1. Introduction
Cyclops lesions or arthrofibrotic nodules of the knee, first described by Jackson and Schaefer, occur in the anterior aspect along the graft after an anterior cruciate ligament reconstruction of the intercondylar notch (1-3). Arthroscopically, they appear as head-like fibrous lesions with reddish-blue areas of discoloration and consist of a pedunculated nodule of fibrovascular proliferative tissue, with or without bone or cartilaginous tissue (3, 4). Those lesions can cause pain, loss of full extension, and locking or discomfort of the knee with or without a palpable clunk (4, 5). Cyclops lesions are usually found after anterior cruciate ligament (ACL) reconstruction or injury (4) or as localized nodules of pigmented villonodular synovitis (PVNS) (5, 6). The reported incidence of Cyclops syndrome is between 1% and 10% of all ACL reconstructions (1, 3, 4), whereas magnetic resonance imaging (MRI) studies have reported a Cyclops lesion incidence of 25% to 47% (4). Furthermore, atypical lesions or variants have also been reported, including chronic synovitis lesions with multinucleated giant cells or gouty tophus lesions (7). However, previous reports were associated with ACL reconstruction or injury (4), and only one case report described a cyclops lesion after posterior cruciate ligament (PCL) repair (8). Thus, we present a novel case of cyclops lesion from a minor PCL injury without laxity or previous surgery. In this case, you can consider the differential diagnosis of Cyclops syndrome when patients present with mechanical symptoms, such as loss of extension, locking, and discomfort during extension.
2. Case Presentation
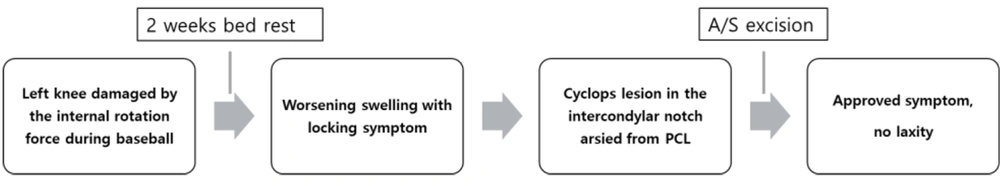
A 37-year-old man without major abnormalities or previous trauma in his knees visited the outpatient clinic complaining of mild knee pain, intermittent locking, and extension discomfort after hard work or occasional exercise. These symptoms started 3 weeks earlier, during his usual baseball activity. He reported feeling a shock in his left knee from an internal rotation force while sliding to a base and standing up. Mild knee pain occurred immediately after the injury; concluding that this was a simple sprain, he took bed rest and did not seek clinical examination or treatment (Figure 1). However, the knee pain and swelling worsened, with occasional locking symptoms and extension discomfort. The initial simple radiograph showed no specific findings, and there was also no laxity. A slight decrease in extension (around 5° of flexion contracture) was observed, but the knee could be fully extended during passive extension. Then, we checked the MRI to find other reasons.
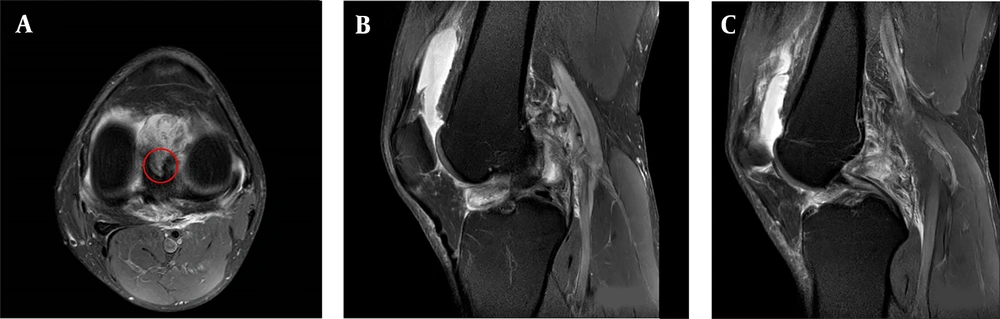
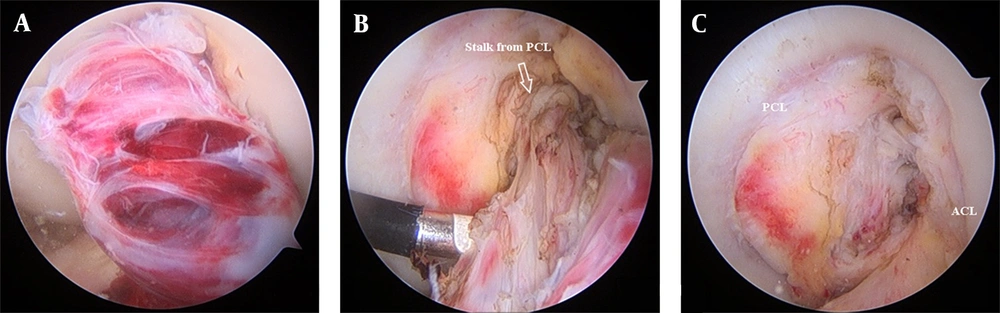
MRI of the left knee (Figure 2A and B) showed an intact ACL but partially injured PCL, small suprapatellar effusion, and a cyclops lesion (2.4 × 3.4 × 2.5 cm) in the intercondylar notch of the femur, which originated from the PCL. The cyclops lesion showed heterogeneous high signal intensity with internal irregular low signal intensity portions on T2-weighted fat-suppression and proton density images. A lesion with diffuse thinning with increased T2 signal intensity was observed in the proximal half of the PCL, consistent with a low-grade partial tear of the PCL (Figure 2C). No other pathologies, including that of the meniscus, were identified that could have induced the locking symptoms. During arthroscopy, a cyclops lesion originating from the PCL was confirmed and excised (Figure 3A-C).
(A) The axial image of the proton density fat-suppression series shows a mass with heterogeneous high signal intensity, portions with internal irregular low signal intensity, and a stalk originating from the PCL (red circle). (B) Sagittal image of the T2-weighted fat-suppression series showing an ill-defined tubular lesion at an intercondylar notch connected to the PCL. (C) A diffuse thinning with increased T2 signal intensity of the proximal portion of the PCL, consistent with partial PCL rupture. PCL, posterior cruciate ligament.
The gross appearance of the excised cyclops lesion was consistent with the collection of irregularly sized blood vessels with central cystic changes. (Figure 4A) The microscopic findings of this lesion included dilated and congested blood vessels of irregular-sized veins and hemorrhagic necrosis within the wavy ligament tissues, which confirmed its origin from the ligament tissue (Figure 4B and C). After arthroscopic surgery, the patient’s symptoms were relieved immediately, and no knee joint laxity with full range of motion was found after surgery at a 6-week outpatient clinic follow-up.
(A) The excised mass measuring 3.1 × 1.9 cm is attached to the ligament. The cut surface of the mass shows the collection of irregularly sized blood vessels with central cystic changes and synovium. (B) Microscopic findings consisting of dilated and congested blood vessels of irregularly sized veins, with some showing organized thrombi with or without hemorrhagic rupture (×100, hematoxylin and eosin [H&E]). (C) Masson trichrome stain shows thrombosed veins and hemorrhagic necrosis within the wavy ligament tissues. (×40, Masson trichrome stain (MT)).
3. Discussion
Cyclops lesions are diagnosed based on clinical symptoms and MRI findings. Patients complain of pain, loss of extension, and painful terminal extension during walking or running (4, 5, 7). Those lesions usually occur after knee arthroscopic surgery, such as ACL reconstruction, but are also caused by injuries to the native ACL, scar tissue, synovitis, and granulation tissue after microtrauma (1, 2, 4, 7). Although rare, tumour-like lesions can also cause mechanical problems such as localized PVNS or gouty tophus (2, 5, 7). The treatment of choice is 4arthroscopic removal of the symptomatic nodule.
MRI is the current tool of choice for the differential diagnosis of cyclops lesions. The localized form of PVNS on MRI is characterized by a focal involvement of the synovium with nodules of pathologic tissue and local warmth, swelling, and stiffness (5, 6). Localized PVNS lesions usually have heterogeneous signal intensity depending on their hemosiderin content and are characterized by decreased intensity on both T1-weighted and T2-weighted images (9) The MRI appearance of tophi is usually of nonspecific low to intermediate signal intensity on both TI- and T2-weighted images and a variable enhancement pattern in the synovium (7). Cyclops lesions occur in 1% to 9.8% of patients with extension loss after ACL reconstruction, for which MRI is also the imaging modality of choice (3, 4). The present study also performed an MRI to evaluate the pathology of the knee; the findings showed a heterogeneous nodule on all sequences with a hypointense rim originating from the PCL with evidence of PCL signal change. This MRI finding led to a clinical suspicion of a Cyclops lesion from the PCL due to acute trauma before surgery, which has not been reported previously.
The pathogenesis of cyclops lesions is multifactorial. Jackson et al. reported that debris raised by drilling of the tibial tunnel or broken graft fibers could lead to a cyclops lesion (3). Another theory suggests that the cause is reparative processes occurring as a reaction of the remaining living tissue, which explains Cyclops syndrome in partial or total ACL tears before surgery (4). However, Marzo et al. suggested that microtrauma due to ventral impingement of the graft and ventral fiber breakage might form a fibrous nodule (10). Although the cyclops lesion in this study did not originate from the ACL, acute trauma of the PCL fiber might form a fibrous nodule through the reparative processes; thus, the patient’s symptoms worsened over time. Histologically, this lesion was characterized by dilated and congested blood vessels of irregular-sized veins with or without hemorrhagic rupture from the synovium and wavy ligamentary tissues connected to the PCL. Thus, this finding confirmed that an acutely injured PCL fiber might form a reparative fibrous nodule. The pathogenesis and treatment of this Cyclops lesion might not differ from those of the ACL; however, this case was unique because no other case report has described a Cyclops lesion following a PCL injury without surgery. After arthroscopic excision, the patient’s symptoms were relieved without laxity, similar to the experience with removal of lesions from the ACL (4).
This study is a case report, so there are several limitations. Firstly, it is difficult to represent the general population with locking symptoms. However, since the main objective of this study is to present special cases with discriminative diagnoses in situations with knee pain or locking symptoms, it does not pose a significant constraint. Secondly, further study is needed as this is the first reported case. For instance, it has been suggested that the excision of cyclops lesions in the ACL could impact knee instability. Therefore, if additional PCL cyclops lesions accumulate, further research is needed to investigate knee instability following cyclops lesion excision.
Mechanical symptoms, including extension loss, locking, and discomfort during extension, are associated with many intra-articular pathologies, such as meniscus injury, cyclops lesions, tophi, and benign masses. While most of these lesions can be treated efficiently by arthroscopy, the differential diagnosis should be performed for unique cases with a lesion from minor PCL injury without laxity or previous surgery.
![(A) The excised mass measuring 3.1 × 1.9 cm is attached to the ligament. The cut surface of the mass shows the collection of irregularly sized blood vessels with central cystic changes and synovium. (B) Microscopic findings consisting of dilated and congested blood vessels of irregularly sized veins, with some showing organized thrombi with or without hemorrhagic rupture (×100, hematoxylin and eosin [H&E]). (C) Masson trichrome stain shows thrombosed veins and hemorrhagic necrosis within the wavy ligament tissues. (×40, Masson trichrome stain (MT)). (A) The excised mass measuring 3.1 × 1.9 cm is attached to the ligament. The cut surface of the mass shows the collection of irregularly sized blood vessels with central cystic changes and synovium. (B) Microscopic findings consisting of dilated and congested blood vessels of irregularly sized veins, with some showing organized thrombi with or without hemorrhagic rupture (×100, hematoxylin and eosin [H&E]). (C) Masson trichrome stain shows thrombosed veins and hemorrhagic necrosis within the wavy ligament tissues. (×40, Masson trichrome stain (MT)).](https://services.brieflands.com/cdn/serve/3170b/3240359e1c7575300d8a1cdc924a9928699693b2/asjsm-136107-g003-F4-preview.webp)