1. Background
The lateral meniscus is not anatomically symmetrical to the medial meniscus. It is rounder and has a wider body than the medial meniscus. The mobility of the lateral meniscus is also higher due to the presence of the popliteal hiatus at the attachment site (1, 2). The frequency of lateral meniscus tears is estimated to be 11.5 per 100,000 in the United States general population, most of which are complicated with an anterior cruciate ligament injury and injury of other intra- or extra-articular structures (3). In a study of 378 cases of isolated meniscus tears in stable knees conducted by Terzidis et al. (4), the rate of tear was 30.7% in the lateral meniscus and 69.3% in the medial meniscus, showing a relatively lower rate of the isolated lateral meniscus tear. Furthermore, most of the meniscus tears caused by sports activities occur in the posterior segment of the meniscus, many of them in the medial meniscus (5). The morphology of meniscus tears is affected by knee stability and the type of sport (6).
Rugby is a full-contact team sport played by two teams competing to bring an oval-shaped ball into the opponent's in-goal to score points. In Japan, rugby is generally played with 15 players on each side. Player positions are broadly divided into forwards and backs. Forwards compete for the ball in a scrum and require big body size and great strength, while backs advance the ball by passing, dodging, kicking, and other maneuvers and require running ability and agility.
Among patients diagnosed arthroscopically with lateral meniscus tears in the medial segment encountered in our center, we noticed that rugby players were clearly more prevalent than players of other sports. We hypothesized that a meniscus tear in the middle segment is a common injury in rugby players and is associated with a specific position in rugby.
2. Objectives
This study aimed to describe in detail a series of lateral meniscus tears while playing rugby.
3. Methods
We retrospectively reviewed the medical charts of our center between January 2006 and April 2020 for cases with an arthroscopically confirmed diagnosis of a meniscus tear. Inclusion criteria were cases with isolated lateral meniscus tears involving the middle segment, and the tears were either transverse or oblique. Exclusion criteria were abnormal morphological meniscus such as discoid meniscus, and other concurrent injuries such as ligament rupture, fracture, and serious cartilage injury. Among the cases identified, we focused on those in which injury was associated with rugby activities. We investigated the epidemiology of injury, including laterality of injury, player position, and phase of play; the symptoms; as well as imaging and arthroscopic findings.
This retrospective chart review was approved by the institutional review board of the National Hospital Organization, Kofu National Hospital (serial number: 27-8).
4. Results
Among 4452 cases (4666 knees) of arthroscopically proven meniscus tears diagnosed in our center, 249 cases (261 knees) had an isolated lateral meniscus tear with no morphological abnormalities, including discoid meniscus and no concurrent injuries such as ligament rupture, bone fracture, and severe cartilage lesion. Of these cases, only 44 cases (46 knees) (1.0% of all knees with meniscus tears) had tears in the middle segment (Cooper classification zone E) (7).
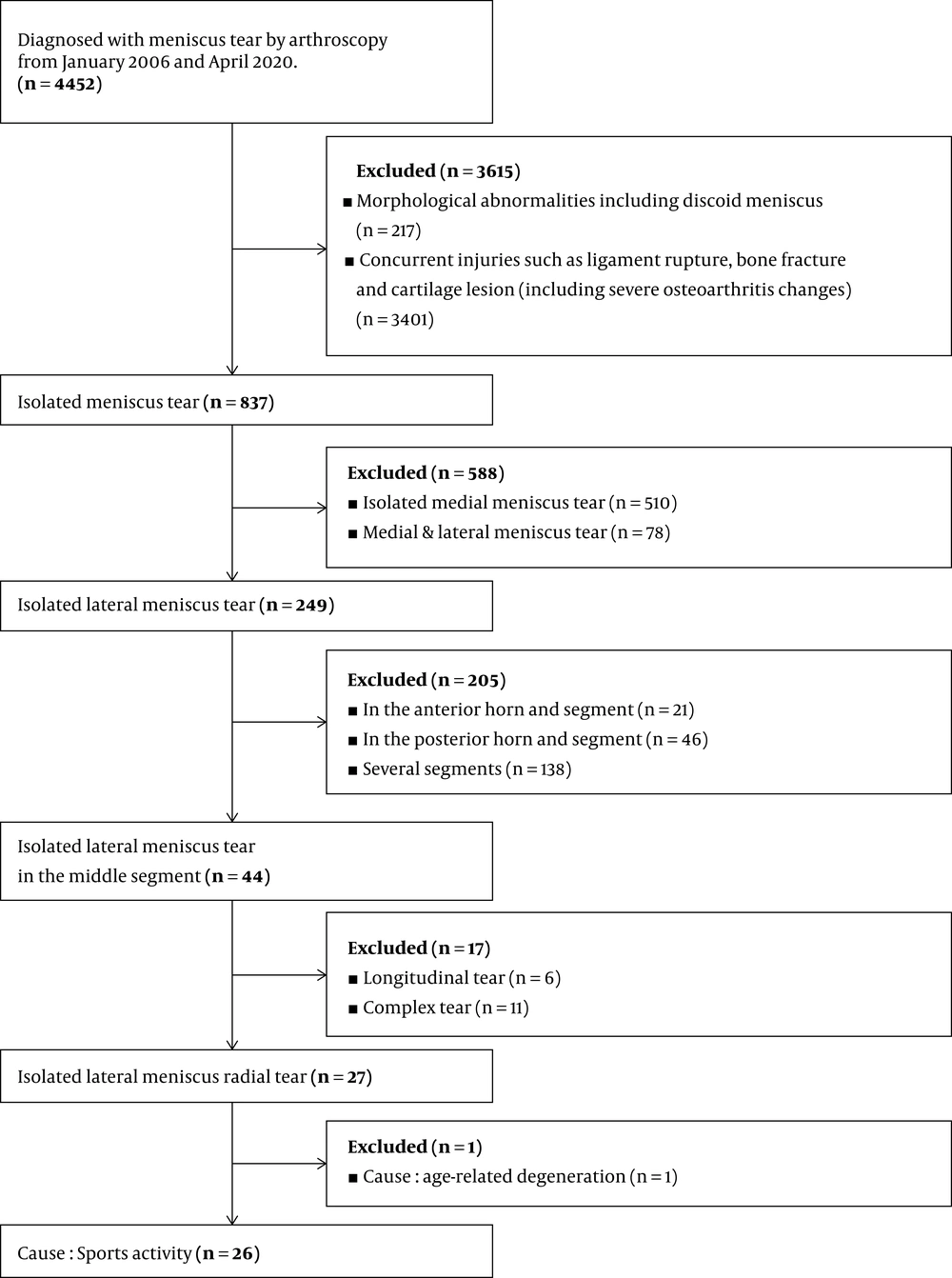
More than half of the tears in the middle segment were radial tears, found in 27 cases (28 knees) (61.4% of tears in the middle segment, 10.8 % of all isolated lateral meniscus tears). The causes of injury were sports activities in 26 cases and age-related degeneration in the remaining case (Figure 1). Rugby was the most common sport with 11 cases (39.2%), followed by soccer and baseball with 4 cases each, and then basketball with 2 cases (Table 1).
| Cause of Injury | Number of Cases | Sex (Male/Female) | Age (Mean) | BMI (Mean) | Diagnosed with Meniscus Tear by Arthroscopy |
|---|---|---|---|---|---|
| Sports | 26 | 21/5 | 15 - 59 (21.5) | 18.9 - 34.9 (25.7) | 1379 |
| Rugby | 11 | 11/0 | 17 - 24 (20.5) | 24.9 - 34.9 (29.6) | 65 |
| Soccer | 4 | 4/0 | 15 - 20 (18.3) | 18.9 - 24 (21.6) | 310 |
| Baseball | 4 | 2/2 | 16 - 59 (28.3) | 20.2 - 30.7 (24.9) | 88 |
| Basketball | 2 | 1/1 | 16 - 18 (17) | 19.2 - 24.8 (22) | 177 |
| Volleyball | 1 | 0/1 | 20 | 21.3 | 183 |
| Badminton | 1 | 0/1 | 18 | 21.2 | 43 |
| Wrestling | 1 | 1/0 | 22 | 23.7 | 9 |
| Weightlifting | 1 | 1/0 | 16 | 22 | 3 |
| Jiu-Jitsu | 1 | 1/0 | 38 | 25 | 2 |
4.1. Laterality of Injury, Rugby Experience, Position
There was no difference in the side of injury, with 5 patients injured on the right side, and 6 patients on the left side. The experience of playing rugby ranged from 4 to 14 years, with an average of 8.3 years. All were students belonging to 15-player rugby clubs at high school or university. Nine subjects were playing at the level of national matches, and two were playing at the level of prefectural qualifying matches. Regarding player position, there were 10 forwards and 1 back; with 5 patients in the front row (hooker, prop), 2 patients in the second row (lock), 3 patients in the third row (flanker, No. 8), and 1 patient was a three-quarter back (center, wing).
4.2. Phase of Play
When injuries were examined by phase of play, “unknown” was most common (6 patients), followed by tackle (2 patients when tackling and 2 patients when being tackled), and running (1 patient when taking off to run).
When further categorized by player position, the phase of play in front row players was unknown in 4 cases and tackle in 1 case; that in a second-row player was unknown in 1 case and running in 1 case; and that in one three-quarter back player was tackled.
4.3. Clinical Findings
The subjective symptom was pain in the knee joint in all patients and pain localized in the lateral part of the knee in 9 patients. The swelling was observed in 1 patient and limited range of motion in 2 patients, although both were not severe. Tenderness in the lateral joint space was noted in 5 patients (45.5%). McMurray test (8) was performed in 10 patients, and 3 patients (30%) were positive. The hyperextension test (9) was performed in 10 patients, 6 of whom (60%) were positive. At presentation, Lysholm scores ranged from 48 to 69 (average 57.1 ± 5.8), VAS scores from 48 to 80 (average 59 ± 11.3), and KOOS total scores from 220 to 375.7 (average 306.7 ± 51.2). As for the status of sport activities after symptom onset, 5 patients with injury at the unknown phase of play continued to participate in the competition, and the remaining 6 patients suspended competition training, or only continued basic training (drills).
4.4. Imaging Findings
4.4.1. Radiographic Findings
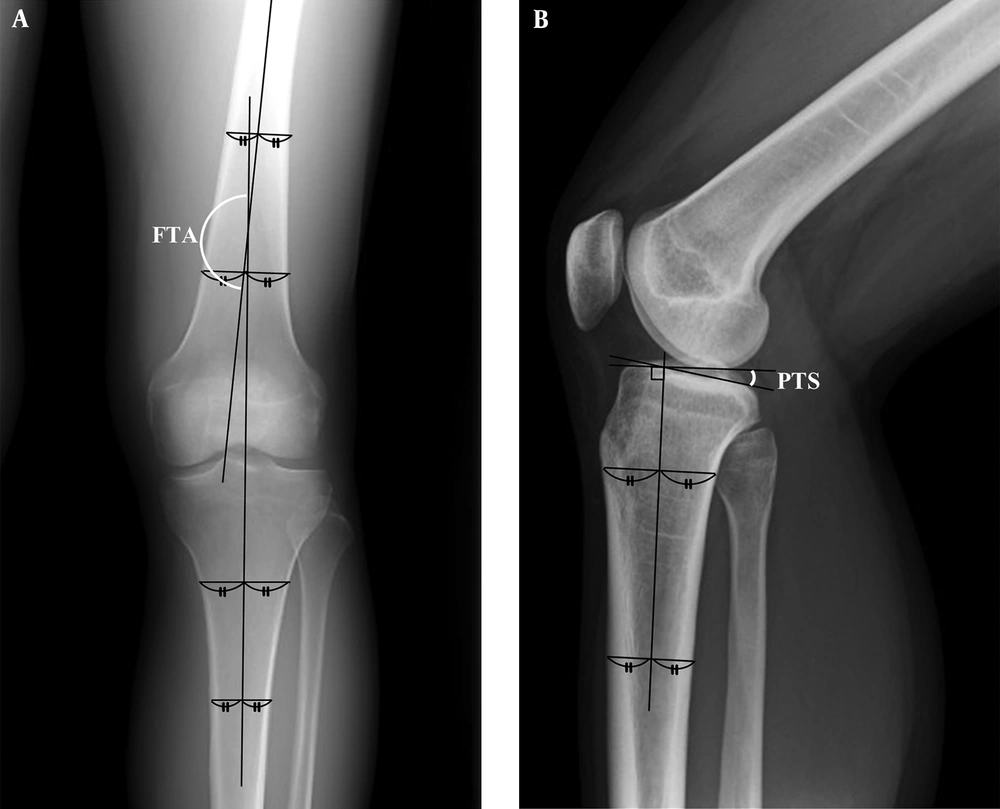
The narrowing of joint space and osteophyte formation were found in none of the patients. Femorotibial angle (FTA) ranged from 171 to 179°, with an average of 176.1° (Figure 2A). Posterior tibial slope (PTS) ranged from 3.5 to 10.5°, with an average of 7.4° (Figure 2B). Both were generally within normal ranges.
Measurements of articular axis. A, FTA: On an anteroposterior radiograph, draw two transverse lines on the femoral diaphysis. Join the midpoints of the transverse diameters to draw the femoral axis. Repeat the same procedure to draw the tibial axis. The angle between the femoral axis and the tibial axis is defined as the FTA; B, PTS: On a lateral radiograph, draw the transverse lines of the tibial diaphysis at 5 cm and 15 cm distal to the tibial articular surface. Join the midpoints of the transverse lines to draw the bone axis. The angle between the perpendicular line of bone axis and the horizontal line along the tibial joint surface is defined as the PTS.
4.4.2. MRI Findings
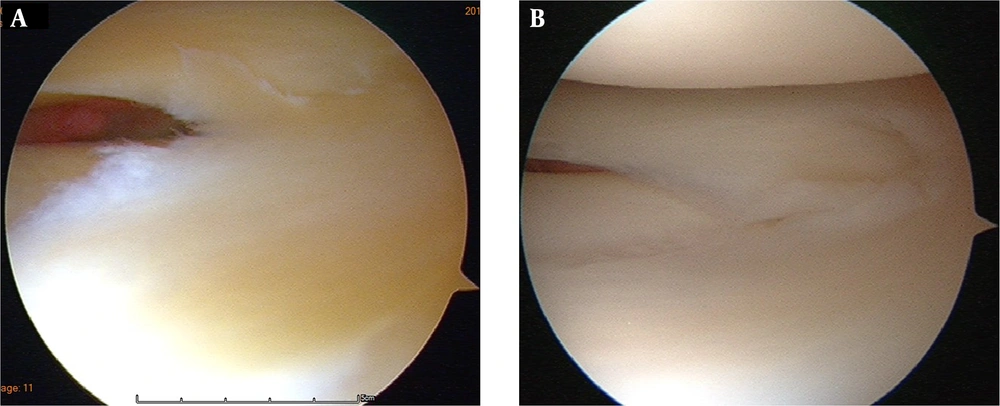
MRI in the coronal view showed abnormalities in 5 knees, but the abnormal spot-shaped or linear signal changes in radial direction were not typical. The sagittal view showed abnormal findings in all knees. In 9 (81.8%) knees, a spot-shaped meniscus partial defect was observed in the middle segment (Figure 3).
4.4.3. Arthroscopy Findings
The meniscus tear reached Cooper classification zone E-2 in 10 knees and E-3 in 1 knee. The meniscus tear patterns were a transverse tear in 6 knees and oblique tear in 5 knees (progressing toward the posterior segment in 4 knees and toward the anterior segment in 1 knee) (Figure 4).
4.4.4. Treatment Method and Outcome
The time from injury to arthroscopic examination/surgery was 5 - 16 (average 9) weeks in patients injured during tackle, 1 week in the patient injured when running, and 6 - 56 (average 21) weeks in patients injured at unknown phase of play. Arthroscopic findings showed no cases with a tear in the vascular zone corresponding to Cooper classification E-0 or E-1. Therefore, partial meniscectomy was performed in all patients (6, 10). Full weight-bearing was permitted 10 days after the operation, light exercise at jogging level was permitted at 8 weeks, and return to competition at 12 weeks. The treatment outcome at the final postoperative follow-up [follow-up period 6 - 13 (average 9.5 ± 2.9) months] was as follows: Lysholm scores 84 - 100 (average 94.8 ± 6), VAS scores 0 - 10 (average 5.3 ± 4.7), and KOOS total scores 461.4 - 500 (average 481.3 ± 12.1). All patients returned to playing rugby with no subjective symptoms.
5. Discussion
Radial tear of the meniscus is speculated to occur when rotational forces act separately on the anterior portion and posterior portion of the meniscus, and the free edge is stretched, causing a tear. Compared to the medial meniscus, the morphology of the lateral meniscus is more susceptible to radial tears, because of its sharper curve and shorter radius (11). The lateral meniscus is more mobile than the medial meniscus, and isolated lateral meniscus tears occur more frequently in a traumatic setting in younger patients (12). A radial tear divides the circumferentially oriented collagen fiber bundles in the meniscus and significantly reduces the load transmission capability, thus requires accurate diagnosis and treatment (13).
Rugby is a full-contact sport, and the frequency of injuries is high (14). The rates of injury in elite and professional rugby players were reported to be 91 - 294/1000 player-hours (15, 16). Although traumatic injuries occur in all parts of the body, the lower limb injury rate is the highest, ranging from 52% to 55%, with the knee injury rate ranging from 10% to 25% (15, 17). In addition, the rate of meniscus tears was reported to be 2.4% - 16% (18, 19).
In rugby, since the physique and the role of the player differ depending on the position, the site and frequency of injury also vary (15). McIntosh has shown that the injury rate of forwards is higher than that of backs, and the frequencies of injury during tackles and scrums are high (20). Of the 11 rugby players who had a lateral meniscus tear in the middle segment in the present study, 10 players were forwards. Among them, those playing in the front row, which is the foremost position of the scrum, accounted for one-half of the injured cases (5 cases). Although some cases were injured during tackles, the number of cases injured at the unknown phase of play was the highest. Although there is a possibility that injury is caused by a direct external force during tackles and repeated side steps and sudden stops, the injury rates of backs and third-row players are too low to support this possibility. Considering the specialized maneuvers of front-row players, the meniscus tear may be related to repeated scrums in rugby.
The average force generated in a scrum is 3370 - 6210 N, and the peak compression force during engagement reaches 8000 - 16500 N (21-23). A large proportion of this force is exerted on the front row, with an average of 3290 N (22). Under these circumstances, the compression force on the meniscus is already enormous. In addition, the knee joint position during scrum tends to be in valgus position, and the lateral joint space is narrowed, further increasing the load on the lateral meniscus. The angle of the knee joint at the time of scrum push is 130° - 155°. A study using 14 cadaver knees has shown that at 150° knee flexion, the contact pressure is the highest near the middle segment of the lateral meniscus (24, 25). These findings support the deterioration and injury of the middle segment of the lateral meniscus by the repeated push maneuvers during the scrum. Moreover, the meniscus, which is compressed under high pressure in the scrum, is pulled backward by the lateral condyle of the femur through knee extension during push, which may increase the risk of oblique tear toward the direction of the posterior segment.
For isolated lateral meniscus tears in the middle segment, the main complaint is pain near the injured site, but swelling and limited range of motion are either absent, or even if present, are mild and do not manifest severe subjective symptoms. For diagnosis of this injury, detection of tenderness and a positive hyperextension test in the clinical manual examination are relatively sensitive. In imaging examination, characteristic findings suggesting this injury are frequently observed in the sagittal view of MRI.
If this injury is left undiagnosed or untreated, there is a risk that the tear may progress and induce osteoarthritis, with the possibility that patients may not be able to continue rugby activities. Since the tears occur mostly in the avascular zone, conservative therapy is unlikely to improve the injury, and surgical therapy is considered to be the first treatment option. In general, the minimally invasive arthroscopic partial meniscectomy is selected (26). In recent years, surgical repair aiming at preserving the meniscus has been actively attempted, but the healing rate is reported to be 61%, which cannot be considered effective (10).
For rugby players in the forward position, especially in the front row, the above manual examinations are useful for clinical screening. If a lateral meniscus tear in the medial segment is suspected, it is important to confirm the injury early by MRI and arthroscopic examination, and proceed with appropriate treatment. Further studies are required to analyze the pathology of this injury as one of the harmful effects caused by rugby, as well as to develop preventive training programs and improve the scrum technique.
5.1. Conclusions
In this study, radial lateral meniscus tears involving the middle segment occurred frequently in rugby players, mostly in forward positions. Arthroscopic partial meniscectomy achieved return to play in all players.