.89 | 0.916 |
| RSBP (mmHg) | 104.46 ± 12.52 | 104.46 ± 13.01 | 1.000 | 103.23 ± 14.82 | 102.76 ± 11.09 | 0.866 | 104.46 ± 12.52 | 104.46 ± 13.02 | 0.479 |
| RDBP (mmHg) | 69.23 ± 10.69 | 66.30 ± 5.64 | 0.207 | 72.61 ± 9.81 | 69.69 ± 11.57b | 0.049 | 69.23 ± 10.69 | 66.31 ± 5.65 | 0.689 |
| RMAP (mmHg) | 80.93 ± 10.26 | 79.00 ± 6.73 | 0.426 | 82.79 ± 9.77 | 80.68 ± 10.04 | 0.155 | 80.94 ± 10.26 | 79 ± 6.73 | 0.856 |
| RPP | 9869.1 ± 2304.9 | 9732.9 ± 2228.6 | 0.702 | 9124 ± 1999.22 | 9064.92 ± 1372.07 | 0.843 | 9869.08 ± 2304.88 | 9732.92 ± 2228.59 | 0.509 |
| Run/walk (min) | 21.70 ± 5.06 | 20.71 ± 4.96b | 0.003 | 18.6 ± 3.8 | 18.34 ± 4.03b | 0.019 | 21.71 ± 5.07 | 20.71 ± 4.97 | 0.646 |
| Anthropometric Measures | |||||||||
| Body mass (kg) | 44.54 ± 10.53 | 43.77 ± 10.38b | 0.002 | 34.43 ± 6.66 | 34.25 ± 6.85 | 0.569 | 44.55 ± 10.54 | 43.78 ± 10.38 | 0.179 |
| BMI (kg.m-2) | 23.27 ± 5.05 | 22.85 ± 5.00b | 0.003 | 17.87 ± 2.78 | 18.02 ± 2.70 | 0.814 | 23.28 ± 5.05 | 22.86 ± 5.00 | 0.113 |
| WC (cm) | 72.26 ± 7.09 | 71.26 ± 7.60 | 0.174 | 64.46 ± 5.32 | 64.07 ± 5.70 | 0.217 | 72.27 ± 7.09 | 71.27 ± 7.61 | 0.819 |
| HC (cm) | 83.26 ± 8.36 | 83.00 ± 8.36 | 0.237 | 73.26 ± 5.84 | 72.76 ± 5.88b | 0.031 | 83.27 ± 8.36 | 83.00 ± 8.37 | 0.082 |
| WHR | 0.86 ± 0.04 | 0.85 ± 0.04 | 0.393 | 0.87 ± 0.06 | 0.87 ± 0.06 | 0.753 | 0.86 ± 0.04 | 0.86 ± 0.05 | 0.303 |
| WSR | 0.51 ± 0.05 | 0.51 ± 0.05 | 0.279 | 0.45 ± 0.03 | 0.45 ± 0.03 | 0.303 | 0.52 ±0.05 | 0.51 ± 0.06 | 0.709 |
| LBM (kg) | 29.58 ± 5.91 | 29.47 ± 5.81 | 0.643 | 27.14 ± 5.39 | 27.20 ± 5.26 | 0.923 | 29.59 ±5.91 | 29.48 ± 5.81 | 0.466 |
| BF% | 33.01 ± 5.45 | 31.94 ± 5.55b | 0.042 | 21.14 ± 3.44 | 20.21 ± 5.57 | 0.510 | 33.02 ± 5.15 | 31.94 ± 5.56 | 0.905 |
| FM (kg) | 15.01 ± 5.45 | 14.30 ± 5.33b | 0.001 | 7.28 ± 1.88 | 7.04 ± 2.84 | 0.637 | 15.02 ± 5.45 | 14.30 ± 5.34 | 0.928 |
| ∑SKF (mm) | 46.46 ± 11.65 | 44.38 ± 11.61b | 0.032 | 29.38 ± 10.18 | 25.84 ± 8.11b | 0.035 | 22.07 ± 6.15 | 21.30 ± 5.87b | 0.035 |
Effect of Home-Based Callisthenic Resistance Training on Cardiovascular Disease Risk in Overweight Compared to Normal Weight Children a
5. Discussion
The primary objective of the present study was to evaluate and contrast the effectiveness of callisthenic resistance training performed at home on CVD risk in overweight compared to normal-weight children. This study resulted in improvements in hip circumference, sum of skinfolds in the normal-weight children. In turn, improvements were found in body mass, BMI, BF%, FM, sum of skinfolds, and cardiorespiratory endurance in the sampled overweight/obese children.
While the present study found that six weeks of home-based callisthenic resistance training was not effective at improving BP measures and its indices in the overweight/obese group (OOC), RDBP was found to be decreased in the normal weight group. The study of Naylor et al. (22) is the only study to have shown a significant decrease in SBP after a resistance training intervention. This is because BP is not studied in children in resistance training studies (23). The lack of change in BP measures and its indices could be attributed to these measurements and indices already being within normal ranges. In turn, only the overweight/obese children were shown to have improvements in cardiorespiratory endurance despite a lack of an aerobic exercise component in the program. Although the evidence demonstrating that resistance training can improve cardiorespiratory endurance in adults is unequivocal (9), there is limited evidence for such effects in children (24), especially those that are overweight/obese. However, available data suggest that resistance training programs may lead to beneficial improvements in cardiorespiratory endurance in children (24, 25). In the present study, the increase in cardiorespiratory fitness may be linked to the previously sedentary and/or overweight/obese nature of the children (3).
The present study demonstrated that six weeks of callisthenic resistance training can improve BM, BMI, %BF, FM, and sum of skinfolds in children who are overweight and obese. Interestingly, the callisthenic resistance training also decreased HC and sum of skinfolds in the normal-weight children. It remains to be confirmed whether future callisthenic resistance training studies will support the findings of the present study. Support is in some measure forthcoming from conventional resistance training studies. In this regard, conventional resistance training has been shown to decrease BF% and increase LBM in overweight/obese children (26). Participation in conventional resistance training has also shown to produce significant decreases in BF% and increased muscle and bone mass in normal-weight boys aged 13 - 17 years (27). These findings are especially important in that it is thought that resistance training can only improve body composition in obese children when combined with dietary control (28). Unfortunately, neither WHR nor WC has been measured in any resistance training studies utilizing children (23).
5.1. Limitations
The findings of this study should not be universally directed to all sedentary and/or overweight/obese children due to the small sample. In addition, the study utilized male and female participants and improvements may prove different in a single gender population due to gender differences in exercise responses and gender-specific adaptations to exercise (9). It is further uncertain if an extended intervention duration would provide further advancements in measures, such as RHR, RBP, RPP, RMAP, and/or BMI.
5.2. Conclusions
The increasing incidence of childhood overweightness/obesity and concomitant CVD risk has become a worldwide public health challenge. Thankfully, it seems that home-based callisthenic resistance training can have positive impacts on overall body composition and may prove to be a cost-effective and essential tool in the fight against childhood overweightness/obesity, whether in normal weight or even overweight/obese children. The findings of the efficacy of callisthenic resistance exercise in reducing body mass, BMI, percentage body fat, fat mass, and sum of skinfolds in overweight and obese children is somewhat of a hallmark since previous research has failed to demonstrate these improvements in children (3, 29). This finding is also noteworthy since young overweight/obese children may not necessarily find exercise as enjoyable when in a group setting, where they may be subjected to harsh criticism for their poor health status, compared to the comfort of their own home where they have more privacy (14).