Dear Editor,
Androgenic-anabolic steroids (AAS) are a subset of testosterone. They are widely used by athletes and, specifically, bodybuilders to improve strength and performance (1). They are classified based on their chemical structures and have a variety of side effects that impact different organs, especially the cardiovascular system, liver, and kidney (2). Skin changes, such as acne, striae, hirsutism, and alopecia, are common side effects of AAS abuse. They can even lead to other complications, such as shrinking testicles, breast enlargement, hair loss, and a decrease in the number of sperm and infertility in males (3). Studies have shown that AAS can be a risk factor in human cancers, such as prostate cancer, and this might be the result of the effect on cellular changes associated with high-density lipoprotein (HDL) and positive effects on muscle lean mass and strength (4). Undeniable connections between steroid abuse among bodybuilders and their side effects necessitate the need for further investigations.
The number of AAS users represents a steady growth trend in the Middle East (5). However, it should be noted that there is a lack of research on this topic not only among the Asian population but also among Western athletes, especially related to unknown side effects, such as lipoma.
Lipomas are benign neoplasms of fat cells that can be confused with liposarcomas or even rarely change to them (6). Therefore, it is crucial to differentiate them, as the first one might be benign; nevertheless, the second could be pernicious. Solitary lipomas might have chromosome rearrangements; however, it is not common in multiple ones (6).
Lipoma has not been reported as a side effect of steroids. Nevertheless, as they can alter the mesenchymal tissue and hormonal changes, they should be noted. Therefore, it seems rational to consider AAS as a risk factor for lipomas in high-dose consumption by athletes (7) due to increasing fat cell proliferation in addition to the fascia in situations where the individual uses AAS.
This report describes the medical history of an elite bodybuilder with lipoma who abused steroids for 7 years. Once an endocrinologist recognized the lipomas, they were surgically removed. The patient was a 33-year-old male elite bodybuilder with a 7-year history of steroid abuse. The individual used different types of anabolic steroids, such as Sustanon, nandrolone, stanozolol, and Primobolan, from 18 until 25 years in a combination of a linear pattern two times (each time 1 mL) per week for 6 weeks. The case injected the steroids in muscular areas, such as the deltoid, pectoral, quadriceps, and gastrocnemius, and used human chorionic gonadotropin (hCG 5000 IU) between the periods (at the end of the third week) and 30 days after the last injection in order to prevent gynecomastia, which is a side effect of steroids. The case also used tamoxifen (Nolvadex) orally (20 mg) during the periods (every night before sleep) until 10 days after finishing the steroids. There was no history of alcohol consumption, tobacco smoking, and family history of any type of tumor.
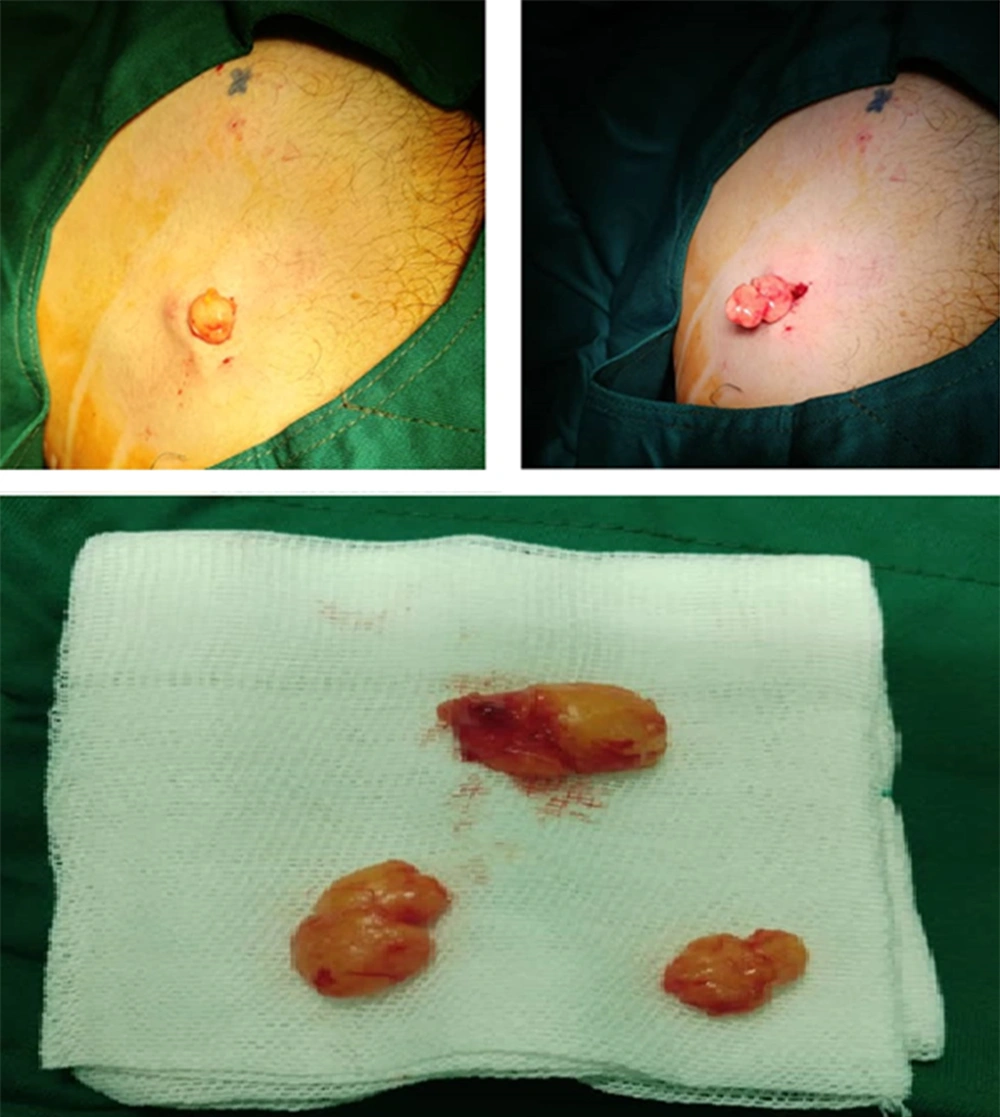
The case stopped using steroids at 25 years after masses began to appear in his body without any specific distributional pattern and in areas remote from the injection sites. The masses were painless, the laboratory data were normal, and the endocrinologist diagnosed them as lipomas by physical examination. After 5 years, the masses started to increase in size and become more in number, superficial, and painful, and the patient had them surgically removed (Figure 1).
The retention of nitrogen in the body is considered the primary mechanism of action of AAS. In men, steroid use interferes with the hypothalamic-pituitary-testicular axis, and sudden discontinuation of AAS after prolonged use can cause hypogonadal activity (8). Hepatotoxicity and hepatic neoplasms can result from active oral AAS (9). Hypertrophy in the prostate with an increased risk of prostate cancer is considered another consequence of prolonged AAS use (10). Being a derivative of testosterone enables AAS to change the structure of the cells by attaching their receptors to the nucleus of the cell and affecting protein synthesis (11).
As the individual in our case used a variety of different types of steroids, hCG, and tamoxifen, we cannot be sure that the lipoma was a direct result of the steroids as they are prohibited drugs and are included in doping control list and elite athletes would be penalized for reporting side effects.
In this case, the importance of identifying the lipomas was the differentiation from liposarcomas and the concern about conversion to them (6). As this side effect has not yet been proven, it is suggested that athletes who use anabolic steroids pay special attention to side effects, especially skin disorders that might be at risk of progressing to malignancy and the need for urgent treatment.