1. Background
Before the COVID-19 pandemic, there was debate about the effectiveness of wearing face masks in public in reducing the spread of respiratory infections, as there was no reliable and consistent evidence to support their use. However, given the primary route of transmission of COVID-19, airborne droplet mask use appears to be a practical non-pharmacological approach (1). Thus, respiratory protective devices are considered essential initial strategies to prevent the spread of the disease (2). Currently, N95 face masks provide the highest level of infection protection, followed by surgical face masks (3). However, some research shows that while wearing a mask is an effective strategy to reduce the spread of the virus, some are concerned that wearing a mask throughout the day can harm the cardiovascular system, especially during exercise. This is because when using surgical masks and N95 masks, increased physical stress may be accompanied by increased heart rate, respiratory resistance, exertion perception or dyspnea, decreased maximum body performance and ventilation, overall discomfort, and fatigue. The rates were higher for N95 masks than for surgical masks (4-7). Using face masks increases breathing resistance and reduces the intake of sufficient oxygen. This hypoxia stimulates the sympathetic nervous system and increases the heart rate (7, 8). Respiratory facemask-induced hypoxia is a physiological condition affecting the heart's autonomic regulation (9). Cardiac autonomic function refers to the parasympathetic and sympathetic activity of the autonomic nervous system branches, the ANS, which regulate the heart. The parasympathetic and sympathetic nervous system effects can be measured using heart rate variability (HRV), a measure that quantifies cardiac ANS activity (10, 11).
Given that the usage of face masks has produced mixed outcomes, it is important to look at the effects of wearing one, particularly when exercising. Steinhilber et al. showed that respiratory masks might "have negative impacts on all aspects of aerobic life, with ramifications for the individual's physical, psychological, and social well-being." (12). Fikenzer et al. showed surgical masks and N95 masks have a negative impact on exercise parameters such as VO2max and maximum power output. These negative effects are more obvious in the N95 mask than in the surgical mask, and as a result, the use of face masks can reduce the athlete's performance (13). Conners et al. showed that during anaerobic exercise, wearing a mask increases the heart rate and rate of perceived exertion when compared to not wearing a mask. This may have an impact on legislation and association rules requiring the use of facial coverings while exercising (6). Ramos-Campo et al. demonstrated that using an FFP2 or a surgical mask during resistance training had no effect on HR, heart rate variability (LF, HF, LF/HF, SDNN, RMSSD, SD1, SD2), or mean intervals (RR) (14). Tornero-Aguilera and Clemente-Suarez showed that using a surgical mask during a 150-minute college lesson produced an increased HR and a decreased SPO2, with no significant effect on mental fatigue perception or response (LF, HF, SD1, SD2) (15). In contrast, a study by Lassing et al. showed that airway resistance and heart rate during steady-state exercise increased with surgical face masks in healthy volunteers. But, the aerobic performance was unchanged (5). These findings may provide important information for athletes and coaches on the physiological impact of face masks compared to the protective effect during exercise, which must be carefully considered (6).
In addition, various research has been conducted in the field on the physiological impact of face masks on acute aerobic and anaerobic exercise performance, but there has been no research on the effect of different face masks during long-term high-intensity interval training. High-intensity interval training (HIIT) includes a frequent series of high-intensity tries followed by changing recovery times. One of its main benefits over other methods is that it gets even better results in a shorter session time (16). Whole-body-based high-intensity interval training (HIIT) is an alternative strategy to consider improving the parameters used to measure fitness (17). HIIT can be an effective solution for people struggling to maintain the right level of physical activity (18) because it can promote significant adaptations in strength, hypertrophy, body composition, and the cardiorespiratory system (16). HIIT exercise also reduces anxiety, stress, and depression and increases resilience during periods of COVID-19 suppression (19).
2. Objectives
The purpose of this study was to determine the effect of four weeks of functional high-intensity interval training with two types of masks (N95 versus surgical masks) on adaptation of the cardiac autonomic system in healthy men. According to the contents, it was hypothesized that the 4-week HIIT without a mask compared to the surgical and/or N95 causes higher physiological adaptation in markers of the cardiac autonomic system such as (RMSSD, SD1, HF, LF, LF/HF). Furthermore, it was hypothesized that the adaptation in cardiac autonomic system markers to HIIT with a surgical mask was superior to that with an N95 mask.
3. Methods
3.1. Ethical Approval
All methods for this study have been approved by the local institutional ethics committee. (Code of ethics: IR.UMZ.REC.1399.011) and conducted by the most recent revision of the Helsinki Declaration. Before commencing the study, subjects were familiar with the experimental procedures, protocols, and equipment. All subjects then gave informed consent. Subjects could ask questions about any part of the protocol and withdraw at any time without penalty.
3.2. Subject’s Classification and Eligibility Criteria
Eighteen healthy male volunteers were randomly assigned to experimental (N95 mask, surgical mask) and control (no mask) groups and performed the functional HIIT protocol. All subjects had no orthopedic trauma at the time of the survey. Criteria for entering the study: 20 - 45 years old, without chronic disease history, including; cardiovascular disease, high blood pressure, diabetes mellitus, chronic bronchitis and cough, arthritis, cancer, and without a smoking history. In contrast, the exclusion criteria in the current search area are as follows; having SpO2 < 95%, having one sign of acute respiratory disease or fever symptoms, as well as clinical signs that cannot be explained by any other illness, such as systolic blood pressure of 90 mmHg, diastolic blood pressure of 95 mmHg, travel history to another country/state within 14 days prior to experience, and close contact with a COVID-19 patient confirmed by RT-PCR test.
3.3. Protective Facemasks Modality
Although all masks are primarily considered effective in protecting people from viruses and respiratory infections, surgical and N95 masks are forms of facial personal protective equipment (PPE). They were the most commonly used and were therefore considered for this study (20).
3.4. Weight-based Functional HIIT Protocol
The body weight-based interval training protocol was adapted from studies by Klika and Jordan (21), as well as from other studies, and implemented with a few modifications (17, 19, 22). The subjects performed the training protocol for four weeks and three weekly sessions. In the first and second weeks, it was three times a week; in the third and fourth weeks, it increased to four times a week. In addition, the duration of each set was 20 seconds in the first week, increased to 25 seconds in the second and third weeks, and reached 30 seconds in the final week. The rest between sets was 30 seconds in all weeks and 60 seconds between each level of training. The subjects used only their body weight to perform the exercises (21). The training protocol consisted of nine stops; air squats, push-ups, lunges, high knee, jumping lunges, butterfly, jump squats, seated leg circles, and back extension exercises with an average heart rate of 170 - 180 beats per minute (80 - 90% of maximum heart rate). The training program lasted for 45 - 60 min. The mask groups used face masks in all stages of the training. The warm-up and cool-down took 10 minutes.
3.5. Maximal Exercise Test and ECG
All testing procedures were performed at the Evaluation and Monitoring Health Center (MECH). First, all subjects performed a warm-up for 5 min at the primary treadmill speed and then performed a typical exercise electrocardiogram test using the modified Bruce protocol. During tests, the operator continuously monitored the participant’s status and recorded SBP, heart rate, presence of chest pain, and ECG changes in the stage of the rest, modified Bruce test, as well as the recovery phase, the fifth minute of the post-exercise. Exercise electrocardiograms using the modified Bruce protocol were finished when the subject's heart rate reached 80 - 90% of the predicted HR Max. The modified Bruce protocol details are taken from the article (20).
3.6. Cardiac Autonomic System
Heart rate variability has been used to study the autonomic nervous system of the heart. Kubios software (version 3.4.2) was used to analyze the HRV indicators. Kobius is free, non-commercial software for researchers and doctors (http://Kubius.uef.f7). The software can analyze HRV in the time domain, frequency domain, and nonlinear index. Compatible with Windows and Linux operating systems, Kobius supports ECG and RR data formats (22). The heart rate variability indices such as; (LFn.u), (HFn.u), (LF/HF), (RMSSD), (SD1) were evaluated (23). The R-R interval for 5 minutes in a sitting position (resting phase, modified Bruce test, and recovery phase) is saved by Custo med software (24).
3.7. Anthropometric and Physiological Measurements
The anthropometric and hemodynamic parameters of subjects were as follows: height and weight were measured by scales and a digital stadiometer. The digital stadiometer had an accuracy of 0.1 cm and 0.1 kg for height and weight. The body mass index (BMI) was calculated by the Body Composition Analysis System (Korea, Boca x1, Medigate Inc), Waist-to-hip ratio (WHR), peripheral blood oxygen saturation (SpO2) was measured with a portable pulse oximeter (China, model PO16, Brisk). Subjects were asked to wear an oximeter on the index finger of their non-dominant hand (25), and blood pressure with an automatic blood pressure monitor (Switzerland, model ME701, Rossmax). VO2max (mL/kg/min), was measured as well as the rate of perceived exertion (RPE) scale (26). In addition, the heart rate was continuously recorded using a 12-lead ECG. All measures were performed after a 5-min resting and recovery phase in the sitting position.
3.8. Statistical Analysis
All statistical analyses were performed using SPSS for Windows, version 25.0. Group distributions were analyzed using the Shapiro-Wilk test. Due to the normality of the data, a parametric statistical method was used for analysis. A two-way ANOVA and HSD Bonferroni post hoc tests were used to assess the differences between the groups. The mean value SD is used to represent all data. Statistical significance was set at P ≤ 0.05.
4. Results
Anthropometric and physiological parameters such as age, weight, BMI, WHR, RPE, blood pressure (rest, recovery), HR (rest, recovery), SPO2 (rest, recovery), VO2max, and distance traveled on the treadmill before and after HIIT exercise are shown in Table 1. After four weeks of HIIT exercise with a surgical mask and N95 mask, and without a mask, hemodynamic and anthropometric data showed that body mass index, resting heart rate, recovery blood pressure, recovery heart rate, and RPE decreased. Also, increased VO2max, SPO2, and distance were observed in all three groups compared to before HIIT exercise.
| Index | Pre | 4 Weeks | ||||
|---|---|---|---|---|---|---|
| N95 | SUR | No Mask | N95 | SUR | No Mask | |
| Age, y | 27.8 ± 7.4 | 28 ± 3. 2 | 29.3 ± 9.2 | - | - | - |
| Weight, kg | 77.8 ± 7.5 | 79.4 ± 19.3 | 77.8 ± 11.8 | 77.4 ± 7.4 | 78.6 ± 14.1 | 77.4 ± 8.8 |
| BMI | 24.3 ± 2.8 | 26.3 ± 4.5 | 23.6 ± 1.6 | 24.1 ± 2.9 | 26.1 ± 3.3 | 23.4 ± 1.1 |
| WHR | 0.83 ± 0.05 | 0.83 ± 0.03 | 0.83 ± 0.01 | 0.81 ± 0.04 | 0.83 ± 0.03 | 0.82 ± 0.03 |
| SPO2 | ||||||
| Rest | 96 ± 1.6 | 96 ± 1.7 | 98 ± 1.0 | 98 ± 1.2 | 98 ± 2.1 | 98 ± 0.8 |
| Recovery | 93.5 ± 1.4 | 92.2 ± 0.8 | 95.2 ± 1.2 | 95.8 ± 1.2 | 95.5 ± 1.5 | 97.8 ± 1.2 |
| BP, mmHg | ||||||
| Rest (DBP) | 72 ± 11 | 64 ± 11 | 74 ± 9 | 73 ± 5 | 67 ± 9 | 79 ± 7 |
| Recovery (DBP) | 78 ± 12 | 63 ± 8 | 77 ± 9 | 82 ± 9 | 74 ± 11 | 80 ± 8 |
| Rest (SBP) | 114 ± 16 | 101 ± 19 | 125 ± 19 | 123 ± 8 | 110 ± 9 | 120 ± 7 |
| Recovery (SBP) | 174 ± 6 | 171 ± 9 | 163 ± 9 | 140 ± 10 | 142 ± 8 | 138 ± 9 |
| HR | ||||||
| Rest | 87 ± 8 | 86 ± 7 | 81 ± 5 | 82 ± 4 | 80 ± 6 | 75 ± 3 |
| Recovery | 138 ± 9 | 141 ± 4 | 135 ± 7 | 125 ± 10 | 128 ± 7 | 119 ± 6 |
| VO2max, mL/kg/min | 38.6 ± 3.2 | 38.4 ± 4.9 | 40.7 ± 3.3 | 50.7 ± 2.5 | 49.1 ± 1.7 | 50.7 ± 1.9 |
| RPE, 20 scale | 19 ± 1 | 20 ± 1 | 17 ± 1 | 16 ± 2 | 17 ± 1 | 15 ± 2 |
| Distance, m | 1129 ± 200 | 1112 ± 200 | 1301 ± 230 | 1368 ± 270 | 1317 ± 290 | 1465 ± 140 |
Changes in Anthropometric and Physiological Parameters Before Functional HIIT and Following 4-weeks of Functional HIIT
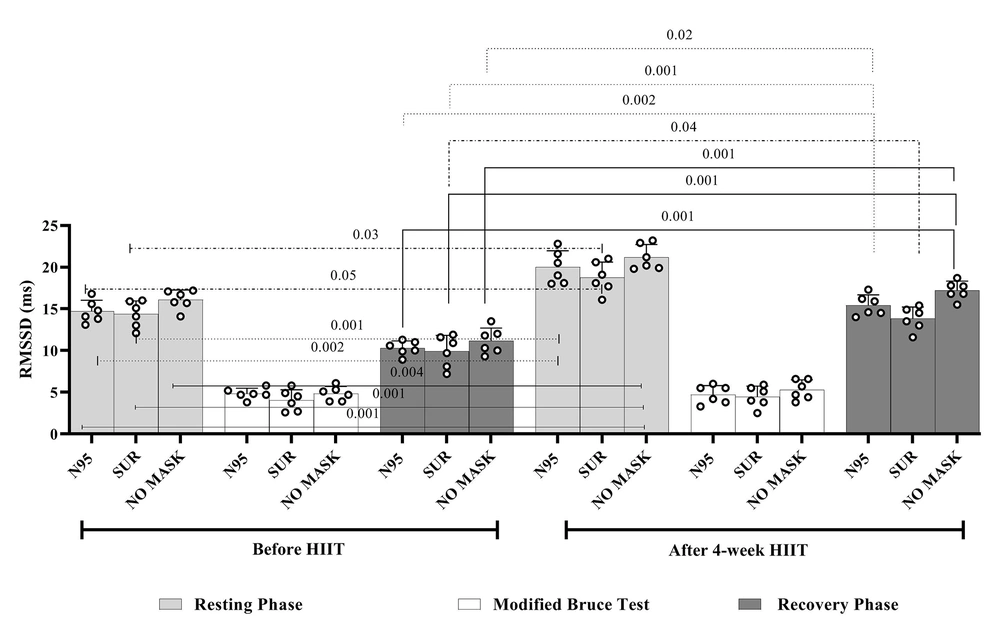
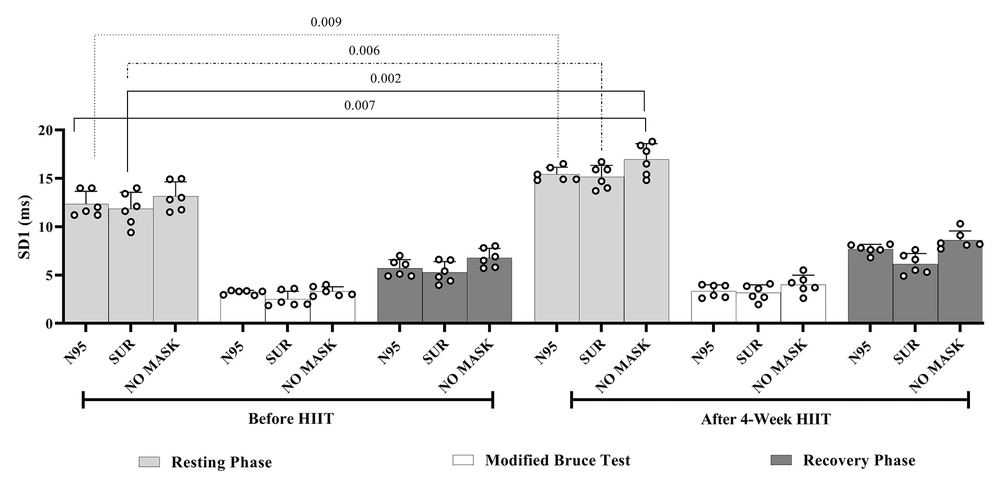
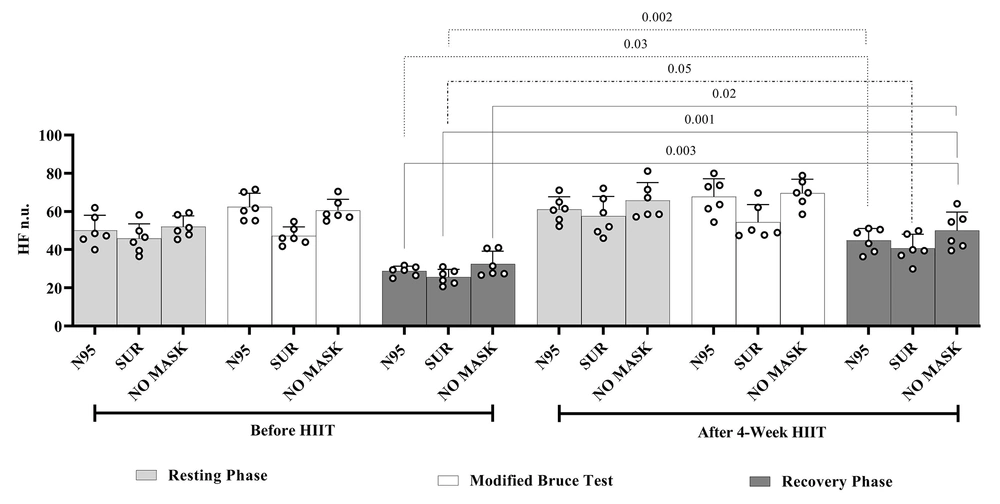
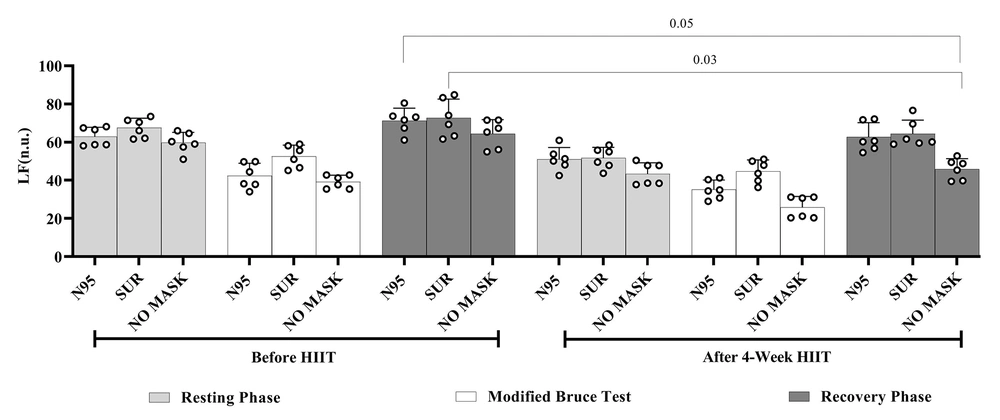
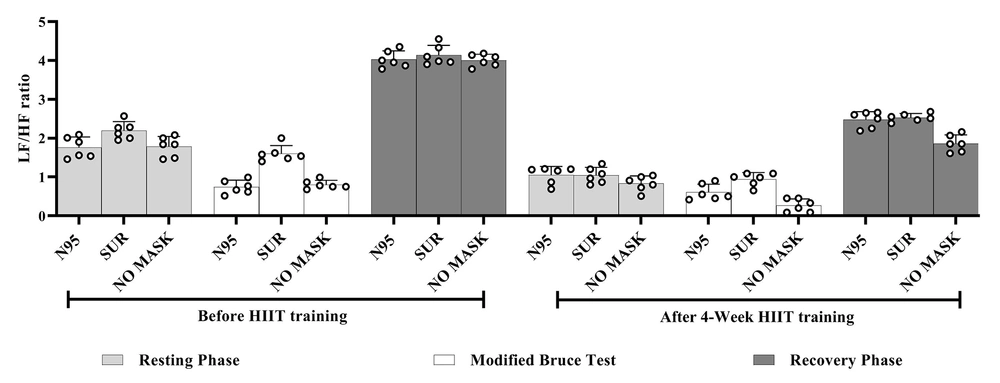
Performing four weeks of functional HIIT exercise resulted in changes in the cardiac autonomic system so that the 4-week adaptation to functional HIIT exercises improved resting parasympathetic indices (RMSSD for N95, surgical and no mask groups (P ≤ 0.05), (see Figure 1), and (SD1 for N95, surgical and no mask groups (P ≤ 0.05), (see Figure 2) compared to baseline levels. However, this increase in resting parasympathetic tone was more evident in the N95 mask group than in the surgical mask group. The 5-minute recovery of the cardiac autonomic system after exhaustion training on a treadmill following compatibility with regular exercise of functional HIIT exercise improved in favor of parasympathetic tone (RMSSD for N95, for surgical and no mask groups (P ≤ 0.05), and HFn.u for N95, for surgical and no mask groups (P ≤ 0.05) (see Figures 1 and 3) compared to baseline levels. Therefore 4-week adaptation to HIIT exercises led to faster recovery of sympathetic indices (LFn.u 0.03, 0.05, LF/HF (see Figures 4 and 5) in the no mask group, compared to the surgical and N95 groups, before functional HIIT exercise, also when compared to surgical and N95 groups after 4-weeks of HIIT. Performing the modified Bruce test before and after four weeks of HIIT showed a statistically not significant difference in the values of LF, LF/HF, RMSSD, HF, and SD1 in the resting and recovery phases between the experimental groups (surgical mask vs. N95). as well as compared to the control group (no mask) did not create.
5. Discussion
The most important findings of the present study were that running on a treadmill after 4 weeks of functional HIIT improved the resting cardiac autonomic system by significantly increasing parasympathetic parameters (RMSSD, SD1). They significantly increased the parasympathetic recovery index (RMSSD, HFn.u) and faster recovery of sympathetic parameters in all three groups. These findings confirm that high-intensity exercise with a surgical mask or N95 mask has no negative effect on the functioning of the cardiac autonomic system.
Studies support our results; Otsuka et al. show that wearing a surgical mask during intense exercise does not affect the cardiopulmonary system performance (27). In a study, Shaw et al. showed wearing surgical, N95, or cloth masks during exercise does not affect performance and has the least effect on physiological indexes (28). In another study, Shaw et al. showed that wearing a surgical and cloth mask during intense exercise has no discernible detrimental effect on exercise performance in young, healthy participants (29). Epstein et al. showed short-term moderate-high aerobic physical activity with surgical masks, and N95 masks in healthy subjects is possible, safe, and associated with only minor changes in physiological parameters such as respiratory rate, HR, BP, SpO2, and time to fatigue (30). Barak et al. showed that the post-short-term submaximal exercise time domain (RRNN, SDNN, and RMSSD) was significantly lower than baseline values. Post-exercise lnLF and lnHF are significantly reduced during recovery compared to baseline (31). In another study, Heffernan et al. showed acute resistance exercise in young, healthy men decreased HF, HFn.u, and increased LF, LFn.u, and LF/HF after 5 min of post-exercise (32). Munk et al. show a significant increase in rMSSD after HIIT, suggesting a possible shift in the mechanism to increased parasympathetic activity and decreased sympathetic activity (33). In another study, Besnier showed that three weeks of intense interval training increased (HFnu%) and LF/HF HRV (34). The lack of difference between the N95 mask and surgical mask after 4 weeks of HIIT exercise compared to HIIT without a mask can probably be attributed to adaptation to hypoxia conditions with a face mask (7), which in the present study improved physiological parameters such as VO2max and decreased resting and recovery heart rate and recovery blood pressure. In the present study, the N95 mask group had a lower RPE and traveled a longer distance on the treadmill compared to the surgical mask group. Wearing an N95 mask with a valve that reduces the breathing resistance during exhalation allows for better ventilation (3, 35). On the other hand, wearing surgical masks in high-intensity training causes a considerable rate of abrupt exercise cessation due to acute dyspnea associated with the suction of the wet and deformed mask (36). Studies have suggested that immediate vagal reactivation after exercise is independent of exercise intensity (37). Post-exercise HRV may be superior to the analysis of resting conditions for athletic monitoring performance, as it may show improved recovery from training with exercise (38). Mechanisms involved in post-exercise autonomic regulation, such as central control retraction and cardiopulmonary and arterial organ activity, may also depend on the intensity of the previous exercise (37).
Essentially, the decrease in resting heart rate (RR interval) has been identified as one of the first adaptations of the heart in response to repetitive exercise. This adaptation can be explained by alternative improvements in vagal activity (parasympathetic activity) (39). On the other hand, HIIT training can be used as an effective program to improve the heart's ability for auto-regulation. Although the underlying mechanisms by which exercise enhances vagal regulation are currently speculative, angiotensin-II and nitric oxide (NO) levels, catecholamines, and beta-adrenergic receptor density are potential mediators that improve cardiovascular ANS. HIIT may increase the bioavailability of nitric oxide (NO) and potential mediators that enhance exercise-induced autonomic regulation of the heart. HIIT can also cause more significant carotid artery dilation, related to improved baroreflex sensitivity (40). HIIT has a more remarkable ability to stimulate the synthesis of nitric oxide (NO) by the endothelium because shear stress is promoted in the vascular wall during periods of high intensity. The bioavailability of this oxide, promoting excitability in vagus neurons, is also regulated by endothelial NO (34, 41). Lower angiotensin-II in athletes is associated with a higher degree of cardiac vagal activity. That inhibition of angiotensin-II by exercise may, to some extent, mediate improvement in vagal heart tone. The decrease in angiotensin-II level after physical training is an important mechanism that promotes the increased activity of the parasympathetic nerve (41).
5.1. Conclusions
This study was the first to investigate the effects of long-term exercise training with face masks on the autonomic nervous system and physical parameters in healthy men. The results of the present study showed that the use of medical face masks during exercise training is safe and has no negative adverse effect on cardiac autonomic function in healthy men. This data may impact the wearing of face masks while exercising or exercising indoors. Some limitations in the study should be acknowledged. First, due to the particular circumstances of the general public in the COVID-19 pandemic, in this study, the effect of the surgical mask and N95 mask was not tested in a large number of subjects, and only healthy men between 20 and 40 years old were present, and whether these results can be achieved in women, the elderly, and children needs to be investigated. Second, only healthy, non-smoking individuals were included. Therefore, the results of this study cannot be generalized to clinical populations such as heart failure patients, chronic obstructive pulmonary patients, or people who survived the COVID-19 virus. This is important given that smoking can alter the cardiac autonomic system. Third, different mask models that may affect physiological performance were not investigated. Different mask models and designs may have different effects on various physiological parameters.