1. Background
Insufficient physical activity is a major risk factor underlying noncommunicable diseases (NCDs) (1), which remains the leading cause of death globally (2). Lack of time has been indicated as the most common barrier to physical activity (3). High-intensity interval training (HIIT) or sprint interval training (SIT) has been claimed as a time-efficient exercise for overcoming this barrier (4). There are many health benefits of HIIT/SIT, including improved cardiorespiratory fitness, vascular function, and insulin sensitivity (5). However, HIIT requires more time than the exercise recommendations for vigorous-intensity aerobic exercise (75 min per week) (6). Some researchers have suggested that HIIT/SIT requires extremely high motivation and high levels of exertion while training (4, 7). It might be assumed that HIIT/SIT might not be practical and safe for some individuals, such as those with a sedentary lifestyle. Therefore, HIIT/SIT protocols with fewer or shorter sprints must be developed to address the limitations of conventional HIIT/SIT.
Reduced-exertion high-intensity interval training (REHIT) is a modified SIT protocol consisting of 2 repeated 20-s all-out sprints within a total exercise duration of 10 min (8). It is well established, based on several studies, that REHIT has improved maximal oxygen consumption in healthy individuals (9, 10), patients with type II diabetes (11), and a patient with cystic fibrosis (12). Moreover, insulin sensitivity improved following REHIT in healthy young men (8). These studies did not report serious adverse effects during and after REHIT. However, it might be too early to conclude that REHIT is safe for the general population, especially for individuals with cardiovascular risks, such as inactive or overweight/obese individuals (13, 14).
Arterial stiffness (AS) is a marker for cardiovascular risk, and it can be evaluated using non-invasive techniques such as the measurement of pulse wave velocity (PWV) (15). Increased AS is associated with an increase in the risk of cardiovascular diseases (16). Although several studies have demonstrated that AS improves following exercise training (17, 18), vigorous activity acutely increases AS both in normal-weight (19, 20) and overweight/obese individuals after exercise (21). This might be related to an increased risk for cardiovascular complications of exercise (22). Acute SIT can also induce a transient increase in AS following exercise (20). However, some studies contradict this understanding (23-25). Presently, it remains unknown if REHIT influences AS.
2. Objectives
To determine the acute effects of REHIT on AS in normal-weight and overweight/obese individuals.
3. Methods
3.1. Participants
We estimated that a sample size of at least 24 participants would be required to identify a small effect size (d = 0.25), with a power of 0.80 at an alpha level of 0.05 (G*Power version 3.0.10, Heinrich Heine University, Düsseldorf, Germany). Normal-weight and overweight/obese individuals (n = 12 per group) aged 21 - 23 years participated in this study. All participants had insufficient activity levels (physical activity level < 600 metabolic equivalent (MET)-min.week-1) (see Table 1 for the participants’ basic characteristics). Overweight/obesity was classified as having a body mass index (BMI) of more than 23 kg/m2 (26). None of the participants had been diagnosed with any chronic diseases (e.g., cardiovascular, respiratory, or metabolic diseases), lower limb injuries, and/or joint pain in the past six months, had regular medication use, or smoked. Participants classified as having moderate to high physical activity, as determined using the International Physical Activity Questionnaire (IPAQ) (27), and those with contraindications to exercise according to a physical activity readiness questionnaire (PAR-Q) (28) were excluded from this study. This study was approved by the Human Research Ethics Committee of Thammasat University (Science) (COA No. 074/2564) in accordance with the Declaration of Helsinki. All participants provided written informed consent before participation.
| Parameters | Normal Weight (n = 12) | Overweight/Obese (n = 12) |
|---|---|---|
| Age (y) | 21.9 ± 0.8 | 21.9 ± 0.5 |
| Height (cm) | 162.6 ± 35.8 | 164.8 ± 79.1 |
| Weight (kg) | 55.4 ± 3.5 | 73.4 ± 13.9 b |
| BMI (kg/m2) | 21.0 ± 1.2 | 27.1 ± 5.2 b |
| Resting heart rate (bpm) | 82.3 ± 11.5 | 78.7 ± 2.9 |
| Systolic blood pressure (mmHg) | 113.2 ± 9.1 | 117.4 ± 8.6 |
| Diastolic blood pressure (mmHg) | 67.8 ± 7.0 | 68.4 ± 6.0 |
| baPWV (cm/msec) | 1079.5 ± 134.2 | 1030.1 ± 181.6 |
| Physical activity level (MET-min.week-1) | 113.5 ± 144.6 | 72.1 ± 99.0 |
Abbreviations: baPWV, brachial-ankle pulse wave velocity; BMI, body mass index; MET, metabolic equivalent.
a Data are presented as the mean ± SD.
b P < 0.05, significantly different from the normal-weight group.
3.2. Experimental Protocols
The experiment was conducted in the morning. All participants were requested to refrain from consuming caffeine or alcohol and perform vigorous exercise for 24 h before the test. Female participants were examined during days 1 - 7 of the menstrual cycle to avoid capturing the effects of hormones on AS (29). After measuring height and weight, the participants rested supine for 5 - 10 min in a temperature-controlled condition. The AS and cardiovascular parameters were assessed before and post-exercise (1, 30, and 60 min).
3.2.1. AS
Arterial stiffness was assessed in terms of the brachial-ankle pulse wave velocity (baPWV) using a non-invasive vascular screening device (VP-1000 plus, Omron Corporation, Kyoto, Japan) (30). Bilateral brachial and posterior-tibial arterial pressure waveforms were determined using air plethysmography and an oscillometric pressure sensor wrapped on both arms and ankles. Electrocardiogram (ECG) electrodes were placed on both wrists, and a phonocardiogram sensor was placed on the chest. The baPWV was automatically calculated using the VP-1000 Plus device using height-based formulas, as described previously (31). The average of two measurements was calculated; two values were within an SD of ≤ 10% (23). The results demonstrated that the right and left baPWV values were identical in both groups (r = 0.90 and r = 0.97 in the normal-weight and overweight/obese individuals, respectively). Therefore, the right baPWV is reported in this study.
3.2.2. Heart Rate and Blood Pressure
The heart rate (HR) and blood pressure (BP) were measured using an automated non-invasive vascular screening device (VP-1000 plus Omron Corporation). For BP, a minimum of two measurements were taken for each participant, and the two values had to not differ by more than 5 mmHg (21). Moreover, the mean brachial pressure (MAP) and pulse pressure (PP) were also examined and reported.
The HR was recorded throughout the exercise using a Polar H10 HR sensor (Polar Electro Oy Inc., Kempele, Finland). The age-predicted maximal HR was calculated using Tanaka’s formula (32).
3.2.3. REHIT
Reduced-exertion high-intensity interval training is a 10-minute exercise, which starts with 2 minutes of warm-up (unloaded pedaling), followed by 2 all-out 20-second sprints with a breaking force equivalent to 7.5% of the body mass interspersed by a recovery period after the first sprint (unloaded pedaling) and 4 minutes of cool-down (unloaded pedaling) after the second sprint. The rating of perceived exertion (RPE) and affect responses were determined using the Borg scale (Thai version) (33) and the feeling scale (34), respectively, before and after REHIT.
3.3. Statistical Analysis
The normal distribution of data was tested using the Shapiro-Wilk test. Results are presented as the mean ± SD. The differences in baseline characteristics between the two groups were tested using the Mann-Whitney U test and independent t-test. Two-way repeated ANOVA (groups (normal-weight vs. overweight/obese) by time (pre-, post-1 min, post-30 min, and post-60 min exercise)) were used to determine differences in response to exercise. Statistical significance was set at P ≤ 0.05.
4. Results
4.1. Baseline Measurements
The participants’ basic characteristics are listed in Table 1. There was a significant difference in weight and BMI between the two groups (P < 0.05).
4.2. Cardiovascular Variables
All exercise sessions were generally safe and well-tolerated, both in normal-weight and overweight/obese participants. The mean peak HR during REHIT in the normal-weight and overweight/obese groups was 90.2 ± 5.8 and 90.2 ± 3.3%, respectively.
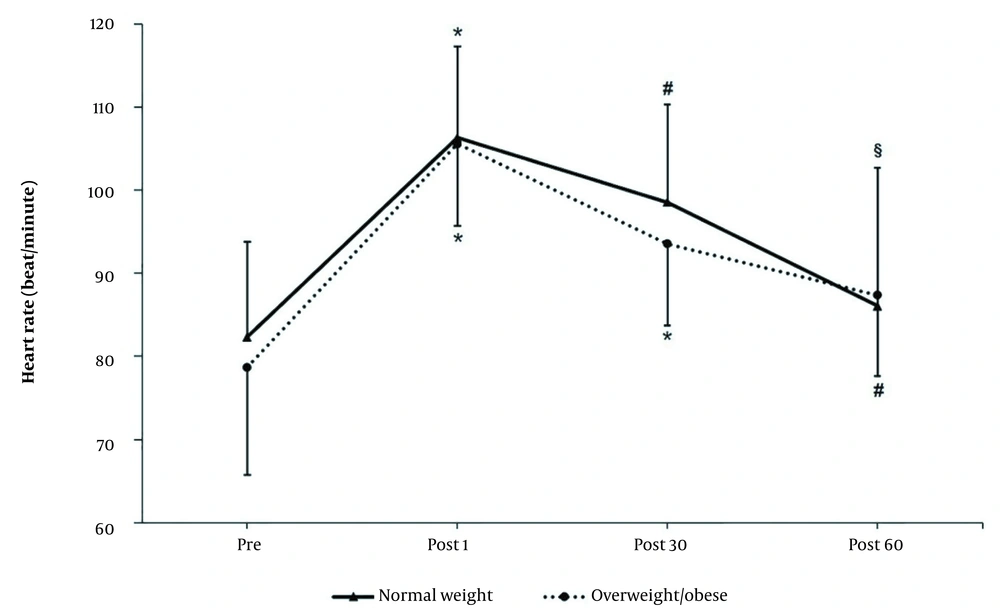
There was a significant increase in the HR after REHIT (post-1 and post-30) (P < 0.05), which then returned to baseline 60 min after REHIT in both groups (Figure 1). However, the HR did not differ between the normal-weight and overweight/obese groups.
Heart rate at baseline and at discrete time points after reduced-exertion high-intensity interval training (REHIT). * P < 0.05 significantly different compared to pre; # P < 0.05 significantly different compared to post-1; § P < 0.05 significantly different compared to post-30. Data are presented as mean ± SD.
Blood pressure values are presented in Table 2. There were no significant differences in the BP between the two groups. After REHIT for 1 min, the diastolic blood pressure (DBP) lowered significantly in both groups (P < 0.05); however, the MAP was significantly lower in the normal-weight group (P < 0.05). Moreover, the PP was significantly higher in both groups compared to that at baseline (P < 0.05). There was a significant decrease in the systolic blood pressure (SBP) and DBP from baseline in both groups after 30 min of REHIT (P < 0.05). After 60 min of REHIT, all cardiovascular parameters returned to the baseline values, except that the SBP decreased significantly (P < 0.05).
| Parameters (mmHg) | Post | |||
|---|---|---|---|---|
| Baseline | 1 min | 30 min | 60 min | |
| SBP | ||||
| Normal-weight | 113.2 ± 9.1 | 111.0 ± 10.8 | 108.5 ± 8.4 b | 107.1 ± 8.4 b |
| Overweight/obese | 117.4 ± 8.6 | 115.9 ± 8.7 | 111.4 ± 8.5 b, c | 110.8 ± 7.3 b, c |
| DBP | ||||
| Normal-weight | 67.8 ± 7.0 | 61.0 ± 7.6 b | 62.3 ± 5.9 b | 62.8 ± 7.6 |
| Overweight/obese | 68.4 ± 6.0 | 61.7 ± 6.2 b | 63.3 ± 6.4 b | 65.8 ± 7.9 |
| MAP | ||||
| Normal-weight | 85.0 ± 7.1 | 81.0 ± 8.4 b | 80.8 ± 8.5 | 81.9 ± 6.7 |
| Overweight/obese | 87.0 ± 7.3 | 83.7 ± 6.7 | 83.1 ± 7.3 | 83.3 ± 7.5 |
| PP | ||||
| Normal-weight | 45.5 ± 5.0 | 50.1 ± 4.6 b | 46.3 ± 4.1 c | 44.3 ± 4.7 c |
| Overweight/obese | 49.1 ± 5.8 | 54.5 ± 4.8 b | 49.5 ± 4.9 c | 46.7 ± 4.3 c |
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure.
a Data are presented as the mean ± SD.
b P < 0.05, significantly different from baseline.
c P < 0.05, significantly different from post-1.
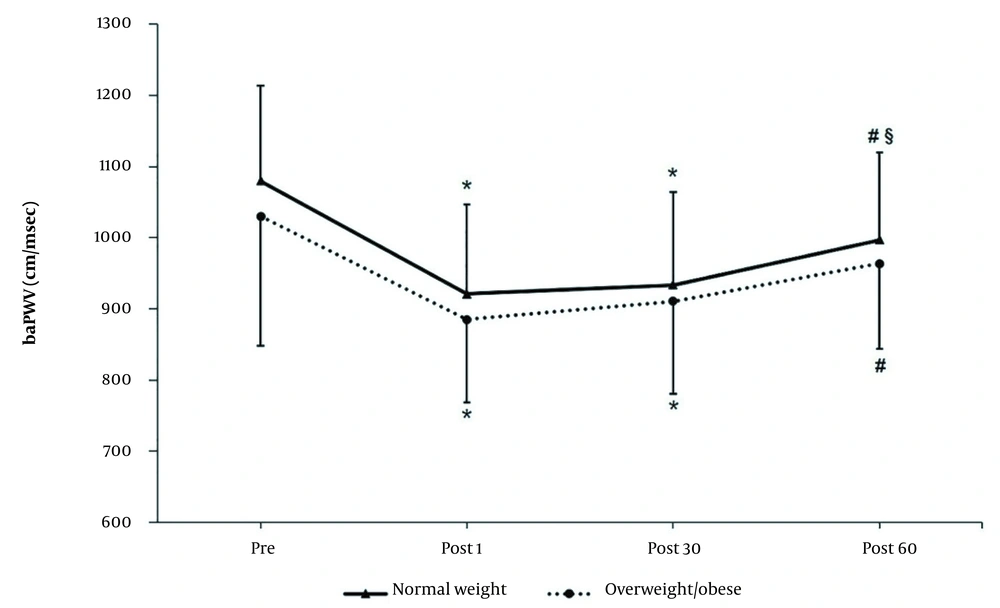
4.3. AS
There was no significant group × time interaction effect for the baPWV. The baPWV reduced significantly following REHIT and returned to baseline at 60 min in both groups (effect of time, P < 0.001) (Figure 2).
Brachial-ankle pulse wave velocity at baseline and at discrete time points after reduced-exertion high-intensity interval training (REHIT). * P <0.05 significantly different compared to pre; # P < 0.05 significantly different compared to post-1; § P < 0.05 significantly different compared to post-30. Data are presented as mean ± SD.
4.4. RPE and Affect Responses
There were no significant differences in the RPE and affected responses between the groups. The average RPE increased significantly following REHIT in both groups (P < 0.05). The average RPE following REHIT was around 15 and 14 in the normal-weight and overweight/obese individuals, respectively). However, the affect responses did not change following REHIT (Table 3).
Abbreviation: RPE, rating of perceived exertion.
a Data are presented as the mean ± SD.
b P < 0.05, significantly different from baseline.
5. Discussion
The key findings of this study were that the baPWV decreased following REHIT in both groups, i.e., the normal-weight and overweight/obese with insufficient physical activity. Furthermore, the groups had no significant difference in any of the cardiovascular parameters, RPE, or affect responses.
5.1. AS and Hemodynamic Parameters at Rest
Several studies have shown that AS increases at rest in obese individuals (21, 25, 35). These findings differ from those of the current study, which demonstrated that overweight/obese individuals did not show a difference in baseline AS and hemodynamic parameters compared to those in normal-weight participants. This could be explained by the fact that there are several factors that influence AS apart from the BMI, such as waist-to-hip ratio and visceral fat area (36). Future studies should focus on examining the waist-to-hip ratio or visceral fat area to classify obesity.
There was no significant difference in baseline hemodynamic parameters between the two groups. This finding contrasts with the data from the study by Bunsawat et al., which revealed that the baseline DBP and MAP were higher among obese individuals than among normal-weight individuals (21). A possible explanation could be that the duration for which the individuals have been overweight is a factor that affects the BP in obese individuals (37). The participants in this study may not have been overweight/obese for long enough to allow their obesity to affect their BP,
5.2. AS and Hemodynamic Parameters Following REHIT
A single bout of REHIT can acutely reduce AS and return to baseline at 60 min. These results are consistent with those from the previous studies. Chuensiri et al. reported a decrease in AS following a single bout of 8 × 20 s high-intensity cycling exercise at 130% and 170% VO2 peak; however, AS did not change after cycling at 100% VO2 peak in obese prepubescent boys (25). Moreover, Hortmann et al. demonstrated that AS did not increase acutely following a cycle HIIT (4 × 4 min at 85 - 95% of maximal HR) in young obese women (24). Additionally, aortic stiffness did not increase significantly following repeated high-intensity interval cycling exercise (3 × 30 s all-out sprint) (23). However, few studies have demonstrated that sprint interval exercise acutely increases central artery stiffness (20, 38, 39). The mechanisms underlying acute REHIT-induced decrease in AS remain unclear. Physiological adaptations following acute exercise bouts include increased blood flow and shear stress, which increase nitric oxide synthase (NOS) activity (40, 41). Moreover, high-intensity exercise could stimulate higher shear stress (25). Hasegawa et al. demonstrated that HIIT could increase nitric oxide (NO) bioavailability by upregulating the endothelial nitric oxide synthase (eNOS) signaling pathway, leading to reduced AS (42).
In this study, REHIT increased the HR after exercise for 1 and 30 min, and the HR then returned to baseline after 60 min. These results are supported by those of Hortmann et al. and Kingsley et al., who demonstrated that the HR increased following HIIT in obese (24) and normal-weight individuals (23). However, the results from the study by Hortmann et al. (24) showed that the HR did not return to baseline after 60 min of 4 × 4 min of HIIT. Based on these observations, it can be assumed that a longer high-intensity duration in the HIIT protocol may influence HR recovery. This highlights the fact that HR can recover after 60 min of REHIT in individuals with insufficient physical activity.
The SBP was reduced following REHIT for 30 and 60 min in both groups. This finding is consistent with data from the study by Dantas et al., which showed that repeated high-intensity interval cycling exercise reduced the SBP in the first 5 hours post-exercise (43). The DBP was reduced following REHIT at 1 min and 30 min and returned to baseline after 60 min in both groups. This result is supported by the results obtained by Morales-Palomo et al., who demonstrated that the DBP was reduced post-HIIT in healthy participants (44). This is consistent with prior literature demonstrating the beneficial effects of REHIT as it shows that REHIT transiently reduces the BP in normal-weight and overweight/obese individuals with insufficient activity. The possible mechanisms underlying post-single-bout REHIT hypotension remain unclear. Chen and Bonham suggested that the central baroreflex network plays an important role in post-exercise hypotension (45). Moreover, a decrease in sympathetic nerve activation combined with the release of local vasodilator substances reduced the BP following exercise (46).
5.3. RPE and Affect
Measuring the mean RPE after REHIT corresponded to hard in both groups. This finding is supported by the findings obtained by Nalcakan et al., who demonstrated that the post-exercise RPE averaged between ~13 and 15 (‘somewhat hard’ to ‘hard’) (47). Even the current study assessed the RPE only once following the first session of REHIT. Previous studies suggest that the score does not differ when assessing the 18th (47) or 24th (11) sessions of REHIT. Moreover, this study revealed a very low negative affective valence response following acute REHIT with a normal weight. Songsorn et al. showed that the affective response decreased following an acute REHIT session and then improved following exercise training (48). Importantly, the RPE and affect response are associated with the overall perception of an exercise experience by an individual (49). Considered together, these findings support the fact that REHIT may be adopted by normal-weight or overweight/obese sedentary individuals.
5.4. Limitations
A few limitations of this study must be considered before interpreting the findings. First, the recovery duration for this study was 60 min and, therefore, may not allow detection of the time it would take for the SBP to return to baseline. Second, the primary purpose of this study was to investigate the acute effects of REHIT on AS. Further research on the training effect of REHIT on vascular health markers should be conducted.
5.5. Conclusions
A single bout of REHIT cannot induce a transient increase in AS. However, it can help reduce AS and BP in normal-weight and overweight/obese individuals. The findings from this study suggest that REHIT is safe and expand upon the findings from previous studies demonstrating the beneficial effect of REHIT by improving markers of vascular health following a single bout of exercise.