1. Background
The meniscofemoral ligaments (MFLs) consist of collagen fibers adhering to the medial femoral condyle from the posterior horn of the lateral meniscus and include the anterior meniscofemoral ligament (aMFL), called the Humphrey ligament, which is anterior to the posterior cruciate ligament (PCL), and the posterior meniscofemoral ligament (pMFL), called the Wrisberg ligament, which is posterior to the PCL. The MFLs primarily allow movement of the lateral meniscus in harmony with the lateral femoral condyle (1). Biomechanical studies have shown that the MFLs restrain posterior translation as the PCL and anterior translation as the anterior cruciate ligament (ACL) (2, 3).
The MFLs affect the contact pressure of the lateral compartment (4, 5). Forkel et al. observed that patients with rupture of the MFL (even if the lateral root remains intact) had a significant increase in the lateral compartment contact pressure, but there was no significant change in the lateral compartment contact pressure in the lateral meniscus root rupture group when the MFL was intact (5). In a clinical study investigating patients with ACL rupture, MFL damage was observed in an arthroscopic evaluation (6).
Several studies have shown that at least one MFL was present in 94.4% of a normal population by magnetic resonance imaging (MRI). Other studies have shown that the pMFL was present in nearly every case and the aMFL in 88.2% of the subjects on MRI (7-10). The relationship between lateral meniscus tear and presence of MFL has been studied, but there is little information about the relationship between ACL rupture and the presence of MFLs (6, 11, 12).
2. Objectives
The study aims were to compare the presence of MFLs by MRI between patients with intact ACLs and patients with ruptured ACLs and determine if there is a relationship between time from injury to MRI examination in ruptured ACL subjects.
3. Methods
We retrospectively evaluated MRI images of the knees of patients aged between 15 and 50 with adequate quality images and medical history available on the picture archiving communication system from 2014 to September 2018. This retrospective MRI study was approved by Ankara Numune Education Research Hospital Ethics Committee Decision no: E-2018-2220.
3.1. Patient Selection
The patient’s age, sex, occupation (past and current jobs), sport activity level (classified as sedentary, recreational, and professional), sides, and time from injury to MRI (± days) were recorded.
The inclusion criteria were: Patients with arthroscopically confirmed total ACL rupture with non-contact mechanism, adequate quality images available on our picture archiving and communication system, and who had undergone primary ACL reconstruction were included in the study. According to this evaluation, we found 202 patients with total ACL. Non-contact ACL ruptures are defined as ACL ruptures that occur without physical contact between patients, and contact ACL ruptures are defined as ACL ruptures that occur with physical contact between patients.
The exclusion criteria were: (1) patients with partial ACL rupture; (2) ACL ruptures with contact mechanism;(3) combined PCL injury;(4) posterolateral corner (PLC) injury or MCL injury; (5) previous knee surgery; (6) moderately advanced primary and secondary knee arthritis (Kellgren–Lawrence grades 3–4); (7) knee tumor; (8) osteochondral defects, associated medial/lateral meniscal lesions other than ramp lesions; (8) varus valgus knee deformity (>15°); (9) general joint laxity (Beighton Scoring > 0) (13), skeletal immaturity, history of major trauma to the knee joint before ACL rupture, infection of the knee; (10) body mass index > 25 ; (11) lack of available MRI, (12) professional athletes or those with recreational sporting activities related to the knee; (13) heavy labor (occupations were subjectively classified as light, intermediate, and heavy); (14) Q-angle > 200.
After exclusion criteria were applied, 100 patients were selected for the study in the ACL ruptured group. We recruited 100 patients with suspected ACL tear (from a similar mechanism of injury) and whose MRI revealed an intact ACL. The patients for inclusion in the matched control group were selected by applying the same exclusion criteria as described above. A demographic form was developed for all patients.
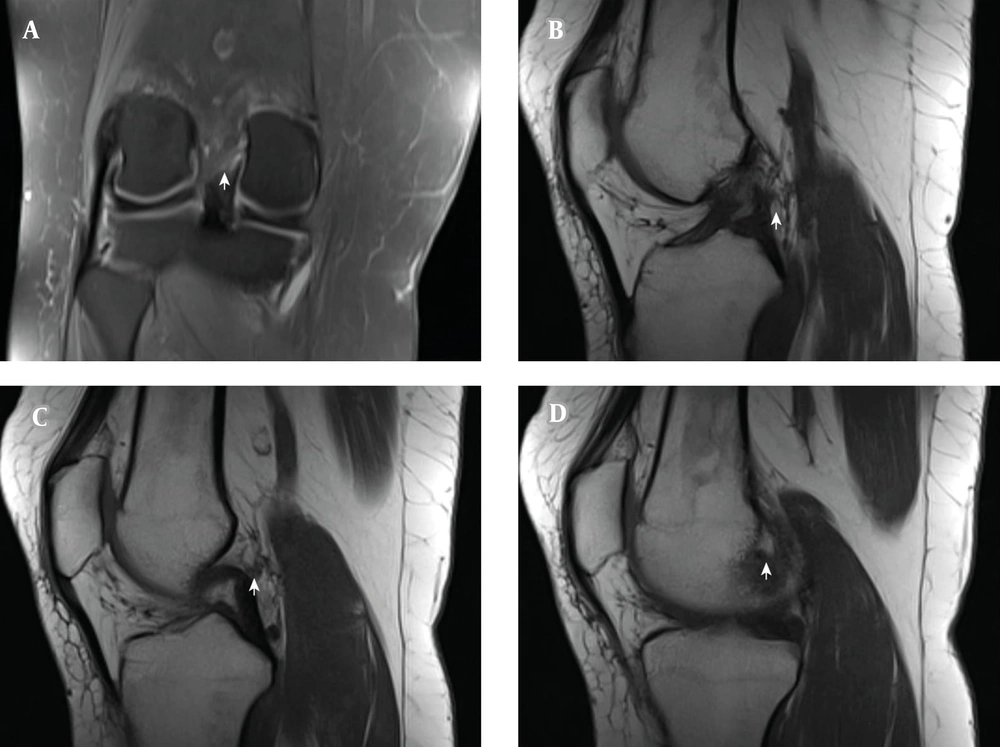
The aMFL (Humphrey) or pMFL (Wrisberg) was characterized as a separate, ovoid, hypointense focus or discrete hypointense bulge or lump, > 3 mm thick and posterior or anterior to the PCL, respectively, on sagittal images; and as a ≥ 3-mm thick hypointense band coursing obliquely from the posterior lateral meniscus to the medial femoral condyle on coronal images (12, 14, 15). Additionally, the presence of aMFL and pMFL was evaluated by examining all available planes. If any MFL was seen in at least one plane, it was recorded as present (Figure 1).
ACL ruptured group, and the control group were then divided into 4 subgroups; patients without any MFL were defined as group 1, patients with only aMFL defined as group 2, patients with only pMFL defined as group 3 and patients with both aMFL and pMFL defined as group 4.
The preoperative MRI scans were reviewed by a radiologist with special expertise in musculoskeletal imaging and an associate professor who had >10 years of orthopedic experience who were blinded to this study. Differences regarding the presence of an MFL were resolved by discussion between the observers to reach consensus.
The knee MRIs of all patients were acquired in our hospital by using an Optima MR450w 1.5-T (tesla) scanner with a phased-array knee coil (General Electric, IL, USA). MRI was performed with the patient in the supine position and knees at 100° to 150° of external rotation. For the MRI protocol, a 4-mm thin coronal section was taken, and sagittal turbo-spin echo proton density-weighted image (WI), T2-WI, and coronal STIR sequences were used. Careful attention was paid to the coronal and sagittal proton density-WI and T2-WI sequences for aMFL and pMFL differentiation (Figure 2).
Coronal image and three consecutive sagittal images lateral to medial. White arrow pointing the posterior meniscofemoral ligament (pMFL). A, the pMFL can be seen coronal image on T2 MRI; B - C, the pMFL can be seen just posterior to the posterior cruciate ligament on T1 MRI d)The pMFL can be seen femoral adhesion side on T1 MRI.
3.2. Statistical Analysis
The NCSS 2007 program (Number Cruncher Statistical System, Kaysville, UT, USA) was used for the statistical analysis. Descriptive statistical methods (mean, standard deviation, median, frequency, percentage, minimum, and maximum) were used to evaluate the study data. The Shapiro–Wilk test and graphical examinations were used to test the normal distribution of quantitative data. Student's t-test was used to compare variables with normal distribution between the two groups. The Mann–Whitney U-test was used to compare quantitative variables with non-normal distributions between the two groups. The Kruskal–Wallis test and Bonferroni–Dunn test were used to compare groups in cases in which three or more variables showed a non-normal distribution. The interobserver and intra-observer reproducibilities were determined by Cohen's Kappa. They were categorized: 0, none; ≤ 0.40 poor; 0.41 to 0.60 moderate agreement; 0.61 to 0.80 good agreement; > 0.81 excellent agreement (16). A point-biserial correlation is used to measure the strength and direction of the association that exists between age and the presence of aMFL or pMFL. A P value < 0.05 was considered statistically significant.
4. Results
There is no significant difference between the groups in terms of age (P = 0.06). There is a significant difference between the groups in terms of side of the injury and gender (P = 0.007, P = 0.001; respectively) (Table 1).
| Variables | Anterior Cruciate Ligament Rupture Group (n = 100) | The Control Group (n = 100) | P |
|---|---|---|---|
| Age (y) | 0.06 a | ||
| Min-max (median) | 15 - 47 (28) | 17 - 50 (29) | |
| Mean ± SD | 27.96 ± 7.46 | 29.96 ± 7.51 | |
| Gender; No. (%) | 0.001 b, c | ||
| Male | 82 (82.0) | 50 (50.0) | |
| Female | 18 (18.0) | 50 (50.0) | |
| Side; No. (%) | 0.007 b, c | ||
| Left | 33 (33.0) | 52 (52.0) | |
| Right | 67 (67.0) | 48 (48.0) | |
| Meniscofemoral ligament; No. (%) | 0.001 b, c | ||
| None (group 1) | 37 (37.0) | 14 (14.0) | |
| Humphrey (group 2) (aMFL) | 14 (14.0) | 13 (13.0) | |
| Wrisberg (group 3) (pMFL) | 40 (40.0) | 43 (43.0) | |
| Humphrey + Wrisberg (group 4) (aMFL,pMFL) | 9 (9.0) | 30 (30.0) |
a Student t-test.
b Pearson chi-square test.
c P < 0.01.
In the ACL ruptured group, a significantly lower presence of Wrisberg or Humphrey ligament was observed than the control group (P = 0.001) (Table 1).
According to the point-biserial correlation, a negative and significant relationship was found between age and the presence aMFL variables in the ACL ruptured group (rpb: 0.342; P < 0.001). A negative and significant relationship was found between age, and the presence of pMFL in the ACL ruptured group (rpb: 0.431; P < 0.001). A negative and significant relationship was found between age and the presence of aMFL in the ACL intact group (rpb: 0.442; P < 0.001). A negative and significant relationship was found between age and the presence of pMFL in the ACL intact group (rpb: 0.631; P < 0.001).
The time from injury to MRI showed a significant difference among ACL ruptured subgroups (P = 0.001; P < 0.01). Pair comparisons were made to determine the subgroup that showed difference; the time from injury to MRI was higher in group 1 than group 2, group 3 and group 4 (P = 0.017, P = 0.001, P = 0.001, P = 0.004; respectively). No statistical difference was observed between the other groups (P > 0.05, all) (Table 2).
| Group with an Anterior Cruciate Ligament Rupture | Trauma Time (Day) | P | ||
|---|---|---|---|---|
| n | Min-Max (Median) | Mean ± SD | ||
| Meniscofemoral ligament | 0.001 a, b | |||
| None (group 1) | 37 | 1 - 1200 (200) | 281.73 ± 293.62 | |
| Humphrey (group 2) (aMFL) | 14 | 2 - 1400 (10) | 213.57 ± 407.26 | |
| Wrisberg (group 3) (pMFL) | 40 | 1 - 3000 (20) | 182.22 ± 532.85 | |
| Humphrey + Wrisberg (group 4) (aMFL,pMFL) | 9 | 3 - 365 (9) | 50.89 ± 118.30 | |
a Kruskal Wallis Test.
b P < 0.01.
A radiologist and an orthopedic surgeon who were blinded to the study separately evaluated the MFLs. The interobserver and intra-observer kappa values were 0.71 and 0.83 for the MFLs, respectively.
5. Discussion
There were two principal findings of this study. First, the presence of MFLs on MRI was significantly lower in the ACL rupture group than in the control group. Second, the presence of MFLs decreased with increasing time from injury.
In this study, we evaluated the absence or presence of the MFLs in ACL ruptured and ACL intact patient knees. Compared with the control group, the ruptured ACL group had a significantly lower prevalence of MFLs. This ACL absence could be due to a congenital absence or a rupture. Two hypotheses can be proposed: MFLs rupture during ACL tearing or congenital pMFL-deficient knees have a higher risk of ACL rupture. Further studies are needed to evaluate these hypotheses.
The presence of the pMFL reportedly ranges between 66.4 and 100% in the literature (7, 12, 17, 18). In our study, the presence of the pMFL was 78 and 49% in the intact and ruptured ACL groups, respectively. However, the presence of the aMFL has been lower (between 0 and 88.2%) than that of the pMFL in almost all previous studies (9, 12, 17-19). In our study, the presence of an isolated aMFL was 44 and 23% in the intact and ruptured ACL groups, respectively.
Anatomical studies have shown several variations in the proximal and distal adhesion sites of the MFLs (17, 20). The aMFL may be thick or thin in two or three bands adjacent to the articular cartilage in the inferoanterior portion of the PCL, starting from the posterior part of the posterior meniscus and in the direction of the femur to the left. The pMFL is generally expressed from the posterior horn of the anterior horn and may be thick or thin in the posterosuperior part of the PCL or in the two bands within the posteromedial PCL band (21). Bozkurt et al. observed that the MFL thickness ranged from 2.6 to 6.1 mm (average: 2.6 mm) (22). In our study, the thickness and adhesion site variations in the MFL bonds were not evaluated. We accepted MFLs ≥ 3 mm as being present.
In the literature, the relationship between age and the presence of MFL is controversial. Rohrich et al. showed that there is no relationship between age and the presence of MFL (23). On the other hand, there are studies showing a relationship between age and the presence of MFL (17, 20). In our study, we found a negative correlation between age and the presence of MFL in both groups.
Forkel et al. found that MFL damage was observed in five of the 32 patients with lateral meniscus root ruptures who underwent arthroscopic evaluation for ruptured ACL (6). Similarly, there was a relationship between posterior meniscus root tear and MFL absence in patients with ACL tear. Previously, when the meniscus was extruded, absence of the MFLs was more prevalent in patients with lateral meniscus root tear (24-26). In our study, we thought that instability causing degeneration of the MFLs would involve both weakening of the MFL structure and possible eventual MFL disappearance. The MFLs were less prevalent in the ACL ruptured group, which was consistent with other studies.
Several studies have shown a relationship between the lateral meniscus and MFLs, especially the discoid meniscus (27, 28). Atypical thickness and atypical region pMFLs have been shown to cause discoid lateral meniscus rupture (29, 30). However, findings in the literature have been inconsistent. A retrospective arthroscopic study by Lee et al. found no relationship between meniscus tear and the MFLs (12). Similarly, Miller et al. found no significant relationship between meniscus tear and the MFLs by MRI (11). Patients with meniscus rupture and meniscus root tears were not included in the present study because meniscus and ACL tears may have affected the results, and there were not enough patients to evaluate different meniscus tear types and ACL ruptures (24-26).
At present, there are no standardized guidelines for evaluation of MFLs by MRI. Proper evaluation of the MFLs on MRI should be performed for each plane and always include the sagittal plane (23). Previous studies on the presence of the aMFL and pMFL in the coronal plane have shown that Cohen’s kappa coefficient was 0.62 for the aMFL and 0.72 for the pMFL. When evaluated in all available planes, Cohen’s kappa coefficient was found to be 0.84 for the aMFL and 0.96 for the pMFL (23). In our study, MFLs were evaluated in each plane. We evaluated MFL by 1.5-T MRI because it has been shown to be sufficient in the literature (31).
There were some study limitations that should be considered. The use of MRI to evaluate the MFLs was a potential major issue because there is no established arthroscopic or surgical correlation with MRI findings. MRI may give false-negative results if it misses the fine MFL bonds and may give false-positive results because of the oblique PCL fibers (15, 32). We were careful to distinguish the oblique PCL and pMFL bundles. In our study, as anatomic markers, only BMI was evaluated. Such indicators as body fat, waist-hip ratio were not evaluated. Although we did not find any relation between the presence of MFL and BMI, other anatomic markers could be impacted by the presence of MFL. All patients were of a Caucasian population. MFLs vary according to race; different results may be obtained in different races (17, 20). Other limitations were the small numbers of patients with intact and ruptured ACLs and that most of the subjects were male. However, no sex-related difference in the prevalence of MFLs in the normal population has been reported (22, 33). Finally, we did not evaluate the cross-sectional areas, proximal/distal adhesion sides, and running angles in the MFLs in this study, which could have affected our results.
In conclusion, we observed the absence of MFLs (aMFL and pMFL) in a significant majority of patients with ruptured ACLs. Furthermore, we found a significant relationship between the time from injury to MRI and the absence of MFL in the ruptured ACL group. Future research is needed to evaluate correlations between arthroscopic or surgical findings and MRI features.