1. Background
Anterior cruciate ligament (ACL) damage is one of the common knee injuries (1) that influence muscle function, proprioceptive sense, joint stability, movement pattern, as well as quality of life (2, 3). ACL injury could reduce the number of mechanoreceptors and perception of joint movement, which also contributes to reduced joint position sense (2, 4). These are important for postural and joint stability, leading to neuromuscular control alteration (5).
The hamstring tendon is one of the popular graft options for ACL reconstruction to reduce anterior knee pain problems and decrease donor-site morbidity (6, 7). ACL reconstruction could also affect the proprioceptive recovery of the knee joint leading to the altered sensation of correct posture and joint stability, and also reduced lower extremity muscle strength that plays an important role in knee stability (8). The single-leg squatting test could indicate the performance and strength of the hip and knee muscles using lower limb characteristics (hip flexion, hip adduction, and knee flexion) (9, 10). Abnormal knee patterns of neuromuscular control during single-leg squatting, such as knee abduction, were associated with knee valgus stress, which would increase tension to the ACL as well as dynamic valgus with knee abduction and these are considered risks of ACL injury in healthy people and re-injury in patients after ACL reconstruction (11, 12). Patients with ACL reconstruction showed impaired dynamic balance during the single-leg squat (SLS) test implying abnormal neuromuscular control of the lower extremities (13, 14).
A related study showed that the knee re-injury rate was over four times higher among patients with ACL reconstruction returning to sports three months after surgery (15). Knee flexion angle and knee alignment were demonstrated as contributors to ACL loading (1). Therefore, an understanding of lower limb muscle performance and knee proprioceptive sense at three months is crucial to evaluate and rehabilitate patients after ACL reconstruction.
2. Objectives
The study aimed to examine lower extremity muscular performance and knee proprioception in patients with ACL reconstruction using a hamstring graft at the preoperative state and three months postoperatively.
3. Methods
3.1. Participants
Twelve male volunteers (mean ± SD: Age 25.75 ± 8.56 years, height 175.17 ± 0.05 cm, body mass 74.17 ± 9.48 kg) agreed to participate in this study. All participants were recruited from a Thammasat University Hospital. Before participating, the purpose of the study, procedures, and risks were explained, and then informed consent was obtained. This study was approved by the Thammasat University Human Research Ethics Committee (COA NO.029/2560). All participants underwent ACL rupture and received a diagnosis for ACL reconstruction using hamstring grafts by a physician. Participants were excluded if they had (1) previous knee surgery, including revision ACL reconstruction surgery, or (2) any history of lower limb injury or other disorder that might have affected the capacity to complete the lower extremity performance tests. The sample size was calculated using G power (G*power version 3.1.9.2) based on the related study (16).
3.2. Procedures
All participants underwent assessments of knee proprioception and lower extremity performance before surgery and after surgery at three months. Participants were allowed to complete a standard warm-up by lower extremity stretching performed before and after each measurement. After a preoperative assessment, all participants initiated a similar home program for postoperative rehabilitation, including lower extremity muscle strength and range of motion exercises in order to return to their activity before the injury. Both legs were assessed, starting with the asymptomatic leg to prevent injury during all assessments.
3.2.1 Knee Proprioceptive Testing
Joint position sense was evaluated using a biodex system 3 isokinetic dynamometer (Biodex Medical Systems Inc., Shirley, USA) at 60°/s. The test was conducted in the standard seat position with subjects blindfolded to block visual input. The lower limb was slowly extended by participants from a starting position of 90° of knee flexion to a target angle at 15° and 60° of knee flexion, respectively. Participants were asked to concentrate on the sensation of the presented angle and memorize each specific angle for 10 s. Then the participant's knee was returned to the starting position, and the participant was asked to actively reproduce the presented joint angle, then press the stop button. Each target angle was performed three times with one-minute resting between target angles. The mean error angle was analyzed.
3.2.2. Lower Extremity Performance Testing
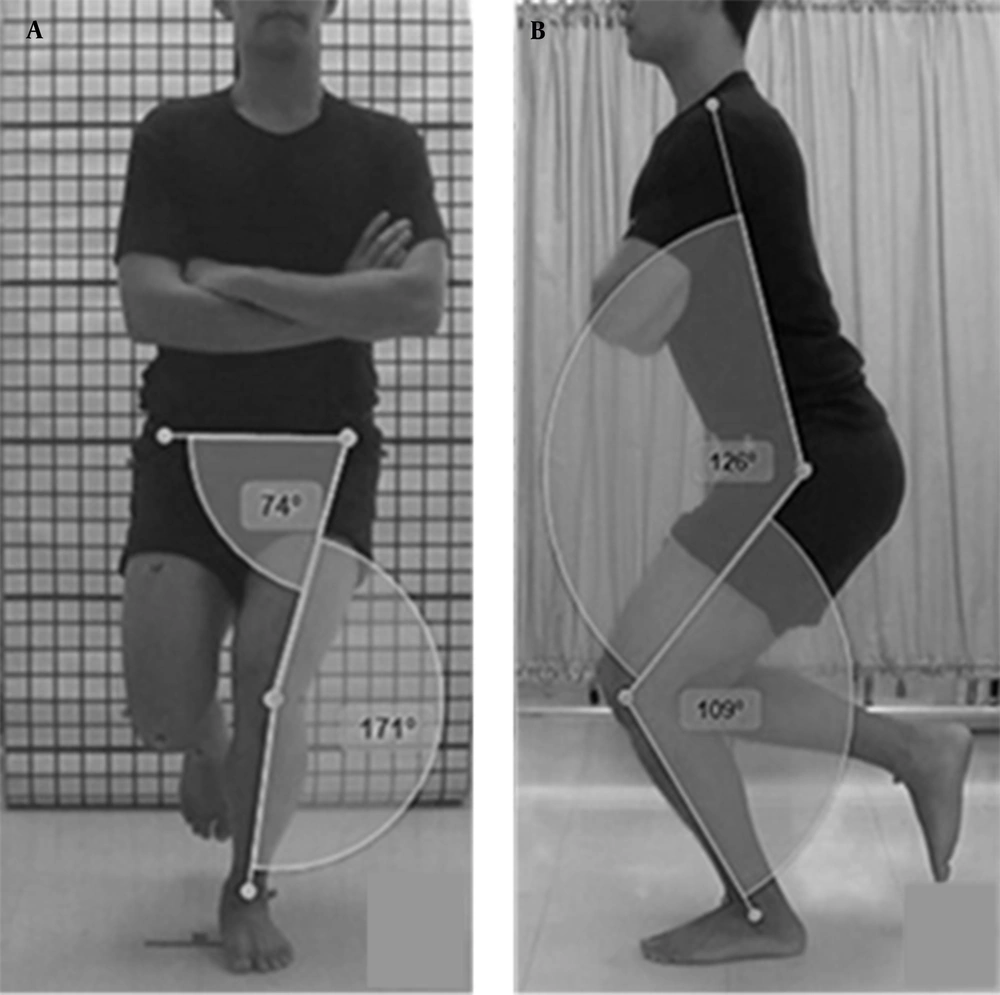
The SLS was assessed using two-dimensional motion analysis in a system comprising three video cameras with a frequency rate of 25 Hz (Sony HDR-PJ230, China), non-reflective sphere markers, and kinovea software (0.8.15) used to assess the joint angle. Three video cameras were set on the front and on the left and right sides of the participant. The height of the cameras was set, placing the center of the camera’s lens as high as the pelvis of the participant. A light-emitting diode system was placed in the testing area to synchronize the first frame. A gridline was applied to set the calibration. Marker placements were applied at both sides according to the jugular notch, acromion process, anterior superior iliac spine (ASIS), anterior thigh (in line between ASIS and knee marker), greater trochanter, between femoral condyles (anterior knee), anterior thigh (along with the line of ASIS and marker at the knee), lateral epicondyle of the femur, lateral malleolus and the middle point between both malleoli. For the SLS protocol, the participant stood with feet shoulder-width apart, then the foot in the untested limb was lifted from the floor at approximately 90° of knee flexion. Each hand was placed over the ipsilateral shoulder. The starting position was straightening of the knee, and the subject was instructed to (1) lift the untested foot from the floor, and (2) slowly squat the weight-bearing limb with the capacity to balance the body and control the knee joint behind foot level. Participants were allowed three practice trials. Then, five maximum efforts were performed continuously. Digitization was performed to define knee and hip joint angles in frontal and sagittal planes, including angles of the knee valgus, knee flexion, hip adduction, and hip flexion (Figure 1). The maximum mean angle of each joint was calculated. The test-retest reliability of the measuring single-leg squat method had already been tested and found to be high (r = 0.800 - 1.000). Knee and hip kinematics were analyzed for the SLS based on the related study of Crossley et al. in 2011 (10).
3.3. Statistical Analyses
Data were analyzed using SPSS software, version 22 (IBM, SPSS Inc., USA). The distribution of all data was calculated using the Shapiro-Wilk test. General characteristics of data were represented using descriptive statistics. Comparisons between the involved and uninvolved knee at the preoperative state and three months after ACL reconstruction were calculated using repeated ANOVA, and statistical significance was set at 0.05.
4. Results
Table 1 illustrates the demographic characteristics of participants, including related injury information.
| Characteristics | (n = 12) |
|---|---|
| Age (y) | 25.8 ± 8.6 |
| Body mass (kg) | 74.2 ± 9.5 |
| Height (cm) | 175.2 ± 0.05 |
| BMI (kg/m2 ) | 24.2 ± 3.1 |
| Injury period (mon) | 14.4 ± 15.3 |
| Meniscus injury | 7 (58.3) |
| Involved leg, right; left | 10 (83.3); 2 (16.7) |
| Dominant leg, right; left | 11 (91.7); 1 (8.3) |
| Sport type, running; football; rugby | 1 (8.3); 10 (83.3); 1 (8.3) |
| Frequency of exercise days/week (day) | |
| 0 | 1 (8.3) |
| 1 - 2 | 2 (16.7) |
| 3 - 4 | 5 (41.7) |
| > 4 | 4 (33.3) |
| Exercise duration | |
| 30 mins | 1 (8.3) |
| 30 mins - 1 hr | 3 (25) |
| 1 - 2 hrs | 5 (41.7) |
| > 2 hrs | 3 (25) |
Characteristics of Participants a
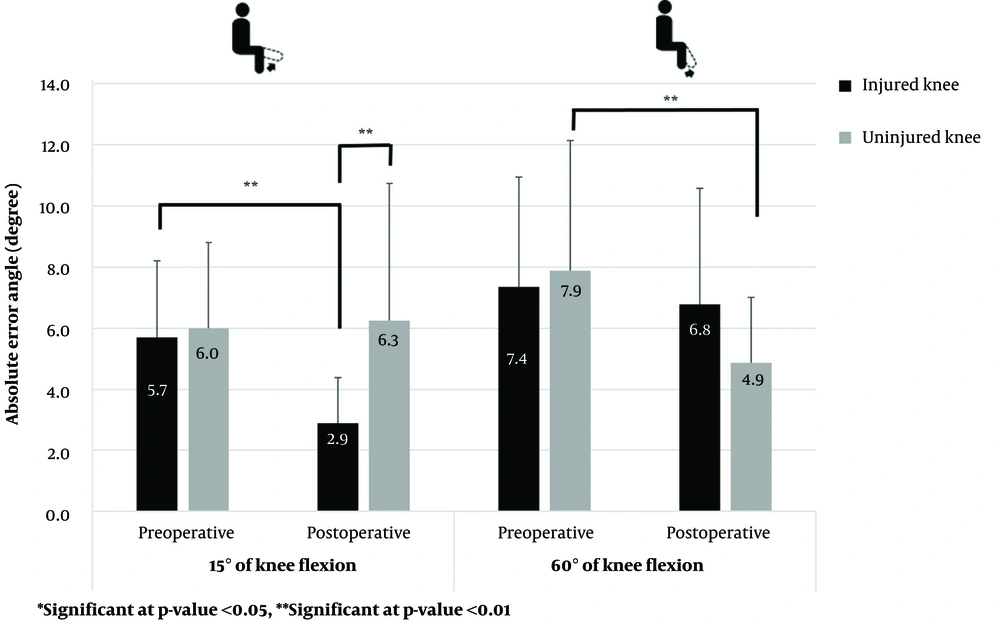
A comparison of knee proprioception (injured and uninjured knees) at 15 and 60-degree-target angles between preoperative and three months after ACL reconstruction is illustrated in Figure 2. A significantly lower mean absolute error angle at 15 degree-target angle was found between preoperative and three months after ACL reconstruction of the injured knee (P = 0.04). However, the uninjured knee showed statistically significant differences between the preoperative state and three months after ACL reconstruction at a 60-degree-target angle (P = 0.01). Although no statistical difference was found in the injured knee at 60 degree-target angle between the preoperative state and three months after ACL reconstruction, the mean absolute error angle was lower three months after ACL reconstruction than that of the preoperative state. In addition, comparing injured and uninjured knees regarding the proprioceptive test at three months from ACL reconstruction revealed significant differences at 15 degree-target angle (P = 0.01).
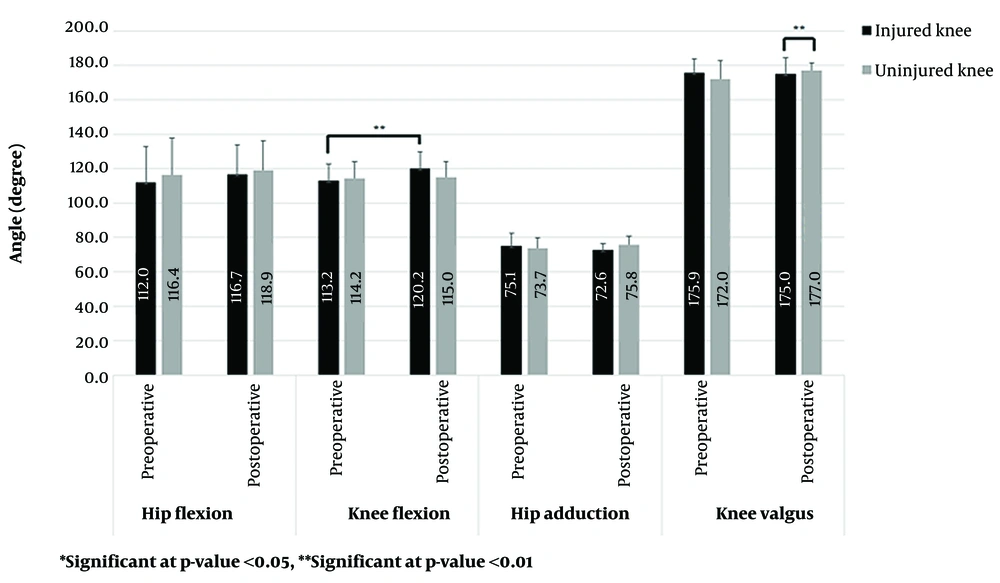
Figure 3 shows comparisons of the SLS (mean, SD) between preoperative and three months after ACL reconstruction at both knees. In the sagittal plane, knee and hip muscle functions at the injured side indicated decreasing performance (higher measured angle) after reconstruction. However, only the mean knee flexion angle in the injured knee showed a significant difference (P = 0.03). In the frontal plane, the knee valgus and hip adduction of the injured knee were found to be greater (lower measured angle) postoperative when compared with preoperative values. For statistical analysis, a significant difference was found in the postoperative valgus angle between injured and uninjured knees (P = 0.04).
5. Discussion
5.1. Knee Proprioception and ACL Reconstruction
Our findings were similar to a related study in that knee proprioception after ACL reconstruction using patellar tendon autograft three months afterward tended to improve in knee extension (0° to 20°) (17), whereas mid-range (40° to 60°) did not significantly differ. The ligament and capsule were more stretched at the end-range than mid-range position facilitating Ruffini and Golgi tendon receptors to raise proprioceptive awareness (18). The end range of knee extension is important for weight-bearing activities such as the stance phase of walking (19). A previous study showed that knee proprioceptive sense at 15° of knee flexion after reconstruction within six months could improve due to remodeling and improving the proprioceptive receptors (20). On the other hand, one study suggested that only 1% of the ACL area was composed of mechanoreceptors of proprioception, and ACL tear or ACL reconstruction may not alter knee joint proprioception (21). In addition, the average time injury before reconstruction could influence the knee joint proprioceptive sense in that mechanoreceptors in ACL seem to decrease one year after ACL injury (22). Additionally, a related study found that the joint position sense in the uninjured knee had a lower mean error angle than that of the injured knee (23). This result is similar to our study at 60° of knee flexion in particular. Bilateral proprioceptive changes may have affected both limbs after ACL injury with the mechanism of affecting afferent information from receptors at the ligament, muscle, joint, and skin (24, 25). These related to the functions of the hamstring and quadriceps, which better recognized positions with greater knee flexion angle (26). Knee proprioception with a small range of knee flexion is accompanied by standing and walking movements, whereas proprioception in a large range of knee flexion would relate to improved muscle function.
5.2. Single Leg Squat Test and ACL Reconstruction
An isokinetic dynamometer is a common tool for measuring muscle strength with high reliability and remains valuable for detecting muscle function and imbalance regarding knee problems (26, 27). However, it cannot directly indicate the level of muscle function. The SLS test involves a complex movement pattern within the kinetic chain (28, 29) that may indicate the ability of neuromuscular control (30). Our results revealed that decreased hip and knee flexion angles were found at the injured side between preoperative and 3 months-postoperatively, especially in the knee middle range angle. A deficit of the eccentric contraction of the quadriceps muscle is related to a reduction in the knee flexion function (30, 31). Our findings also supported that proprioception of knee flexion at 60° showed no improvement of the injured side postoperatively. Decreased neuromuscular control could be explained by losing ACL mechanoreceptors, disrupting ligamentous muscular reflex between ACL and the quadriceps muscle, and impaired quadriceps after long-term injury of the knee, including muscle activation and muscle weakness (31, 32). Our results showed that the injured leg had a greater knee valgus angle than the uninjured leg. This could result from impaired neuromuscular control (12). Poor neuromuscular control could be defined with increased hip adduction and knee valgus angle moments related to the gluteus medius muscle (33). The impaired neuromuscular control referred to hip adduction, and the knee valgus was also found while squatting down with reduced quadriceps and hamstring muscle action to control the knee during dynamic joint stability.
These could suggest that the injured knee three months after reconstruction exhibited inadequate knee muscle strength and knee proprioception, especially in the middle range. However, many factors may influence the results, including the period between the onset of injury and surgery date, characteristics of injury (isolated ACL and ACL with meniscus), and individual physical activity (22, 34, 35). These may involve performance adaptation and compensation from the injury period until rehabilitation period. Further studies should consider these factors.
5.3. Limitations of the Study
The rotation of the hip may result from the valgus angle during SLS test in the frontal plane. Three-dimensional motion analysis should be confirmed in the future. Our study did not control the rehabilitation program and activity after reconstruction, but the physician followed up on the participants' status and their program every month. However, the rehabilitation program should be modified and controlled in the future.
5.4. Conclusions
After three-month ACL reconstruction, proprioception and hip-knee muscle performance were found to improve at the end range of knee extension, while the middle range of knee extension showed deficits in knee joint position sense and hip-knee muscle performance. This would emphasize that improved hip and knee neuromuscular control is an essential component of rehabilitation programs designed for patients undergoing ACL reconstruction.